Computer-Assisted ACL Reconstruction
Stefano Zaffagnini
Simone Bignozzi
Nicola Lopomo
Danilo Bruni
Giulio Marcheggiani
Alessandro Russo
Maurilo Marcacci
COMPUTER-ASSISTED ACL RECONSTRUCTION: RATIONALE
In the 19th century, Lord Kelvin Thompson stated, “I often say that when you can measure what you are speaking about, and express it in numbers, you know something about it; but when you cannot measure it, when you cannot express it in numbers, your knowledge is of a meagre and unsatisfactory kind” (63), which can be summarized in “If it can be measured, it can be improved.” This philosophy fully adapts to the concept of computer-assisted surgery (CAS). With the help of this technology, in the last years, the knowledge about anatomy and kinematics of the anterior cruciate ligament (ACL) has improved dramatically.
CAS in ACL reconstruction has now reached 15 years of research. First publications started in the second half of the 1990s (62). The main goal of the navigated procedures was to improve the correct position of the graft, using anatomical references and graft isometry during the range of motion, considering that 70% to 80% of the complications were due to malpositioned tunnels (16).
The purpose of these first systems was to augment the information given to the surgeon, in order to better identify the anatomical landmarks that were difficult to be recognized in an arthroscopic setup. The efficacy of these enhanced information given by computer-based ACL reconstruction was evaluated in the clinical use by Dessenne et al. (1,16) who demonstrated the feasibility of navigation in routine clinical setup. In addition, Klos et al. (28) in 1998 concluded that simple visual enhancements were useful to improve the repeatability of arthroscopic ACL reconstruction using radiographic tunnel position measurements as a comparison.
These studies, however, did not increase the interest of the orthopaedic community in this field for several years. The reason for this scarce interest in navigation was probably due to the unclear goal in tunnel placement and orientation during the ACL reconstruction. Also the isometry concept has been shown to be insufficient and the correct positioning of graft insertions is still a matter of debate (11,17,41,57,59). In addition, the costs and the time-consuming problems related to the use of this device were the major obstacles to the wide spreading in clinical practice.
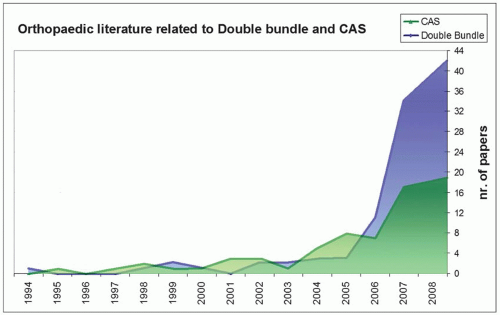
More recently, thanks to more surgeon-friendly systems and to the evolution of software for computer-based ACL surgery, there has been an increased interest in this field. This development includes the possibility to perform stability testing, including rotational and translational measurements, or decomposition of complex clinical test such as pivot shift (6), allowing to better evaluate the effect of different surgical procedures to the stability of the knee and to better describe patients’ specific laxity (46). The augmented performance of navigation systems allows to use this methodology to assess the performance of new and more complex reconstructive surgical techniques, such as double bundle. In fact, starting from 2005, there has been a big number of articles on navigated ACL and on anatomical double-bundle reconstruction techniques (Fig. 33.1).
The possibility to better understand and describe different surgeries and to characterize patients’ specific laxity has moved the trend of navigation to a new concept: the “on demand” surgery, where kinematics and anatomy can be compared to a database of different surgical workflow, in order to better address the pathology for the specific patients.
At present, instrumental evaluation during surgery, with the use of navigation systems, remains the more accurate procedure; therefore, several clinical studies have evaluated the effect of different surgical techniques to joint kinematics at time zero.
NAVIGATION TYPES
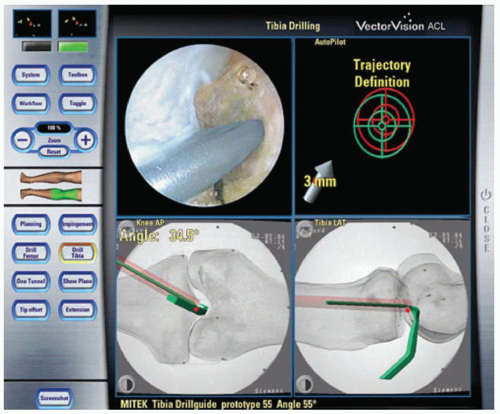
There are two types of navigation systems used clinically. Image-based systems that utilize anatomical data derived from different imaging methods, such as computer tomography (e.g., Navitrack [Orthosoft, Montreal, Canada]), intraoperative fluoroscopy (e.g., Vector Vision [BrainLAB, Muenchen, Germany], Fig. 33.2), or standard x-rays (e.g., SurgiGATE [Medvision Houston, Texas]).
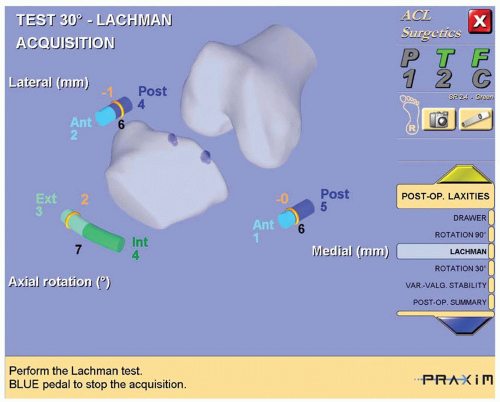
Image-free systems rely on the acquisition of anatomical references during surgery and require no preoperative imaging. The anatomical data registration allows to create the virtual bone model of the patient. Most of the image-free systems are based on bone morphing (e.g., Praxim [Medvision, La Tronche, France], Fig. 33.3), which requires large numbers of data points to match the individual knee morphology to be modeled, increasing surgical times.
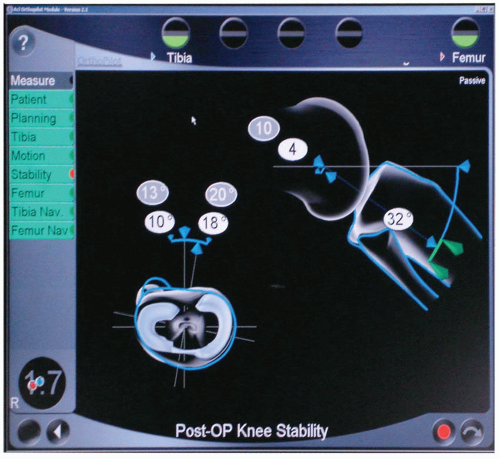
Some systems do not perform bone morphing (e.g., Orthopilot [Aesculap, Tuttlingen, Germany], Fig. 33.4) and BLU-IGS, [Orthokey, Lewes, Delaware], Fig. 33.11). The registration is used to define bones’ reference systems and reference points used for surgical planning or by kinematic acquisitions. Limb position and orientation are shown in Figure 33.4 with image templates that are derived from the acquired data.
Hardware for tracking the surgical scenario also differs. There are mainly two types of systems: optoelectronic and electromagnetic. Most of optoelectronic systems utilize sterilizable markers that reflect the infrared light emitted by the cameras. These markers do not require power supply but are generally disposable, increasing the cost for single surgery.
Electromagnetic systems use a receiver to track the position of transmitters mounted on the bones. This technology has the advantage of not suffering from the “line of sight” problems, causing potential problems in the setup of the operative room. The critical point of electromagnetic technology, at present, consists in magnetic interferences caused by ferromagnetic objects, such as surgical tools, that may cause limitation in its accuracy.
TUNNEL PLACEMENT USING CAS
One of the most critical factors for successful clinical outcome of ACL reconstruction is proper intra-articular positioning of the graft. There is general agreement that long-term results are significantly influenced by correct tunnel placement (5,14,20,31).
Clinical validation of the navigation was focused on the evaluation of tunnel placement. CAS systems for ACL reconstruction have focused on isometry and graft elongation (4,13,25,37,49, 50, 51,53) or on impingementfree placement (16,21,23,40,49,53,54). Most of the papers highlighted the versatility of the systems for different surgical techniques, indicating the CAS as useful tool in reducing surgical errors (15,51,53).
The evaluation was made analyzing the repeatability of tunnel placement with respect to femoral and tibial anatomical references and comparing it with patients operated with conventional technique (1,22,28,29,40,41,44,48,54,60). Some surgeons (8,40,54) found no significant differences between CAS surgery and manual placement by an experienced surgeon. While in contrast, others (15,28,61) found improved accuracy with a computer-assisted system based on radiographs and computer animation.
In tibial placement, the mean position of tunnels is not altered by the use of navigated systems, but the deviation is significantly decreased (8,28,53,54,61). Nevertheless studies from several centers have shown to improve most significantly femoral placement, most studies (28,48,53) showed improved positioning in navigated ACL reconstruction using radiographic data. Because many studies are still defining the position of ACL at the femoral site (17), there is no clear optimal aiming point. The position in the femur is also related to kinematic outcome found during in vitro laboratory experiments (33,42,45,64). The navigation system makes it possible to obtain time zero data on the table even if these data are still influenced by other factors such as meniscal damage or removal and collateral damage on extra-articular structures (3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree