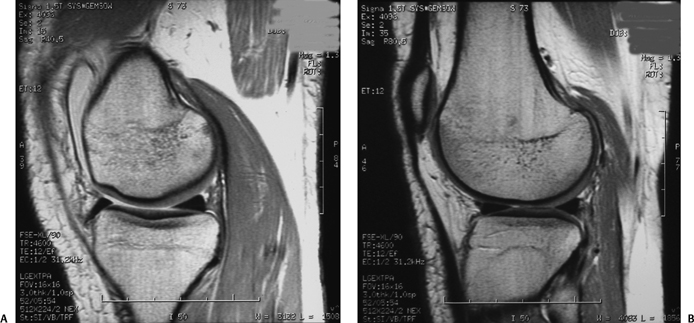
1 Posterolateral corner knee injuries can be very problematic injuries when they are not recognized by the treating health care professional. This is especially true as the operative results of significant injuries for acute repairs are much better than chronic reconstructions. This can be compounded by the fact that we haven’t as a profession developed specific diagnostic tools to help identify these injuries, and many physicians do not include the multiple varied means to clinically diagnose posterolateral corner knee injuries in their repertoire for the clinical examination of an acute or chronic ligament-injured knee. Physicians who treat acute knee injuries should heed the advice of the late Jack Hughston, M.D., with regard to the underdiagnosis of posterolateral corner knee injuries. Hughston stated on many occasions that although you may not have seen posterolateral corner knee injuries (in your practice), “I can assure you that they have seen you.” A lot of work has been performed over the last several years to facilitate the diagnosis and treatment of posterolateral knee injuries. Understanding the anatomy of the posterolateral knee has been a major problem in advancing our treatment of these injuries. For example, different treatment centers call the same structure by different names, which has made it difficult to compare studies performed by different regional or international groups, and has hindered the research progress in the treatment of these injuries. For example, we can understand the dilemma of young clinicians trying to figure out a series of podium presentations at an instructional course lecture or symposium where the presenters discuss the arcuate complex, the arcuate ligament, and the popliteofibular ligament. If these young clinicians were to read the “classic” literature, such as works by Seebacher,1 Hughston,2–5 or Warren’s group,6–11 they would be even more confused about the differences between these structures. In Chapter 2 I review the history of the nomenclature of the posterolateral corner of the knee over the past 250 years and try to resolve most of the confusion about these structures. In fact, quite possibly the only main structures of the posterolateral corner of the knee that have an accurate qualitative description in the literature over this time period are the fibular (lateral) collateral ligament and the popliteus tendon. There have been significant differences in the dissection techniques among many different reporting institutions over time, which has also contributed to this problem. Although it is well recognized that fresh or fresh-frozen cadaveric knee specimens are the most ideal to determine the intricate structures and arrangements of the posterolateral corner of the knee, some earlier studies used formalin-embalmed knees to report on the anatomy of the posterolateral corner of the knee. In addition, most of the studies have dissected the posterolateral corner of the knee from an outside-in approach. Although this is fairly standard for anatomists, physicians at one institution, the Hospital for Special Surgery,7 have noted that the inside-out dissection technique helped them recognize the intricate arrangements of structures of the posterolateral corner of the knee, especially the popliteofibular ligament. In addition, one’s familiarity with dissection techniques facilitates one’s recognition of the arrangement of these structures and one’s recognition of possibly previously undescribed fascial attachments and arrangements. I can state that in my own studies, I have significantly improved my ability to include more quantitative information in my publications over time. I believe much of this is due to experience, as well as to a large clinical practice that has helped me to recognize the important areas to look at anatomically and has helped me repair or reconstruct injuries so that patients can return to their highest level of function. Posterolateral rotatory instability of the knee was first described in 1976 as a clinical entity that caused significant functional limitations in patients.2 However, only in the past 10 to 15 years has the role of posterolateral knee injuries in causing abnormal knee motion become better understood. It has also become increasingly recognized that the incidence of posterolateral knee injuries and the negative effect of untreated injuries on knee function and outcome has been underreported. The anatomy of the posterolateral knee has been recognized as being very complex, and thus the diagnosis of posterolateral knee injuries has been known to be very difficult. In evaluating acute knee injuries, there may be concurrent swelling, effusion, and generalized knee pain, which can make it difficult to recognize a posterolateral corner injury, especially if the examiner does not look for it. In addition, in the presence of other concurrent knee ligament injuries, such as of the anterior cruciate ligament, medial collateral ligament, or posterior cruciate ligament in either the acute or chronic patient, it may be difficult on physical examination to determine the neutral axis point of the knee on the anterior to posterior and medial to lateral planes,2,10,12–15 which can make it difficult to determine on clinical examination whether there is significant injury to the posterolateral structures of the knee. In addition, it has been well recognized that the posterolateral corner of the knee has a variable amount of natural physiologic laxity among patients,16 so it is very important to make sure that the examiner verifies that the increase of motion seen on the injured knee is compared with the natural laxity of the patient’s contralateral normal knee. But when both knees are injured, it can be very difficult to discern the extent of a posterolateral injury. Injuries to the ligaments of the knee are very common, especially in the active adolescent and young adult population. The incidence of overall complete knee ligament injuries17 in the general population is estimated to be 1 per 1000 patients per year.18 Of the more serious knee ligament injuries that require surgery, anterior cruciate ligament tears are the most common with about 2000 per year in Norway19 and 100,000 per year in the United States.20,21 It also has been estimated that the risk of an athlete tearing the anterior cruciate ligament during a competitive season is about 2%.22 The incidence of anterior cruciate ligament tears in Norwegian Team Handball has been found to be 0.9 per 1000 player-hours, with each team having an average of one player sustaining an anterior cruciate ligament tear per year.23,24 Only 50% of these athletes were able to return to full participation at the same level. Although the majority of reconstructions of torn anterior cruciate ligaments do well, there is still some concern that some of these reconstructions fail due to unrecognized or untreated posterolateral knee injuries.21,25–27 Historically, it has been reported that injuries to the posterolateral aspect of the knee occur less frequently than injuries to other knee ligaments. DeLee et al28 noted that in the retrospective study of 735 knee ligament injuries treated in San Antonio, Texas, from 1971 through 1977, 12 patients (1.6%) had isolated acute posterolateral knee injuries, while there were 32 (4.4%) other cases of acute posterolateral knee injuries seen in association with cruciate ligament tears (total incidence, 5.8%). In Danish studies, which have looked at the incidence of knee injuries that present to an emergency room for treatment, the annual incidence of severe posterolateral knee injuries was estimated to be less than 0.1 per 1000 patients. This compared with an incidence of 0.7 for the medial collateral ligament and 0.3 for the anterior cruciate ligament per 1000 inhabitants.18 Miller et al29 reported a 6% incidence of posterolateral knee injuries (30 patients) in a consecutive series of 481 knee magnetic resonance imaging (MRI) scans. However, it has been speculated25,30 that the overall incidence of posterolateral knee injuries has been underestimated and underreported because of the difficulty in diagnosing this complex problem and because examiners do not look for it. Five studies have provided some evidence that this may be true. O’Brien et al25 reported a 15% failure rate in a group of patients who underwent anterior cruciate ligament reconstructions, which appeared to be due to unrecognized or untreated posterolateral instability at the time of their index anterior cruciate ligament reconstruction. However, it is unclear what the total incidence of posterolateral knee injuries was in this population. Fanelli and Edson31 reported that in a consecutive group of 222 patients with a knee hemarthrosis in a level 1 trauma center, 28.4% had posterolateral injuries. Within their group of 222 patients, 85 had posterior cruciate ligament tears, with 53 of these patients (62%) having concurrent posterolateral knee injuries along with their posterior cruciate ligament tears. In addition, with a total of 148 anterior cruciate ligament tears in this group of 222 patients, there were 18 concurrent posterolateral knee injuries in patients with anterior cruciate ligament tears (12%). Another study has reported that in a group of 100 consecutive anterior cruciate ligament reconstructions, the incidence of concurrent posterolateral instability in these knees was shown to be 11%.30 Noyes et al27 reported that in a consecutive series of 41 patients with anterior cruciate ligament tears, varus alignment, and varying amounts of posterolateral instability, 15 patients had a total of 19 previous anterior cruciate ligament reconstructions that had failed. They reported that many of these failures were due to unrecognized posterolateral instability.27 Finally, another study by Noyes et al27 reported that 18 (30%) of 57 patients who underwent a revision anterior cruciate ligament reconstruction using bone-patellar tendon-bone autografts (performed between 1990 and 1996) had untreated or unrecognized posterolateral corner injuries, which appeared to contribute to the index anterior cruciate ligament reconstruction graft failure. These studies would indicate that posterolateral knee injuries have a higher incidence than has been reported and are an important cause of cruciate ligament reconstruction graft failure. It has been recognized in the past that the incidence of posterolateral knee injuries has been underestimated and that prospective studies were needed. In an effort to determine the incidence of posterolateral knee injuries in a prospective manner, we prospectively documented all acute knee injuries that underwent an MRI scan at the major imaging referral center in the Minneapolis-St. Paul metropolitan area. All knees that had been injured within 30 days of the scan were read by a musculoskeletal radiologist who specialized in sports medicine. We found that out of a total 331 consecutive acute knee injuries, 185 (56%) had a ligament injury. Of these 185 patients with a ligament injury, 136 patients (74%) had an anterior cruciate ligament tear, 27 (15%) had a posterior cruciate ligament tear, 72 (39%) had a medial collateral ligament tear, and 30 patients (16%) had a posterolateral corner injury. In this group of 30 patients, there were found to be 18 fibular collateral ligament tears, 17 popliteus tendon tears, and 17 popliteofibular ligament tears documented; 20 (67%) had documented posterolateral knee injuries and other concurrent ligament tears present. Overall, 9.1% of patients who presented to the imaging center for evaluation were found to have a posterolateral knee injury. Although it can be argued that MRI may not be as accurate as a good physical examination in the documentation of posterolateral corner injuries, it can also be argued that it is very difficult to obtain a large population of patients with acute knee injuries at a sports medicine referral center without some referral bias. I performed this study because I felt a large MRI study with all the acute knee injuries that presented to a major MRI referral center would provide as close as possible the actual number of posterolateral knee injuries that occur in the general population. In summarizing the various different incidence studies that have included posterolateral knee injuries, it would appear that the incidence of posterolateral knee injuries is between 5% and 9%. Thus, it appears that the actual incidence of posterolateral knee injuries has been underestimated in the past. It is hoped that with an improved understanding of how to diagnose these complex injuries, more injuries will be recognized in the acute time frame and treated before they progress to chronic injuries. One of the most important things to recognize about grade 3 posterolateral corner injuries is that a failure to diagnose them in the acute injury phase results in a chronic injury, which often leads to significant functional limitations during minor activities, to meniscal tears,30 and to a high incidence of arthritis over time if they are not treated.2,32–34 It has been hypothesized that untreated posterolateral corner injuries do not heal because the two opposing convex surfaces of the lateral compartment of the knee have an inherent bony instability35,36 (Fig 1-1). Unlike the medial compartment of the knee, where isolated injuries to the medial collateral ligament complex usually heal without any residual or functional laxity, in part because the concave surface of the medial tibial plateau articulates with the convex surface of the medial femoral condyle and provides an inherent amount of bony stability to the medial compartment,37 the relatively convex surfaces of the lateral tibial plateau and lateral femoral condyle result in increased motion due to the inherent bony instability after a posterolateral corner injury, which can lead to residual knee laxity as the injured structures either do not heal or heal in a nonfunctional elongated position.35 Also, it is well recognized that the results of an acute repair of a posterolateral corner injury are far superior to that of a chronic reconstruction.4,28,30,38,39 With this information in mind, the examiner must be vigilant and listen to patients’ description of their mechanism of injury, as well as perform a thorough clinical examination to test the integrity of all ligaments of the knee when a ligament injury is suspected, so as not to miss an acute posterolateral corner injury. The consequences to the patient of a missed acute posterolateral corner injury can be significant, due to the poorer outcomes and more extensive surgery required to treat chronic rather than acute posterolateral knee in juries.2,4,30,38,39
Introduction and Incidence of Posterolateral Knee Injuries
Introduction and Incidence of Posterolateral Knee Injuries
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








