81
Congenital Radioulnar Synostosis
Allan E. Peljovich and Peter M. Waters
History and Clinical Presentation
An otherwise healthy 19-month-old girl presented because her parents noticed that she was unable to eat with her left hand, and had difficulties with her right. Her mother’s pregnancy was remarkable only for a cesarean section delivery 6 weeks preterm. She was noticed at birth to have bilateral inguinal hernias, both of which had since been repaired. Although she has been low in her percentiles for both height and weight, her development has been normal. Her mother is not sure which hand is her dominant one, but she seems to rely more on her left.
Physical Examination
Her complete musculoskeletal examination was unremarkable with the exception of her upper extremities. Her left elbow lacked ∼10 degrees of extension. This elbow was fixed in ∼90 degrees of pronation. The left wrist was rather supple and gave her 60 degrees of pronation and supination through the carpus. Her right elbow flexed and extended fully, and was held in ∼45 degrees of pronation. Unlike in the left arm, there was a minor degree of forearm pronation and supination in the right arm. The right wrist was equally supple to the left.
Diagnostics Studies
Anteroposterior (AP) and lateral radiographs were available for both forearms/elbows (Fig. 81–1). She had a complete proximal bony synostosis of the left proximal radius and ulna. The synostosis involved the entire aspect of the proximal forearm, including the radial head and the proximal radioulnar joint. The radial head was posterior to the capitellum. There was a partial synostosis proximally of the right forearm with evidence of a foreshortened, and posteriorly dislocated radial head.

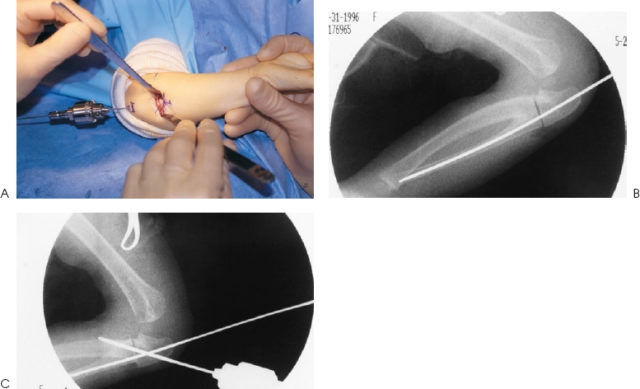
Figure 81–1 Initial radiographs. Anteroposterior (AP) film of the left forearm (the operative side).
Differential Diagnosis
Chronic brachial plexus birth palsy
Spastic contracture as found in cerebral palsy
Acute and chronic traumatic injuries, including “nursemaid’s elbow,” and Monteggia fracture-dislocations
The presence of an osseous synostosis confirms the diagnosis. Other etiologies for the clinical finding of a stiff pronated forearm in children include:
PEARLS
- Using biplanar radiographs, be sure that the smooth longitudinal pin is heading down the intramedullary canal of the ulna.
- Use careful and deliberate subperiosteal dissection of the synostosis mass.
- Perform prophylactic forearm fasciotomies.
PITFALLS
- Be aware of the patient’s forearm position relative to the position of the upper extremity to determine the appropriate amount of corrective rotation.
- Monitor the patient postoperatively for a compartment syndrome. Increasing analgesic requirement is a key diagnostic factor in pediatric patients with compartment syndrome.
Diagnosis
Bilateral Congenital Radioulnar Synostosis
Radioulnar synostosis can present as a congenital deformity, as the result of forearm trauma including surgical trauma, and as a sequela to global trauma such as head injuries and burns. As a congenital deformity, radioulnar synostosis is thought to represent a failure of longitudinal segmentation. For a portion of the elbow’s in utero development, the proximal ulna and radius share a common perichondrium. Normal segmentation results in the development of separate ulnohumeral, radiocapitellar, and proximal radioulnar joints. Failure of this process is thought to result in the persistence of bridging tissue, which can remain fibrous or ossify. The extent of the synostosis also depends on the extent to which the process of segmentation fails. In some cases, the radial head is involved, in others it is a separate structure with the synostosis occurring just distal. In these latter cases, many authors have noted associated anomalies of the radial head and the radiocapitellar joint including radial head dislocation. The forearm is typically pronated, as this is the usual position of the upper extremity at the point of longitudinal segmentation of the radius and ulna in utero. Our patient presented with bilateral synostoses that were different: one osseous, one fibrous, one with radial head/radiocapitellar joint anomaly, and both pronated.
