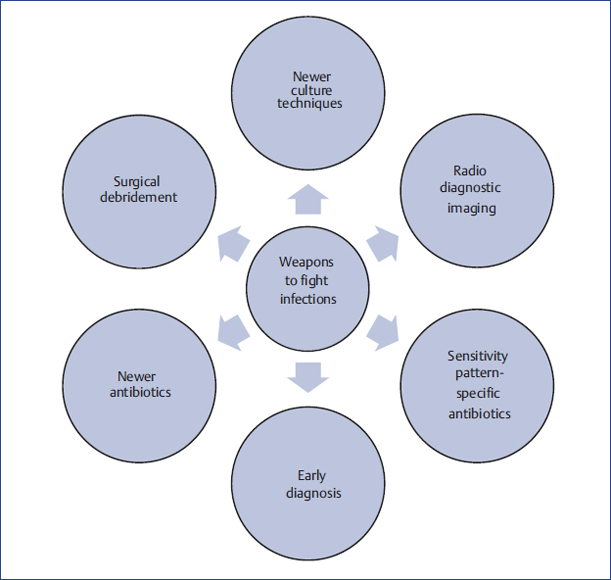
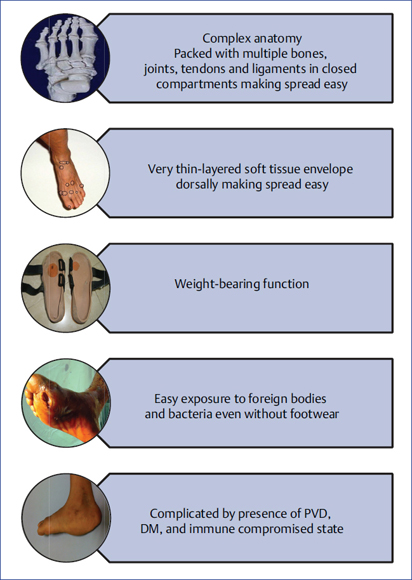
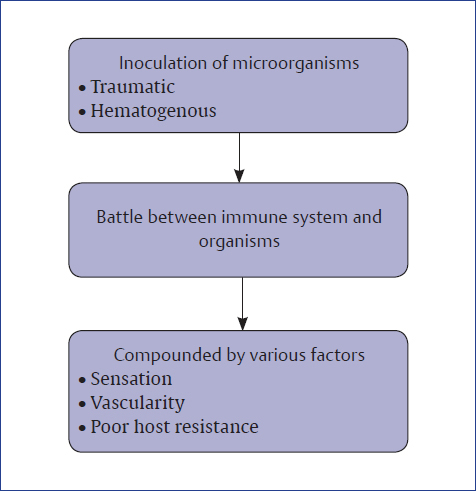
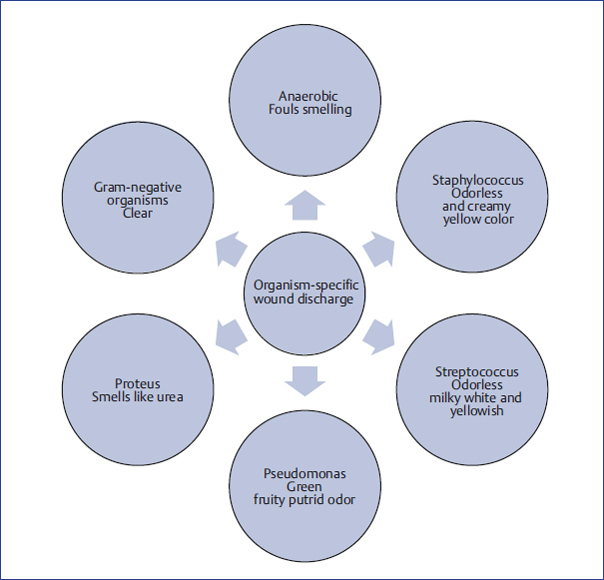
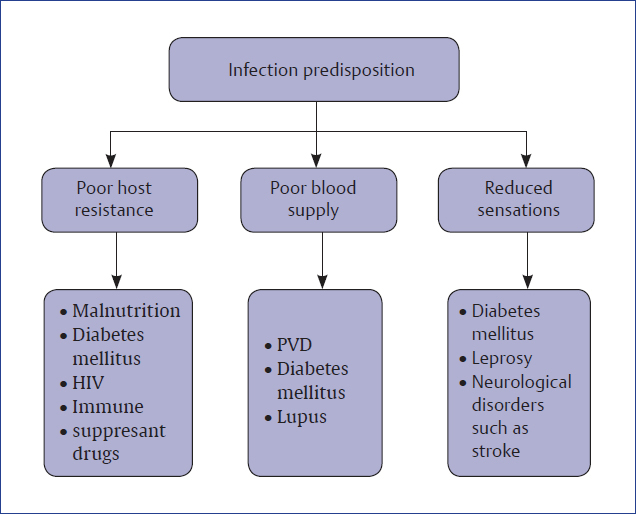
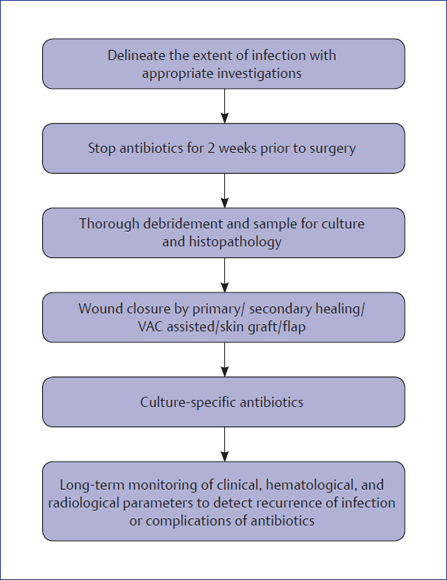
Chapter Modern-day infections are different with respect to type of organisms, resistance pattern, pattern of presentations, and unique state of immune compromised cases! Fig. 13.1 shows armamentarium of clinicians to battle with modern-day infections. Foot infections are different from infections elsewhere in the body owing to the specific anatomic and physiologic features of the foot. These features cause easy spread of infection which is explained in Fig. 13.2. Pathogenesis of infections of foot and ankle is illustrated in Flowchart 13.1. Flowchart 13.2 displays causes and conditions that predisposes host to infection. Flowchart 13.2 Reasons for predisposition to infections. ♦ The foot can be affected by a wide range of conditions ranging from a relatively mild foreign body granuloma to a limb- or life-threatening gangrene. ♦ Etiologies: Traumatic or nontraumatic. ♦ Either of the etiologies can result in the following: • Cellulitis • Fasciitis • Osteomyelitis • Infective arthritis ♦ Soft-tissue infections can be following: • Ingrowing toe nail • Paronychia • Erythrasma • Foreign body impaction • Puncture wounds • Cellulitis • Peripheral vascular disease (PVD) ♦ Bone infection (osteomyelitis): Acute, chronic, or posttraumatic. Osteomyelitis may be pyogenic or tubercular in nature. ♦ Diabetic foot: A variety in itself. ♦ Usual bacteria that cause infection in the foot include: •Staphylococcus aureus • Group A Streptococci •Pseudomonas aeruginosa To reach at correct diagnosis, proper history of the patient along with evaluation of the signs and symptoms should be carried out. ♦ A detailed history is essential, more so in foot infections. A trivial trauma thought to be insignificant by the patient could be significant in the context of the clinical scenario. ♦ Details of the type of trauma (low or high energy) and the environment in which it occurred (e.g., farm yard) could give a clue regarding the organism that one is dealing with. ♦ Medical history to rule out compounding factors such as diabetes, peripheral vascular disease, and smoking. ♦ Pain: For example, throbbing pain suggests case of pyogenic infection or inflammation ♦ Swelling ♦ Constitutional symptoms such as fever, nausea, or vomiting are indicative of septicemia or bacteremia ♦ Discharge: Look for color and presence of bone pieces ♦ Redness ♦ Edema: Leads to loss of skin wrinkles ♦ Sinus: Probe the sinus to feel the base and confirm whether it is bony or soft tissue. Palpating bone when probing the lesion is highly specific and has a high positive predictive value for diagnosis of osteomyelitis. ♦ Discharge: Smell and color of discharge can give an indication of the organisms involved (Fig. 13.3). ♦ Neurovascular examination is necessary to diagnose associated neuropathy and vascular disease. Pain in the presence of neuropathy is indicative of underlying infection. The following investigations are to be carried out prior to starting the treatment. ♦ CBC may not be raised in severe infection or diabetes ♦ ESR and CRP are indicators of infection and are also used to assess improvement after antibiotics and/or debridement ♦ Liver and renal functions must be assessed prior to starting antibiotics. ♦ Serum albumin levels are necessary to correct malnutrition. ♦ Might show increased soft tissue shadow ♦ Gas could be due to gas gangrene ♦ Foreign body could be seen. For example, radiopaque objects such as metal, gravel, and glass can be identified easily with plain films ♦ Osteolytic lesions in bone, periosteal reaction, sequestrum, involucrum, etc., indicate osteomyelitis. Changes are seen after 2 weeks of infection ♦ Radiolucent objects such as glass, rubber, and wood could be seen easily ♦ It helps to define the extent of abscess ♦ It is the most sensitive investigation. One study demonstrated MRI to be significantly more sensitive and accurate, with equal specificity in comparison to plain radiographs, technetium-99m MDP, and gallium-67 scans in osteomyelitis. With bone infection, marrow is replaced by fluid and inflammatory cells, which are displayed as regions of reduced signal intensity on T1-weighted images and as increased signal intensity on T2-weighted images and short tau inversion recovery (STIR) sequences ♦ It best detects changes in soft tissues ♦ Extent of involvement of muscles, ligaments, joints, and fascial planes could also be assessed ♦ It differentiates viable tissue from necrotic tissue ♦ General consensus exists that MRI is a superior study to CT scan when assessing for nonviable tissue or drainable fluid collections ♦ It is ideal for detecting bony changes ♦ It also detects cortical breaks and osteolytic lesions ♦ It is useful in involucrum and sequestrum ♦ It can detect pus pocket within the medullary canal ♦ It delineates abscess cavity ♦ It detects gas in deep tissues in cases of gas gangrene or necrotizing fasciitis ♦ Scintigraphic studies can be useful in the diagnosis of bone infections in the foot, bone infection versus soft tissue infection, and bone infection versus Charcot osteoarthropathy ♦ The three common nuclear medicine studies in this group include the radioactive forms of technetium, gallium, and indium ♦ Technetium-99m methylene diphosphonate (MDP) • MDP detects infection 24 to 48 hours after its onset • It is a three-phase test • Uptake in all three phases indicates osteomyelitis • No or minimum uptake in last phase suggests soft tissue infection • This is not very specific as high uptake is seen following surgery, following trauma, bone tumors, and Charcot’s osteoarthropathy ♦ Gallium-67 • Gallium accumulates in bone • It is false negative in case of antibiotics administration • It is false positive in case of soft tissue infection, hematoma, fracture, surgery, and tumor ♦ Leukocyte-labeled indium-111 • This is more sensitive and specific • It cannot detect chronic osteomyelitis • It is time consuming (3 days) ♦ Leukocyte-labeled technetium-99m hexamethyl propylamine oxime (HMPAO) • HMPAO is completed in 3 to 4 hours • It is useful in differentiating osteomyelitis from postfracture or postsurgical state • It is useful in differentiating osteomyelitis from Charcot’s osteoarthropathy ♦ Deep tissue sample is ideal for culture ♦ Superficial swab is contaminated with normal flora and hence should be avoided. ♦ Biopsy is also very useful for diagnosing bone infections. Bone biopsy remains the standard criterion in the diagnosis of osteomyelitis ♦ Gram and Zeil–Neihlson staining can help in starting empirical antibiotics ♦ Various culture media are used to identify the organism Flowchart 13.3 gives a brief overview of the surgical management of infections of foot and ankle. Flowchart 13.3 Overview of the surgical management of infections.
13
Common Foot and Ankle Infections: Diagnosis and Management
Introduction
How Foot and Ankle Infections Are Different?
Pathogenesis of Foot and Ankle Infections
Spectrum of Infections
Diagnosis
History
Symptoms
Signs
Investigations
Hematology
Plain Radiograph
Ultrasonography
MRI
CT scan
Scintigraphy
Wound Culture
Management of Infections
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree