5 The portions of the physical examination that are useful for the diagnosis of posterolateral knee injuries are the external rotation recurvatum test, varus stress test at 30 degrees, dial test at 30 and 90 degrees, posterolateral drawer test, reverse pivot shift test, and an evaluation for a varus thrust gait.1–8 Although many clinicians become skilled in the diagnosis of cruciate ligament injuries and develop a qualitative feel for knee laxity, the clinical examination assessment is still largely subjective, and its overall reliability depends on the skill and experience of the examiner. Because posterolateral knee injuries are commonly associated with other ligamentous injuries and may be missed at the time of the initial evaluation,9–11 the injured knee should also be examined for ecchymosis, swelling, or tenderness over the posterolateral structures of the knee, especially for acute knee injuries. In addition, due to an approximate 15% incidence of associated common peroneal nerve injuries with posterolateral knee injuries, it is important to assess for the motor and sensory function of this nerve during the clinical examination of acute knee injuries.11–13 The external rotation recurvatum test assesses for increased genu recurvatum and relative genu varus4 (Fig. 5-1). In this test, the patient lies supine on the examining table while the examiner lifts up the patient’s great toe. It is important to compare the amount of recurvatum of the injured knee to the contralateral normal knee. A positive external rotation recurvatum test, where there is increased recurvatum and a relative varus position of the injured knee, usually indicates a combined cruciate ligament injury in addition to a posterolateral knee injury. In our experience, this usually means that a concurrent anterior cruciate ligament (ACL) tear is present. The varus stress test is performed with the patient supine and the leg over the side of the examining table with the knee flexed to 30 degrees1 (Fig. 5-2). A varus stress is applied to the knee through the foot/ankle, while the examiner’s fingers palpate for the amount of lateral joint line opening. Due to physiologic variations in the amount of normal lateral joint line opening, it is important to compare the amount of lateral joint line opening of the injured knee to the contralateral knee. The American Medical Association guidelines14 for grade I (0–5 mm), grade II (6–10 mm), and grade III (> 1 cm) joint line opening, compared with the normal contralateral knee, are followed to assess the severity of the posterolateral knee injury (Table 5-1). It is important to recognize that increased varus opening will not be present without a concurrent injury to the fibular collateral ligament.6,15–20 Figure 5-1 The external rotation recurvatum test. The examiner lifts the patient’s great toe and assesses for an increased amount of knee recurvatum (A) and relative varus (B) compared with the normal contralateral knee. (From LaPrade RF, Terry GC. Injuries to the posterolateral aspect of the knee. The dial test assesses for an increased amount of external rotation of the tibia on the femur at 30 degrees (Fig. 5-3). This test can be performed with the patient in either the supine or prone position; the amount of external rotation of the tibia compared with the femur in the injured knee is compared with that in the contralateral normal knee.21,22 An external rotation force is applied to the foot to determine the presence of increased rotation of the tibia on the femur compared with that in the normal contralateral knee. Visualization of the difference in rotation of the tibial tubercle is the best way to assess this study in the supine patient. Although this test has been found to be very specific in identifying posterolateral knee injuries in biomechanical sectioning studies,6,18–20 it is a very subjective test that relies on subtleties in the physical examination. I believe that this makes the dial test one of the least useful tests clinically because it demonstrates relatively minor (10–15 degrees) visual changes in external rotation. In performing this test, it is very important to compare the increased external rotation of the injured knee to the normal contralateral knee. In a group of 30 normal volunteers who had their amount of tibial rotation calculated with a measurement device, the mean side-to-side difference between normal knees was 5.5 degrees at 30 degrees and 4.4 degrees at 90 degrees.7 An increase in external rotation of 10 to 15 degrees of the knee at 30 degrees is considered to be due to a posterolateral knee injury6,19,20,23 (Table 5-2). Figure 5-2 The varus stress test at 30 degrees. The examiner applies a varus force through the foot/ankle with one hand, while the other hand stabilizes the patient’s knee and the examiner’s fingers palpate to assess the amount of lateral joint-line opening. (A) Neutral position. (B) Varus force applied.
Clinical Examination of Posterolateral Knee Injuries


| AMA Grade | Amount of Varus Opening | Severity of Injury |
| I | 0–5 mm | Mild |
| II | 6–10 mm | Moderate |
| III | > 1 cm | Severe |
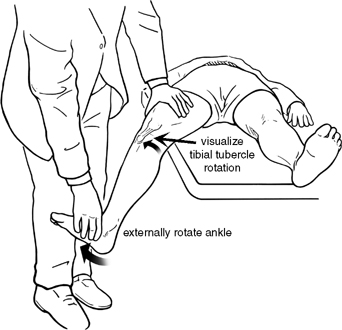
Figure 5-3 The dial test at 30 degrees of knee flexion. An external rotation force is applied to the knee and the amount of external rotation of the tibia, compared with the femur, is qualitatively measured by observing for differences in rotation of the tibial tubercles between the injured and normal contralateral knee.
In an isolated posterolateral knee injury, there should be a decrease in the amount of external rotation at 90 degrees compared with that found at 30 degrees.6,20,24 The amount of increased external rotation seen at 90 degrees of knee flexion compared with the contralateral normal knee with an isolated posterolateral knee injury should be 5 to 7 degrees.20,25 However, if there is a concurrent posterior cruciate ligament (PCL) tear, there will be an increase in external rotation at 90 degrees.20,26 In addition, with a concurrent ACL tear, there also appears to be a similar increase in external rotation at 90 degrees with a combined posterolateral knee injury, which averages 15 degrees compared with the contralateral normal knee.27 Therefore, an increase of external rotation clinically seen on the dial test at 90 degrees of knee flexion can be due to either a concurrent ACL or PCL injury (Fig. 5-4).
| Grade | Degrees of Increased External Rotation | Severity of Injury |
| I | 0–5 degrees | Mild |
| II | 6–10 degrees | Moderate |
| III | > –10 degrees | Severe |
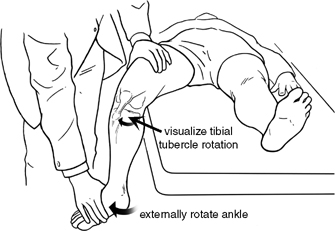
Figure 5-4 The dial test at 90 degrees. An external rotation force is applied to the foot/ankle and the amount of rotation of the tibial tubercle is observed. For an isolated posterolateral knee injury, the amount of increased external rotation averages between 5 and 7 degrees. An increase in external rotation to between 10 and 15 degrees would indicate a probable concurrent posterior or anterior cruciate ligament tear and a c ombined posterolateral knee injury.
The posterolateral drawer test4 is performed at 90 degrees of knee flexion with the foot externally rotated 15 degrees (Fig. 5-5). A posterolateral force is applied to the knee to assess for an increase in knee joint motion. An increase in a combined, coupled posterolateral rotation compared with the normal contralateral knee is indicative of a posterolateral knee injury. It is important clinically to differentiate this test from the posterior drawer test in neutral rotation, which primarily assesses the integrity of the posterior cruciate ligament4 (Table 5-3).

Figure 5-5 The posterolateral drawer test. In this test, the knee is flexed to 90 degrees and the foot is externally rotated to 15 degrees. The examiner applies a gentle posterolateral rotation force to the knee and the amount of posterolateral rotation of the tibia on the femur is qualitatively measured compared with the normal contralateral knee. (A) Neutral position. (B) Posterolateral drawer applied.
| Grade | Sprain Type | Clinical Findings |
| Grade I | Minor sprain | Minimal increase in varus translation, external rotation at 30 and 90 degrees, and posterolateral drawer at 90 degrees |
| Grade II | Moderate sprain | An increase of varus less than 1 cm (compared with the contralateral side) with a palpable end point; an increase of external rotation at 30 degrees less than 10 degrees; an increase in posterolateral drawer no more than one grade compared with the contralateral side |
| Grade III | Severe sprain | Greater than 1 cm of varus opening at 30 degrees; a 10-degree increase of external rotation at 30 degrees compared with the contralateral side; a one to two grade increase in the posterolateral drawer test at 90 degrees compared with the contralateral side |
The reverse pivot shift test5 is a dynamic test to assess for posterolateral rotation of the tibia on the femur (Fig. 5-6). I consider it to be a dynamic variant of the posterolateral drawer test. This test has been noted to have the most variability of all motion tests and has been found to be positive in 35% of normal knees examined under anesthesia.21 In this test, the knee is flexed to 70 to 90 degrees and the foot is externally rotated. The knee is then slowly extended and observed to see if a reduction of a posterolaterally subluxed tibia occurs on the femur. The reverse pivot shift test is considered to be positive when a noticeable reduction of the tibia occurs on the femur. Due to the large physiologic variability among patients with a normal knee and a positive reverse pivot shift test, especially in patients with physiologic genu recurvatum, the test leg itself is rarely useful to determine the presence of a posterolateral knee injury in isolation.
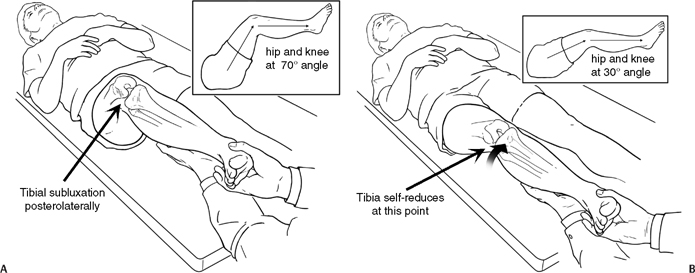
Figure 5-6 The reverse pivot shift test. (A) The knee is flexed to between 70 and 90 degrees and the foot is externally rotated, which would result in posterolateral subluxation of the tibia on the femur. (B) The knee is then extended while the knee is observed for a reduction of the posterolaterally subluxed tibia on the femur at about 30 degrees.
Tears of the popliteomeniscal fascicles can result in lateral meniscal hypermobility and entrapment of the lateral meniscus in the joint with application of a varus stress. Patients who present with this pathology often complain of vague lateral joint knee pain, and MRI scans are often inconclusive. In these patients, the figure-four test, where the ipsilateral foot is placed over the contralateral knee, has been found to be an accurate method to diagnose popliteomeniscal fascicle tears with resulting lateral meniscal entrapment.28
In addition to these clinical tests specific for the assessment of posterolateral knee injuries, it is important to assess for increased amounts of anterior tibial translation on the Lachman test. The increased posterior translation seen at 30 degrees with a posterolateral knee injury,6,20,24 as well as the increase in anterior translation seen with posterolateral structure injury in the face of a concurrent ACL tear,19,24,27 may be detected clinically as increased anterior translation in both an ACL-intact (a “pseudo-Lachman” test) and ACL-deficient knee with the Lachman test. If there is a solid end point present (in an ACL-intact knee) with increased anterior translation on the Lachman test, one should be suspicious of a possible underlying posterolateral knee injury with its associated increase in posterior translation in early flexion.6,20,24,29 Thus, a positive pseudo-Lachman test may be positive with either a concurrent PCL or posterolateral knee injury (or both). It is also important to recognize that a significant increase in anterior translation in an ACL-deficient knee on the Lachman test of the injured knee may signify an underlying posterolateral knee injury. In those knees that have an ACL tear, a 3+ or 4+ Lachman test, and an intact PCL and posterior horn of the medial meniscus, one should assume that a posterolateral knee injury has to be ruled out of the clinical diagnosis.
In addition, posterior translation of the knee in neutral rotation should be carefully assessed. If posterior translation of the knee is slightly increased at 30 degrees, but near normal at 90 degrees (with a negative or trace positive quadriceps active test),30 then a posterolateral knee injury (with an intact PCL) should be suspected. If posterior knee translation in neutral rotation at 90 degrees is also significantly increased, then in addition to a PCL injury, a combined posterolateral corner injury should also be suspected.6,20 It is becoming increasingly recognized that most isolated PCL tears result in <1 cm of increased posterior translation with a clinical posterior drawer test of 1+ to 2+. In a knee with a 3+ posterior drawer test or for which ≥12 mm of increased posterior translation is seen on stress radiographs, one must rule out a combined posterolateral and PCL tear.
In addition to these clinical tests for abnormal joint motion, it is also important to assess for any potential motor or sensory deficits of the common peroneal nerve. This would include an assessment of sensation in the first dorsal web space and dorsal and lateral aspect of the foot and an assessment of motor strength of the extensor hallucis longus, extensor digitorum longus, and ankle dorsiflexors and evertors.
Finally, a patient should be assessed for the presence of a varus-thrust gait with ambulation.8,31–33 In patients with this gait abnormally, a varus thrusting occurs due to a high adduction moment as the ligamentous-deficient lateral compartment opens up at foot strike during the stance phase of the gait cycle. With further ambulation, the dynamic action of the biceps femoris and a shift of the center of gravity of the body with a forward gait stride help to close down the increased varus opening of the lateral compartment. As it closes down, a visible shift (thrust) of the affected knee is seen. Patients can sometimes adapt and prevent this gait abnormality by ambulating with a flexed knee gait,33 which helps to decrease abnormal lateral compartment opening in a posterolateral deficient knee. Although most of these patients have an underlying varus alignment of their knees that contributes to this instability, not all patients have an underlying genu varus alignment.
♦ Radiographic Evaluation of Posterolateral Knee Injuries
Plain radiographs of a knee with a posterolateral knee injury may show a Segond fracture34 (Fig. 5-7), arcuate fracture35 (Fig. 5-8), or abnormal widening of the lateral compartment joint space.8 In addition, patients with chronic posterolateral knee injuries may have degenerative changes of the medial compartment. 3,36 Anteroposterior (AP) varus-thrust radiographs have also been noted to be helpful in demonstrating the amount of increased lateral joint line opening, but are not routinely done as part of initial radiographic screening8 (Fig. 5-9).
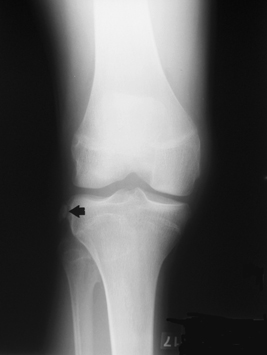
Figure 5-7 Anteroposterior (AP) radiograph demonstrating a Segond avulsion fracture (arrow) of the meniscotibial portion of the mid-third lateral capsular ligament and the anterior arm of the short head of the biceps femoris off the tibia (right knee).
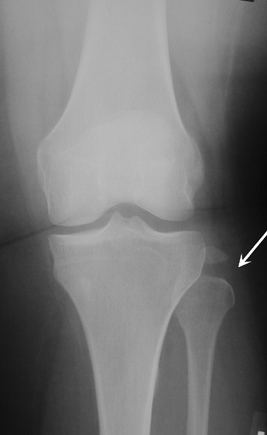
Figure 5-8. An AP radiograph demonstrating an “arcuate” avulsion fracture of the fibular styloid (left knee).
Other radiographs that can be useful to assess the extent of a posterolateral corner injury include bilateral PCL stress radiographs. It has been noted that isolated complete PCL tears usually have an 8- to 10-mm side-to-side difference in posterior knee translation on stress radiographs. In these cases in which the amount of posterior translation increases to > 12 mm, then one should suspect a probable concurrent posterolateral (or potential posteromedial) knee injury (Fig. 5-10).
Although a Segond fracture34 has been described to be pathognomonic for an ACL tear,37 it has also been noted to be present in the face of posterolateral knee injuries.11,38 Originally described to be an avulsion of a fleck of bone off the proximolateral tibia with its attached lateral capsule,34,37,39 it has since been found frequently to have also the anterior arm of the short head of the biceps femoris attached to the avulsed tissues.40 I have found in some instances that Segond fractures, or Segond soft tissue avulsion injury variants, are much larger and sometimes contain the entire lateral capsular attachments in the face of a posterolateral knee injury.