As with our case, most patients do not present until later in infancy. In one study the average age of diagnosis was ∼6 years. This is due, in part, to the ability of the children to adapt to their fixed forearm position through a mobile shoulder joint, as well as a hypermobile wrist. To supinate a forearm that is being held in pronation, the shoulder joint must adduct and externally rotate. The greater the degree of forearm pronation, the more difficult it becomes to supinate the wrist. Many patients with mild degrees of pronation can easily adapt. With increasing degrees of pronation, however, children find it increasingly difficult, if not impossible, to simply perform many activities of daily living that require forearm supination. These activities include eating, reaching about the face and head, dressing, and play/recreational activities. These tasks become increasingly difficult if both forearms are involved.
Although many feel that pronation greater than 45 to 60 degrees will be functionally limiting, one study found no association between the degree of pronation and disability. Surgery is recommended when the degree of pronation clearly interferes with the child’s ability to use the extremity. “Back handing” by hyperpronation to simulate a supinated position is often an indication of limitation.
At presentation, careful examination reveals that the forearm is held in a degree of pronation. This is not always easy to detect upon casual inspection. Therefore, it is important for the examiner to stabilize the elbow and the wrist when checking for the integrity of forearm rotation. It is important to distinguish between rotation that occurs through the forearm axis and that which occurs through the wrist, because wrist hypermobility is a common finding in congenital radioulnar synostosis. One common finding that was present in our case was a small elbow flexion contracture. Plain films will support the diagnosis once the bridge becomes ossified; however, one must be mindful of the possibility of a fibrous bridge. It is important to note the status of the radiocapitellar joint. One author recommends radial head excision if dislocated and problematic once a child reaches skeletal maturity.
Once surgery is indicated, our approach is based on the idea that children will have nearly normal upper extremity function as long as the forearms are in a more functional position of rotation. Supple shoulders and hypermobile wrists allow these children to adapt. As such, we do not perform procedures designed to restore rotation to the forearm. We also recommend surgery at an early age because some feel that the risk of neurovascular complication increases after 10 years of age. Our procedure is a modification of that originally described by Green. Simmons et al described a significant incidence of neurovascular complications with rotational osteotomies. Their recommendation was to limit the degree of correction at a single surgery, or shorten the forearm, to prevent such complications. The senior author has found that prophylactic forearm fasciotomies have thus far eliminated the occurrence of compartment syndrome in our patients. This approach is both reliable and technically straightforward while minimizing potential complications and untoward outcomes.
Surgical Management
Requirements
- Smooth Kirschner wire (K wire) or steinman pin: ∼3/32 inch, depending on age
- Smooth K or C wire: ∼0.062 inch depending on age
- Sagittal saw
- Osteotomes
- Fluoroscopy
Technique
The procedure is performed with the patient in the supine position and under general anesthesia on a radiolucent hand table. The entire arm is prepped and draped after placement of a nonsterile tourniquet. Appropriate preoperative intravenous antibiotics are administered for infectious prophylaxis, and the procedure is started once the arm is exsanguinated and the tourniquet elevated.
The next step is to expose the synostosis site (Fig. 81–2A). A 5- to 6-cm longitudinal incision is created along the proximal subcutaneous ulnar border. Fluoroscopic assistance can guide the exact positioning of the wound so it is centered over the synostotic mass. The incision is carefully taken down to the level of bone, and the periosteum is sharply incised for the length of the skin incision. No neurovascular tissue of significance is encountered in this exposure other than crossing veins, which can be ligated or coagulated. The dissection then proceeds subperiosteally radially, ulnarly, and volarly for the entire extent of the synostotic mass. We have often found that there is a bony crevice at the level of the synostosis. Awareness of this crevice prevents accidental penetration into the soft tissues surrounding the proximal forearm. Fluoroscopic assistance prevents accidental penetration of the elbow joint. Once this dissection is complete, Hohmann-type retractors can be used to aid in exposure. The surgeon must be mindful of the important volar neurovascular structures as well as the posterior interosseous nerve.