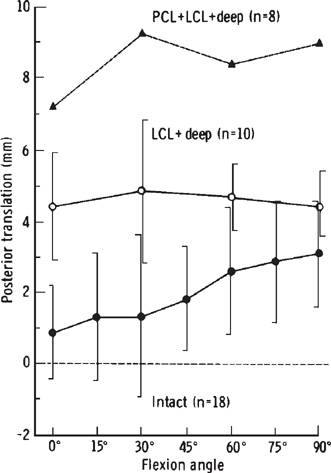
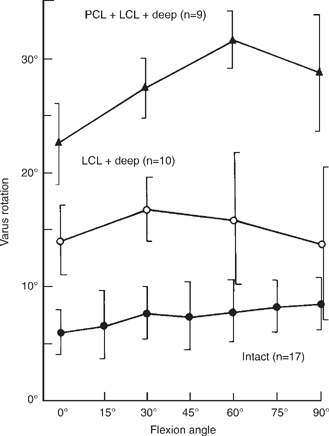
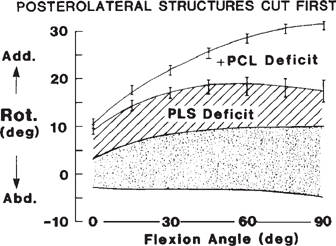
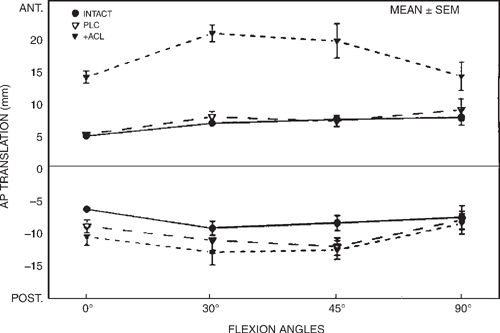
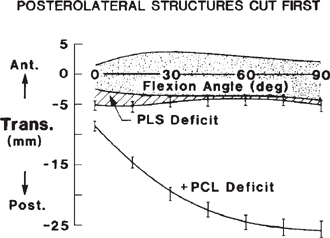
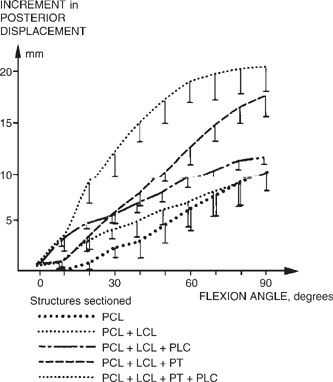
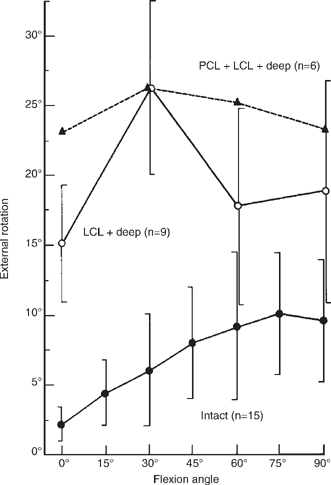
6 Modern biomechanical testing of knee motion limits to determine the contribution of individual structures or groups of structures to knee stability has been performed since the mid-1970s,1 when techniques were developed for continuous recordings of force and applied moments, displacement, and rotational relationships. Earlier biomechanical testing techniques had significant sources of potential error due to an inability to obtain precise measurements of the applied loads or motion achieved with an applied load. Those previous techniques included manual manipulation of the knees to apply loads, slings and weight-pulley systems to apply loads, and stress radiographs to measure motion.2,3 Although these previous studies helped to improve the understanding of how structures contributed to knee instability, they lacked accuracy because many of the forces or applied moments to the knees were not known or controlled and the amount of displacement or rotation were either estimated or imprecisely measured as simultaneous displacement could not be recorded. For this reason, this chapter discusses only those biomechanical studies on the posterolateral knee that provide a quantitative measurement of the forces, moment displacements, or rotations tested. Most biomechanical studies of the posterolateral knee have been studied largely through cadaveric sequential sectioning studies, in which the knee was subjected to joint loading before and after sectioning of a specific structure or group of structures. The resulting changes in joint motion were assessed and utilized to quantitate the contribution of the cut structure to overall knee stability for particularly applied loads. More recent studies have applied a given displacement to the joint, and measure the change in force present to create this displacement both before and after cutting individual specific posterolateral structures. Many of the biomechanical studies about the posterolateral knee are difficult to compare with each other due to differences in nomenclature and the fact that many sequential cutting studies have grouped and sectioned these posterolateral structures together rather than studying them as individual structures. A review of the pertinent modern biomechanical studies of the posterolateral knee with an attempt to summarize which structures are important to primary and secondary knee stability follows. I have grouped the clinically relevant biomechanics into specific areas of motion testing to aid in the understanding of which structures may be injured for specific regions of instability abnormalities in patients with posterolateral knee injuries. The studies are summarized according to primary and secondary restraints. For those structures that are primary restraints, the instability being tested has found that structure which was cut or injured is the main restraint to that particular motion. Some structures provide secondary restraints to a particular motion when the primary restraint is absent. Also, it is important to recognize that injuries to the posterolateral corner of the knee are more complex than the lesions created in restraint and selective sectioning studies under static conditions in biomechanical testing laboratories. If one constant exists with respect to the stability provided to the posterolateral knee from a static biomechanical standpoint, it is that all studies have shown that the fibular collateral ligament is the primary restraint to varus motion in all positions of knee flexion.1,4–9 Isolated sectioning of the fibular collateral ligament results in a significant increase in varus rotation at any knee flexion angle,6–10 and varus rotation has not been demonstrated to be increased with posterolateral structure sectioning as long as the fibular collateral ligament is still intact.6,9 Grood et al5 examined the restraints to varus opening of the knee at 5 and 25 degrees of knee flexion by measuring the forces necessary to create 5 mm of lateral joint line opening. They reported that at 5 degrees of knee flexion, the fibular collateral ligament was calculated to provide about 55% of the restraining moment to 5 mm of lateral joint line opening. The cruciate ligaments were calculated to contribute 22% to lateral restraint, the posterior capsule 13%, the iliotibial band and popliteus tendon 5%, and the anterior and midlateral capsule 4%. In comparison, at 25 degrees of knee flexion, the role of the fibular collateral ligament to restraining varus moment increased to 69%, whereas the role of the cruciates and combined capsule decreased to 12% and 9%, respectively. The role of the iliotibial band and popliteus tendon in providing lateral restraint was also slightly increased to 10%. Many other structures have been found to be important in providing secondary varus stability to the knee when the fibular collateral ligament was sectioned. Nielsen et al6 found a marked increase in varus opening of the knee with combined sectioning of the fibular collateral ligament and the posterolateral capsule of the knee, which was found to be maximal at 40 degrees of knee flexion. In another study, Nielsen et al1 reported that combined posterior cruciate ligament (PCL), fibular collateral ligament, and posterolateral structure sectioning resulted in a marked increase in varus instability of the knee. Nielsen and Helmig12 also found that the popliteus tendon had an important secondary role in preventing abnormal varus opening after the fibular collateral ligament was sectioned. They found that the maximal increase in varus opening again was at 40 degrees of knee flexion. Gollehon et al8 sectioned the popliteus tendon and the posterolateral capsular structures, whereas Grood et al9 cut the popliteus tendon attachment on the femur and the posterolateral part of the capsule, including the arcuate complex (which appears to be the popliteofibular ligament and capsular arm of the short head of the biceps femoris), along with the capsular attachment of the popliteus muscle (which appears to be the popliteal aponeurosis to the lateral meniscus) and any fabellofibular ligament or short lateral ligament that the authors found to be present after cutting the fibular collateral ligament. In both of these studies,8,9 varus rotation was significantly increased with sectioning of these posterolateral knee structures compared with isolated fibular collateral ligament sectioning alone (Figs. 6-1 and 6-2).Veltri et al10 found that additional sectioning of the popliteus tendon or popliteofibular ligament after the fibular collateral ligament was cut resulted in a significant further increase in varus rotation, which was found to be maximal at 30 degrees of knee flexion. Figure 6-1 Varus opening with cutting posterolateral structures with 10 Newton- meters of varus torque applied. LCL, lateral collateral ligament; PCL, posterior cruciate ligament. (From Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg 1987;69A:233–242, with permission.) Figure 6-2 Varus opening with cutting posterolateral corner structures with application of a 20-newton meter torque. Shaded area, intact knees. Add., adduction (varus); abd., abduction (valgus); PLS, posterolateral structure. (From Grood ES, Stowers SF, Noyes FR. Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg 1988;70A:88–97, with permission.) Studies have also shown that both cruciate ligaments are recruited to help resist an applied varus moment when the fibular collateral ligament and other posterolateral structures are absent. Gollehon et al8 demonstrated that if the PCL was sectioned after the fibular collateral ligament and the deep posterolateral ligament complex were sectioned, a large increase in varus rotation occurred compared with isolated sectioning of the fibular collateral ligament at all knee flexion angles. Grood et al9 also reported that cutting the PCL, after the fibular collateral ligament, popliteus tendon, and posterolateral structures were cut, resulted in increased varus rotation, which was maximally increased at 90 degrees. However, it has also been found that isolated PCL sectioning alone (with intact posterolateral knee structures) did not increase varus rotation of the knee.8,9,11 Nielsen and Helmig12 noted that the varus instability caused by anterior cruciate ligament (ACL) and fibular collateral ligament cutting could not be distinguished from isolated fibular collateral ligament cutting, and they postulated that the ACL could not be regarded as the primary varus stabilizer of the knee. Wroble et al13 reported that isolated ACL sectioning resulted in no significant increase in varus opening at any knee flexion angle. They also demonstrated that in the ACL-deficient knee, cutting the fibular collateral ligament increased varus instability by only small amounts (at an average of 3 degrees), whereas additional sectioning of the posterolateral structures (which appear to be the popliteus and the associated posterolateral complex) produced larger secondary increases in varus opening at all knee flexion angles. Markolf et al14,15 reported that the resultant forces on the cruciate ligaments of cadaveric knees subjected to varus moments were significantly increased when the fibular collateral ligament and posterolateral structures were cut. They noted that when a varus moment was applied, the mean force on the native ACL was significantly increased when the posterolateral structures were cut compared with the intact state at all knee flexion angles. In addition, they reported that the native PCL, in a knee with intact posterolateral structures, was not loaded by varus moments applied to the knee. However, after the posterolateral structures were cut, the PCL became a main secondary restraint to an applied varus moment. When the posterolateral structures were cut, the PCL was found to have a significant increase in the mean force found on it at flexion angles greater than 45 degrees for an applied varus moment.14 Maynard et al16 performed mechanical strength testing of the fibular collateral ligament, popliteofibular ligament, and popliteus tendon (all three were pulled together) along the long axis of the fibular collateral ligament to simulate a pure varus injury to the knee. They found that tensile testing, at a rate of 100% per second, first resulted in failure of the fibular collateral ligament, at an average force to failure of 747 N, followed by failure of the popliteofibular ligament (with primarily intrasubstance tearing) at an average force to failure of 425 N, and failure of the popliteus tendon at its musculotendinous junction. Therefore, in spite of many varying experimental models, the main structure that has been demonstrated to provide knee stability with application of a varus force is the fibular collateral ligament. In addition, the popliteus complex, posterolateral capsule, and cruciate ligaments have also been demonstrated to have an important secondary role in preventing varus instability when the fibular collateral ligament was cut. This means that if a knee does have an increase in varus opening on clinical examination, one must first suspect an injury to the fibular collateral ligament. Significant increases in a varus opening clinically would mean either a combined posterolateral structure injury or possibly a combined cruciate ligament tear is present. Studies have not demonstrated any role of the posterolateral structures in preventing increased valgus motion.6,8,13 Markolf et al14 found that valgus angulation of the tibia was unaffected by sectioning of the fibular collateral ligament and posterolateral structures. In addition, they found no increase on force on either the anterior cruciate or PCL for an applied valgus moment with the posterolateral structures sectioned. Veltri et al10 also found no greater than a 1-degree increase in primary valgus rotation of the knee for any isolated or combined posterolateral structure sectioning. Selective sectioning studies have reported that cutting the posterolateral structures results in no significant increase in primary anterior tibial translation.8,9,12 Veltri et al10 found that for isolated posterolateral corner sectioning (which appears to include the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and the capsular arm of the short head of the biceps femoris), there was no change in anterior translation of the knee with an anterior applied force at any knee flexion angle. Veltri et al17 also found no significant change in anterior translation of the knee for posterolateral structure sectioning in a similar study. This would indicate that the posterolateral structures do not have a primary role in preventing anterior tibial translation of the knee. If one suspects an isolated posterolateral corner injury, there should not be any increase in anterior translation for the true Lachman test. However, there may be some increase in posterolateral motion, which may make it seem like there is an increased amount of relative anterior translation. In this instance, there should be a solid end point to the anterior Lachman test on clinical examination. Nielsen and Helmig12 found that anterior tibial displacement with the posterolateral capsule, popliteus tendon, and fibular collateral ligament sectioned was not increased until the ACL was also cut. They felt that this indicated that the posterolateral structures were an important secondary restraint to anterior tibial translation in the ACL-deficient knee. They also found that cutting the popliteus tendon or posterolateral structures in the ACL-deficient knee increased anterior tibial translation, most notably in the initial 40 degrees of knee flexion. They also noted that combined cutting of the ACL, popliteus tendon, and all posterolateral structures resulted in further increases in anterior translation instability up to 90 degrees of knee flexion. Wroble13 also found that in the ACL-deficient knee, cutting the fibular collateral ligament or posterolateral structures (the popliteus tendon and posterolateral capsule) produced small, but significant, increases in anterior tibial translation. They also reported that for combined sectioning of both the ACL and posterolateral structures, anterior tibial translation increased primarily near extension (in the initial 15 to 30 degrees of knee flexion), which they noted caused increased anterior translation that should be measurable clinically on the Lachman test. In the ACL-deficient knee, the posterolateral structures that act as secondary restraints to anterior translation at 90 degrees of knee flexion have been found to include the iliotibial band, mid-third lateral capsular ligament, and the fibular collateral ligament.18 In these ACL-deficient knees, the mean force contribution to anterior drawer at 90 degrees was calculated to be 25% for the iliotibial band, 21% for the mid-third lateral capsular ligament, and 12% for the fibular collateral ligament. The remaining forces were taken up by medial-sided structures. Veltri et al10 found results similar to those of other studies in knees in which the posterolateral structures were sectioned along with the ACL. In these knees, the authors found that significant increases in anterior translation occurred at all knee flexion angles for combined ACL and posterolateral structure sectioning compared with isolating sectioning of the posterolateral structures or for intact knees (Fig. 6-3). The maximal increase in anterior translation was found at 30 degrees of knee flexion for combined ACL and posterolateral structure sectioning. The authors stated that this indicated that the posterolateral structures were an important secondary stabilizer to anterior tibial translation. A study that measured the force in the posterolateral knee structures, using a robotic/universal force-moment sensor testing system, revealed that the forces in the posterolateral structures were minimal with an intact ACL (<20 N), but that the forces present on the posterolateral structures when the ACL was sectioned increased by 123% at full knee extension and 413% at 15 degrees of knee flexion for an 134 N·m anteriorly applied force.19 This would confirm the results of other authors, who found that although the posterolateral knee structures play a minor role in resisting anterior tibial translation in an intact ACL knee,8–10,12,17 they have a significant role in resisting anterior tibial translation in the ACL-deficient knee.10,12,13 In analyzing Kanamori et al’s19 study, one could postulate that this information has very important implications for isolated repairs or reconstructions of torn posterolateral knee structures that occur in combination with an ACL tear. This study indicates that an isolated repair or reconstruction of torn posterolateral knee structures would be at risk for stretching out, if the ACL was not simultaneously reconstructed, because of the extra forces seen in the posterolateral structures with an ACL-deficient knee. Figure 6-3 Secondary role of the posterolateral structures to preventing anterior tibial translation in the anterior cruciate ligament (ACL)-deficient knee resulting from a 100-newton meter anterior force, isolating sectioning if the posterolateral structures did not increase anterior translation at any flexion angle. PLC, posterolateral corner; ACL, anterior cruciate ligament. (From Veltri DM, Deng X-H, Torzilli PA, Warren RF, Maynard MJ. The role of the cruciate and posterolateral ligaments in stability of the knee. Am J Sports Med 1995;23: 436–443, with permission.) In summary, although the posterolateral structures do not have a primary role in preventing anterior tibial translation of the knee, they do play a very important role as a secondary restraint to anterior tibial translation in the ACL- deficient knee. In addition, the increase in anterior tibial translation seen with posterolateral corner injuries in a combined ACL tear should result in a significant increase in anterior tibial translation on the Lachman test that should be detectable clinically.10,12,13 Therefore, in a knee with a 3+ or 4+ Lachman test and no other obvious ligament instability, including an intact posterior horn of the medial meniscus, the examiner must rule out a potential concurrent posterolateral knee injury. It has also been demonstrated that there is a significant increase in force on the posterolateral knee structures in an ACL-deficient knee. This important biomechanical finding supplements the clinical observation that, in combined posterolateral and cruciate ligament injuries, both the posterolateral structures and the cruciate ligament should be repaired or reconstructed concurrently at the original surgery, rather than during a staged surgery, to prevent the posterolateral structures from being stretched out. It is very important to recognize that the main stabilizer of the knee with respect to primary posterior tibial translation is an intact PCL.2,7,8,10,18,20 It is also important to recognize that the amount of posterior tibial translation that occurs with isolated sectioning of the PCL increases with increasing knee flexion angles. The greatest amount of measured posterior translation in the PCL-deficient knee was found to be at 90 degrees of knee flexion with values ranging from 1 to 5 mm at 0 degrees of knee flexion to 11 to 20 mm at 90 degrees of knee flexion.8,9 The posterolateral structures of the knee have been noted to play a significant primary, but minor, role in restricting posterior tibial translation. Gollehon et al8 reported that isolated sectioning of the posterolateral structures resulted in at least a slight increase in posterior tibial translation at all angles of knee flexion. They also found that at 0 and 30 degrees of knee flexion there was no significant difference in posterior translation between specimens in which sectioning of the posterolateral structures was performed alone and those that have undergone isolated PCL sectioning (Fig. 6-4). Grood et al9 found that cutting all of the posterolateral structures resulted in a small, but significant, increase in posterior tibial translation from 0 to 45 degrees of knee flexion (Fig. 6-5). In addition, Veltri et al10 found that isolated sectioning of the posterolateral corner (which appears to have included the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and the capsular arm of the short head of the biceps femoris) resulted in increases in posterior tibial translation with application of a posterior force at all angles of knee flexion with maximal increases occurring between 30 and 45 degrees of knee flexion. In a separate study, Veltri et al17 also reported that isolated sectioning of the posterolateral structures affected primary posterior translation of the knee. Sectioning of the posterolateral structures increased posterior tibial translation at all degreesof knee flexion. Maximum primary posterior tibial translation was between 3.4 and 3.9 mm at between 30 and 45 degrees of knee flexion for isolated posterolateral structures sectioning. These studies8–10,17 indicate that the posterolateral structures have a small but important primary role in preventing increased posterior tibial translation of the knee, especially near extension. This finding has important clinical significance in that the starting point of the tibia would be more posterior on the initial assessment of a Lachman’s test with a posterolateral knee injury, which would be especially important with an intact ACL. The increase in anterior tibial translation from this “pseudo-Lachman” test may give the false impression of increased anterior tibial translation with an intact ACL. It is important to recognize that in these cases, the pseudo-Lachman test would have a solid end point, and the examiner in this case must carefully assess the integrity of the ACL. Figure 6-4 Increases in primary posterior translation with posterolateral knee structure cutting, compared with intact knees. Primary posterior translation increased more near the extension for lateral (fibular) collateral ligament (LCL) and deep structure sectioning, and posterior translation increased at 60° and 90° when the posterior collateral ligament (PCL) was also cut. (From Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg 1987;69A:233–242, with permission.) In addition to the minor primary role of the posterolateral knee structures in restricting posterior tibial translation, they have also been found to have an important secondary role in providing posterior stability in a PCL-deficient knee. Nielsen and Helmig7 reported that combined cutting of the PCL, fibular collateral ligament, and posterolateral structures resulted in marked increases in posterior tibial translation, which became more important with increasing knee flexion. Gollehon et al8 noted that combined PCL and posterolateral structures cutting resulted in a large increase in posterior tibial translation at all knee flexion angles. Grood et al9 also reported that there was a significant further increase in posterior tibial translation after both the PCL and posterolateral structures were cut. Butler et al18 found that the posterolateral capsule and popliteus tendon had a significant role in acting as a secondary restraint to posterior tibial translation when the PCL was cut at 90 degrees of knee flexion, whereas the iliotibial band and mid-third lateral capsular ligament had no primary or secondary role in resisting posterior tibial translation at 90 degrees. Although the medial collateral ligament complex, posteromedial capsule, mid-third medial capsular ligament, and fibular collateral ligament had some secondary role in preventing posterior tibial translation in a PCL-deficient knee, only the loss of the combined restraint of the posterolateral capsule and popliteus tendon was found to cause a significant increase in posterior tibial translation in a PCL-deficient knee.18 Figure 6-5 Increases in primary posterior tibial translation with posterolateral knee structure cutting. (From Grood ES, Stowers SF, Noyes FR. Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg 1988;70A:88–97, with permission.) Nielsen and Helmig7 found that in the PCL-deficient knee, the popliteus tendon was the structure that had the largest effect on resisting posterior tibial translation from 10 to 90 degrees of knee flexion when it was cut (Fig. 6-6).Others have also demonstrated that combined sectioning of the PCL and posterolateral structures of the knee significantly increased posterior tibial translation compared with isolating sectioning of either the PCL or the posterolateral structures individually.8,9 Markolf et al14 measured the force in the PCL with a posteriorly applied 50-N force with concurrent fibular collateral ligament and posterolateral corner structure sectioning. They found that the mean force on the PCL was unaffected by sectioning of these posterolateral structures for a straight posteriorly applied force. Harner et al21 evaluated the effect of a simulated contraction of the popliteus muscle on both the forces seen on the native PCL and in knee kinematic changes for a 110-N posteriorly applied load (which simulated a posterior drawer test) using a cadaveric robotic model. They found that a simulated 44-N contraction of the popliteus muscle resulted in significantly decreased in situ forces seen on the native PCL at both 30 and 90 degrees of knee flexion. In addition, they found that after cutting the PCL, the amount of posterior translation of the tibia was reduced by up to 36% with a simulated popliteus muscle contraction. They concluded that this demonstrated the popliteus muscle dynamically resists posterior tibial translation with the PCL, and an intact and functional popliteus complex can help with improved knee stability in the PCL-deficient knee. They confirmed the clinical observation by Barnett and Richardson22 that the popliteus complex provides active support to the PCL in resisting posterior subluxation of the tibia on the femur in the flexed knee. Figure 6-6 The role of the popliteus tendon on increases in posterior knee translation during sequential structure sectioning and a 25-newton meter positively directed force. PCL, posterior increase ligament; LCL, lateral (fibular) collateral ligament; PLC, posterolateral corner; PT, popliters tendon. (From Nielsen S, Helmig P. The static stabilizing function of the popliteal tendon in the knee: an experimental study. Arch Orthop Trauma Surg 1986;104:357–362, with permission.) In summary, the posterolateral structures of the knee act as a minor, but significant, primary restraint to posterior tibial translation across all angles of knee flexion,8–10,17 but the PCL is the main primary stabilizer for these posterior translation movements.2,7,8,10,18,20 The role of primary restraint of the posterolateral structures of the knee to posterior tibial translation is most important between 0 and 30 degrees of knee flexion, where the amount of posterior tibial translation may be as much as for a knee with an isolated posterolateral corner injury as for an isolated PCL tear.8,9 This has clinical importance in a knee with a posterolateral corner injury in that these may be a false impression of anterior translation on the Lachman test or pseudo-Lachman test in a knee with an intact ACL. In a PCL-deficient knee, the posterolateral structures also act as an important secondary stabilizer to posterior translation of the knee. When the posterolateral structures and the PCL were both cut, a significant further increase in posterior translation was seen compared with isolated cutting of either structure.7–9,18 This has important clinical significance because most 2+ posterior drawer tears have an isolated PCL tear, whereas most 3+ posterior drawer tests knee combined PCL and posterolateral structure injuries. This information has been found to be important in the assessment of increased posterior translation on PCL stress radiographs. As mentioned previously, most isolated PCL tears have less than 1 cm of increased posterior translation on PCL stress x-rays. However, increases on posterior translation equal to or greater than 12 mm are almost always an indication of a combined PCL and posterolateral corner injury (or a possible combined posteromedial knee injury). Lipke et al23 measured motion changes with ACL and anterolateral/posterolateral structure cutting between 0 and 40 degrees of knee flexion. They reported that isolated fibular collateral ligament and posterolateral complex (described as the lateral capsule and ligament structures) sectioning resulted in no significant increase in internal rotation until the ACL was also cut. They also found a significant increase in internal rotation when the ACL was cut, and further additional internal rotation occurred with cutting the fibular collateral ligament or posterolateral structures. They did not assess higher knee flexion angles in their biomechanical testing studies. However, other studies performed at varying knee flexion angles have shown that when an internal rotation torque was placed on the knee, an isolated or combined loss of the fibular collateral ligament, deep or posterolateral structures (the popliteus complex and posterior joint capsule), or PCL caused a significant increase in primary internal rotation of the tibia.6,9,24 In addition, Veltri et al10 found a small, but significant, increase in internal tibial rotation with the posterolateral structures cut compared with intact knees. However, the maximal increase was only 2.9 degrees at 90 degrees of knee flexion. The small increase in primary internal rotation seen in other studies may explain why it was not found in Lipke et al’s23 study. Nielsen et al6 reported that cutting the fibular collateral ligament and the posterolateral knee structures resulted in increased internal rotation at flexion angles greater than 50 degrees. Nielsen et al11 also noted no increase in primary internal tibial rotation with isolated PCL sectioning. In addition, Wroble et al13 demonstrated that in the ACL-deficient knee, the posterolateral structures (which appear to be the popliteus complex and posterolateral capsule in their study) had an important role as a secondary stabilizer in preventing internal tibial rotation, which was most important close to knee extension. Markolf et al14 measured the forces generated in the cruciate ligaments when the posterolateral structures were cut and found the mean force on the ACL increased at 0, 10, and 20 degrees of knee flexion, but not at higher knee flexion angles, for an applied internal rotation torque. They found no change in PCL force at any knee flexion angle with the posterolateral structures sectioned for any applied internal rotation torque.14 In summary, it appears that the posterolateral structures play a small role in preventing primary internal rotation of the knee. In addition, they play an important role as a secondary restraint to internal rotation in the ACL-deficient knee, especially when the knee is close to extension. However, due to the varied amount of internal rotation changes and the large standard deviations seen for this test, this particular knee instability has not been shown to have much clinical significance to date in motion testing. Perhaps further study into its clinical significance and the development of a clinical test to measure this motion abnormality may be indicated. The integrity of the posterolateral structures has been demonstrated to be very important in preventing increased primary external rotation of the knee. Lipke et al23 found that with cutting all the structures of the posterolateral complex, a significant increase in external rotation was found between 0 and 40 degrees of knee flexion. However, they did not assess this affect at higher knee flexion angles. Nielsen et al6 found no change in external rotation of the knee with isolated fibular collateral ligament cutting and minimal changes with isolated posterolateral structures (everything except the fibular collateral ligament) sectioning. They found a large increase in external rotation, however, with an average of 15.6 degrees, at 30 degrees of knee flexion and a 10.2-degree increase in external rotation at 70 degrees of knee flexion, with combined fibular collateral ligament and posterolateral capsule sectioning. They found the maximal increase in external rotation was at 35 degrees of knee flexion. Nielsen et al11 noted a significant increase in external rotation occurred with combined PCL, fibular collateral ligament, and posterolateral structure sectioning, which increased with increasing knee flexion. They postulated that this would indicate that the PCL is an important secondary stabilizer to external rotation at knee flexion angles greater than 35 degrees. Nielsen and Helmig12 found a significant increase in external rotation for isolated popliteus tendon sectioning between 20 and 130 degrees of knee flexion. They found the largest increased amount of external rotation (16 degrees) occurred at 30 degrees of knee flexion with the fibular collateral ligament, popliteus tendon, and posterolateral corner structures cut. Further flexion of the knee under these same cutting conditions resulted in a decrease in the amount of external rotation with ~7 degrees of increased external rotation compared with an intact knee occurring at 90 degrees of knee flexion. Gollehon et al8 also demonstrated the importance of intact posterolateral structures with respect to external tibial rotation. They noted that isolated sectioning of the fibular collateral ligament, as well as the popliteus complex, resulted in a significant increase in external tibial rotation at all knee flexion angles compared with intact knees (Fig. 6-7). Grood et al9 found that after sectioning of the posterolateral structures (which appear to have been the fibular collateral ligament, popliteofibular ligament, fabellofibular ligament, capsular arm of the short head of the biceps femoris, and the popliteus tendon femoral attachment), a significant increase in external tibial rotation occurred at both 30 and 90 degrees of knee flexion (13 and 5.3 degrees of increase, respectively) (Fig. 6-8). Veltri et al10 also found that cutting the fibular collateral ligament, popliteus tendon, and popliteofibular ligament resulted in an increase in external rotation at all angles of knee flexion, which was maximum at 45 degrees. In addition, Kaneda et al25 verified some of these previous studies,8,9 using biplanar roentgenographic photogrammetry and assessed the effect of cutting the posterolateral structures on external tibial rotation of the knee. They found that sectioning the fibular collateral ligament and the posterolateral structures (which appear to have been the popliteofibular ligament, fabellofibular ligament, popliteus tendon, and the capsular arm of the short head of the biceps femoris) resulted in significant increases in external tibial rotation at 30, 60, and 90 degrees of knee flexion compared with the intact knee state. The clinical significance of these biomechanical studies is that the dial test at 30 and 90 degrees for examination of the knee is based on the results found in these biomechanical studies.7–10,25
Clinically Relevant Biomechanics of Posterolateral Knee Injuries
♦ Role of the Posterolateral Structures in Preventing Varus/Valgus Motion
♦ Role of Posterolateral Structures in Preventing Anterior Translation
♦ The Role of the Posterolateral Structures in Preventing Posterior Translation of the Tibia
♦ Role of the Posterolateral Structures in Preventing Internal Rotation at the Knee
♦ Role of the Posterolateral Structures in Preventing External Rotation at the Knee
Clinically Relevant Biomechanics of Posterolateral Knee Injuries
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree