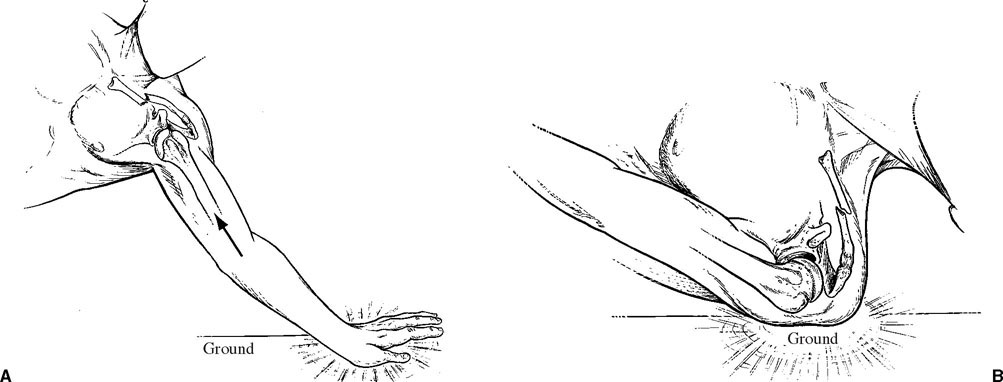
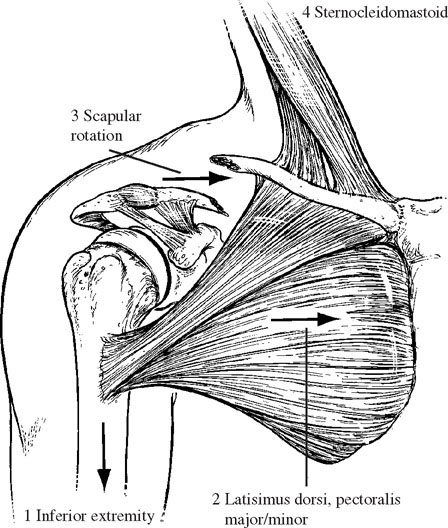
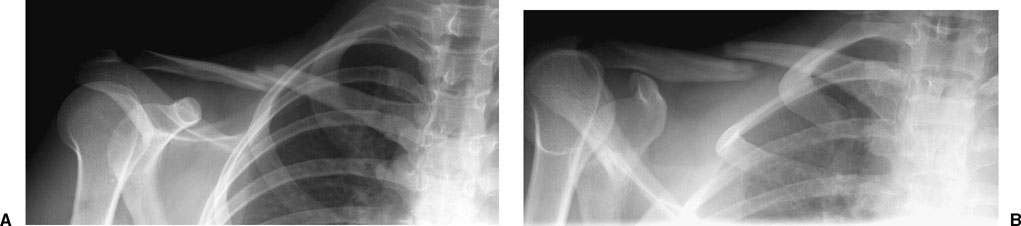
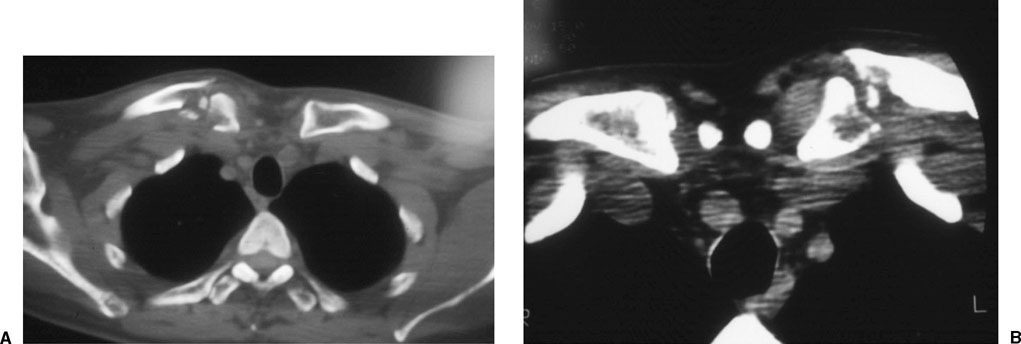
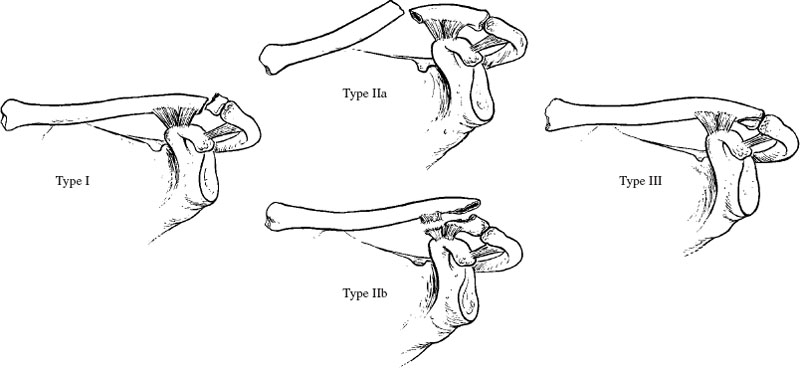
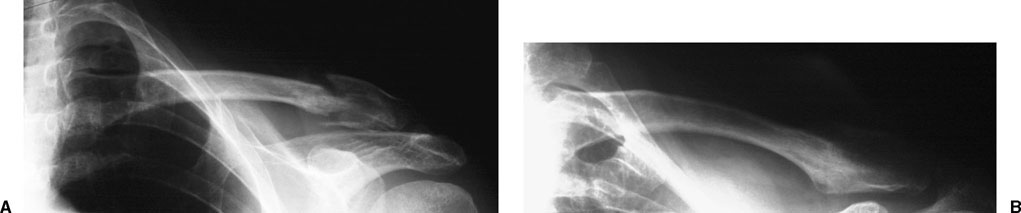
Clavicle fractures account for 2.6 to 12% of all fractures, and 44 to 66% of fractures about the shoulder.1,2 The annual incidence of these injuries is around 50 per 100,000.3 These fractures often occur as a result of an indirect mechanism, specifically a fall onto an outstretched upper extremity, usually resulting in a middle-third fracture. The direct mechanism, a fall directly onto the shoulder, occurs much less commonly and is usually associated with a fracture of the lateral end of the clavicle.4 Postacchini et al1 in 2002 reported on 535 clavicle fractures and observed that 68% of clavicle fracture occurred in males, and most fractures occurred in individuals younger than 20 years old; 81% of the fractures occurred in the middle third of the clavicle, 48% were displaced, and 19% were comminuted. Overall, middle-third fractures account for 80% of all clavicle fractures, whereas fractures of the lateral and medial third of the clavicle account for 15% and 5%, respectively. The prevalence of displaced clavicle fractures increases with age. In adults, clavicle fractures are more disabling and carry a higher incidence of complications because of the greater force required to produce them.2,4 The most common mechanism of injury for this fracture is a fall onto the outstretched hand or a direct blow to the clavicle (Fig. 10-1). Most of these injuries are the result of moderate to high-energy trauma in adolescents and adults; in elderly patients they are often the result of low-energy trauma. The clavicle most commonly fails in compression as a result of axial forces that occur as the patient falls onto the point of the shoulder or the outstretched hand.5 Stanley et al5 found that of 150 consecutive patients with clavicle fractures, 122 specifically recalled falling onto an outstretched upper extremity or directly onto the shoulder. Patients who present with clavicle fractures as a result of high-energy trauma should be evaluated by the protocol advocated by the American College of Surgeons; in all cases, life-threatening injuries must take precedence over the clavicle injury. Most patients, regardless of the mechanism of injury, describe pain in the area of the fracture and increased pain with any attempted shoulder or upper extremity motion. Clavicle fractures can usually be identified by visual inspection because of its subcutaneous location, its prominence in forming the contour of the shoulder girdle, and the prevalence of the displaced pattern. Most patients present with swelling and tenderness about the area of the fracture. They typically resist shoulder movement and tend to maintain the upper extremity at the side in an adducted, “protected” position. Fracture displacement is usually evident, and the ends of the fracture fragments are frequently palpable. The condition of the overlying skin must be carefully evaluated to be certain the fracture is closed or that there is no impending skin compromise as a result of displaced fragments. Open fractures are very uncommon and require emergency management. Tenting of the skin is most often found in association with displaced middle-third and lateral-third fractures. For middle-third fractures, the superiorly displaced medial fragment (as a result of the pull of the sternocleidomastoid muscle) can stretch the overlying skin (Fig. 10-2); comminuted fragments, especially if rotated, can cause further skin compromise. For lateral-third fractures the superior displacement of the medial fragment can tent the skin (Fig. 10-3A). This is further compromised by the skin abrasion that is often found in association with these injuries when the fractures result from a fall off a bicycle or motorcycle (Fig. 10-3B). FIGURE 10-1 Clavicle fractures can occur as a result of an indirect (A) or direct (B) mechanism. Medial-third fractures are usually nondisplaced and, consequently, are not as evident on examination as displaced lateral- or middle-third fractures. As a result, skin compromise is not usually a concern. FIGURE 10-2 Midshaft clavicle fractures typically result in prominence at the fracture site, which corresponds to the lateral end of the medial fragment. The lateral fragment is usually displaced inferiorly by the weight of the upper extremity (1) and medially by the pull of the latissimus dorsi and pectoralis muscles (2) and the unopposed rotation of the scapula (3). The medical fragment is displaced superiorly by the unopposed pull of the sternocleidomastoid (4). Palpation of the area of the fracture produces tenderness. Active shoulder range of motion is significantly limited by pain. Assisted or passive range of motion is painful and can produce crepitus at the fracture site. The proximity of the clavicle to the neurovascular structures makes a thorough neurovascular examination mandatory (Fig. 10-4). This is particularly true of middle-third fractures and those that occur as a result of high-energy trauma. A thorough assessment of the brachial plexus and the distal pulses (brachial artery, ulnar artery, and radial artery) should be performed and the results documented. If there is a concern about vascular compromise, a prompt vascular consult should be obtained. The remainder of the upper extremity should be carefully examined to identify other injuries. In addition, the possibility of an associated thoracic injury (rib injuries, pneumothorax, and hemothorax), although very uncommon, should be considered based on the mechanism of the injury and the clinical findings. Initial evaluation of the patient with a suspected clavicle fracture should include a standard trauma series. The anteroposterior (AP) chest radiograph should include the entire clavicle and acromioclavicular (AC) and sternoclavicular (SC) joints. It should be carefully evaluated for evidence of a thoracic cage injury. Standard AP radiographs are generally sufficient to confirm the presence of a clavicle fracture and the degree of fracture displacement (Fig. 10-5A). The film should include the AC joint and the SC joint, as well as the proximal humerus and apices of the lung. Special views can assist in the identification and characterization of clavicle fractures. A 20 to 60° cephalad tilt view provides an image without the overlap of the thoracic anatomy (Fig. 10-5B).6,7 An apical oblique view can be helpful in diagnosing minimally displaced fractures, especially in children. This view is taken with the involved shoulder angled 45° toward the x-ray source, which is angled 20° cephalad. Standard radiographs may be inadequate to properly identify medial-third clavicle fractures and intraarticular lateral-third fractures. In these situations, a computed tomography (CT) scan should be obtained (Fig. 10-6), not only to identify the presence of the fracture but also to understand the fracture pattern and the degree of intraarticular involvement. FIGURE 10-3 Lateral-third clavicle fractures have a characteristic appearance that can resemble complete acromioclavicular joint separations (A). When the mechanism of injury involves a fall onto the shoulder, a skin abrasion often results (B). FIGURE 10-4 The clavicle lies in close proximity to the neurovascular structures that supply the ipsilateral upper extremity. In 1967 Allman8 described the following classification system for all clavicle fractures based on location: Group I represented fractures of the middle third, which was the most frequent site of fracture (80%). The proximal and distal ends of the clavicle are secured by the intact ligamentous and muscular attachments. These fractures can then be further described based on fracture pattern, degree of shortening (overriding), and the degree of displacement, although these parameters were not part of Allman’s original description. Displacement and comminution are important parameters that should be included in the description of middle-third fractures because of their implications for treatment and prognosis. Group II represented fractures of the lateral third. These were further subclassified by Neer into three types based on the degree of displacement and the location of the fracture with respect to the coracoclavicular ligaments (Fig. 10-7): Type I: minimal displacement; these fractures occur between the conoid and trapezoid ligaments or between the coracoclavicular and AC ligaments; the intact ligaments maintain the fragments in position, thereby limiting displacement Type II: displaced; these fractures occur medial to the coracoclavicular ligaments, thereby allowing the medial fragment to displace superiorly Type III: intraarticular; these fractures involve the articular surface of the lateral clavicle FIGURE 10-5 (A) An anteroposterior radiograph is usually sufficient to identify the majority of clavicle fractures. (B) A20 to 60° cephalic tilt view provides a clearer image by minimizing overlap with thoracic anatomy. Subsequent to Neer’s description, Rockwood further subclassified type II fractures into two subtypes: Type II A: conoid and trapezoid ligaments remain attached to the distal fragment Type II B: conoid ligament disrupted and the trapezoid ligament remains attached to distal fragment Group III fractures, as described by Allman, represented medial-third fractures. These were the least common sites of clavicle fracture. Craig described a classification (Table 10-1) that combined the Allman and Neer fracture types and expanded the description of the fractures and included less common injuries (i.e., epiphyseal separations). This system is particularly useful to describe and classify medial-and lateral-third fractures; however, it does not provide a detailed classification of middle-third fractures. In 1998, after reviewing 1000 consecutive clavicle fractures, Robinson proposed a new classification system (Table 10-2) that incorporated important prognostic factors including displacement, comminution, and intraarticular involvement (Fig. 10-8). Although this classification system includes almost all clavicle fractures, it has not yet been used extensively. This may be due, in part, to the numbering system, which is different from that described by Allman and Neer. In the Robinson system, lateral-third fractures are type III, middle-third fractures are type II, and medial-third fractures are type I. FIGURE 10-6 (A,B) Computed tomography (CT) scans aid in the diagnosis of intraarticular fractures of the medial third of the clavicle as shown here in these two examples. In 1991 the Orthopaedic Trauma Association (OTA) adopted the AO/Association for the Study of Internal Fixation (ASIF) comprehensive fracture classification system originally described in the 1970s and expanded it to include fractures of the spine and distal extremities. Fractures of the clavicle are included in this comprehensive system and are classified based on location and displacement. Regardless of the classification system utilized, it is essential to understand the fracture pattern and anatomy and to effectively describe the fracture so that treatment outcomes can be accurately documented and compared. FIGURE 10-7 The Neer classification of lateral clavicle fractures.
Clavicle Fractures
 History
History
 Clinical Evaluation
Clinical Evaluation
Radiographic Evaluation


 Classification
Classification
| Group I: Fractures of the middle third | |
|---|---|
| Group II: Fractures of the distal third | |
| Type I | Minimal displacement (interligamentous) |
| Type II | Displaced secondary to fracture line medial to the coracoclavicular ligaments (A) Conoid and trapezoid attached (B) Conoid torn, trapezoid attached |
| Type III | Fractures of the articular surface |
| Type IV | Periosteal sleeve fracture (children) |
| Type V | Comminuted with ligaments attached neither proximally or distally, but to an inferior comminuted fragment |
| Group III: Fractures of the proximal third | |
| Type I | Minimal displacement |
| Type II | Displaced (ligaments ruptured) |
| Type III | Intraarticular |
| Type IV | Epiphyseal separation (children and young adults) |
| Type V | Comminuted |
 Treatment
Treatment
The vast majority of clavicle fractures can be successfully treated nonoperatively with some form of immobilization. Various methods of immobilization have been described including: an arm sling (Fig. 10-9A), a sling and a swath (Fig. 10-9B), a figure-of-eight bandage (Fig. 10-9C,D), or shoulder spica.9,10 The goals of the various methods of immobilization are to (1) support the shoulder girdle, raising the lateral fragment in an upward, outward and backward direction; (2) depress the medial fragment; (3) maintain some degree of fracture reduction; and (4) allow for the patient to use the ipsilateral hand and elbow. Regardless of the method of immobilization utilized, some degree of shortening and deformity are the usual sequelae. We prefer to immobilize most clavicle fractures with a simple sling (and swath if necessary), accepting that some degree of deformity is very unlikely to lead to long-term sequelae (these are discussed later, in the section on complications). A figure-of-eight bandage is sometimes helpful for reducing displaced fractures that are associated with skin problems; however, the location of the padded bandage must not be over the area of potential skin compromise.
| Type 1: Medial | |
|---|---|
| A | Nondisplaced |
| A1 | Extraarticular |
| A2 | Intraarticular |
| B | Displaced |
| B1 | Extraarticular |
| B2 | Intraarticular |
| Type 2: Middle | |
| A | Cortical alignment |
| A1 | Nondisplaced |
| A2 | Angulated |
| B | Displaced |
| B1 | Simple or single butterfly fragment |
| B2 | Comminuted or segmental |
| Type 3: Distal | |
| A | Nondisplaced |
| A1 | Extraarticular |
| A2 | Intraarticular |
| B | Displaced |
| B1 | Extraarticular |
| B2 | Intraarticular |
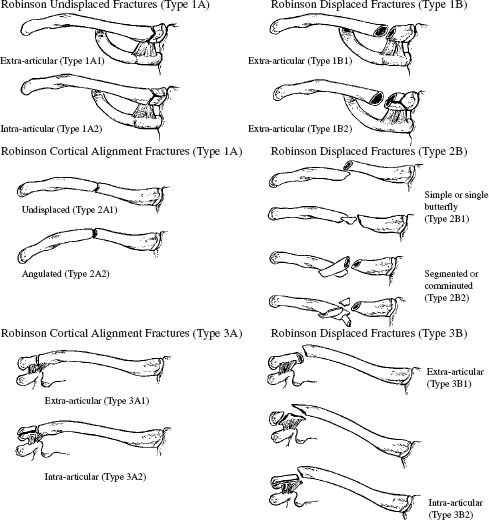
FIGURE 10-8 The Robinson classification of clavicle fractures.
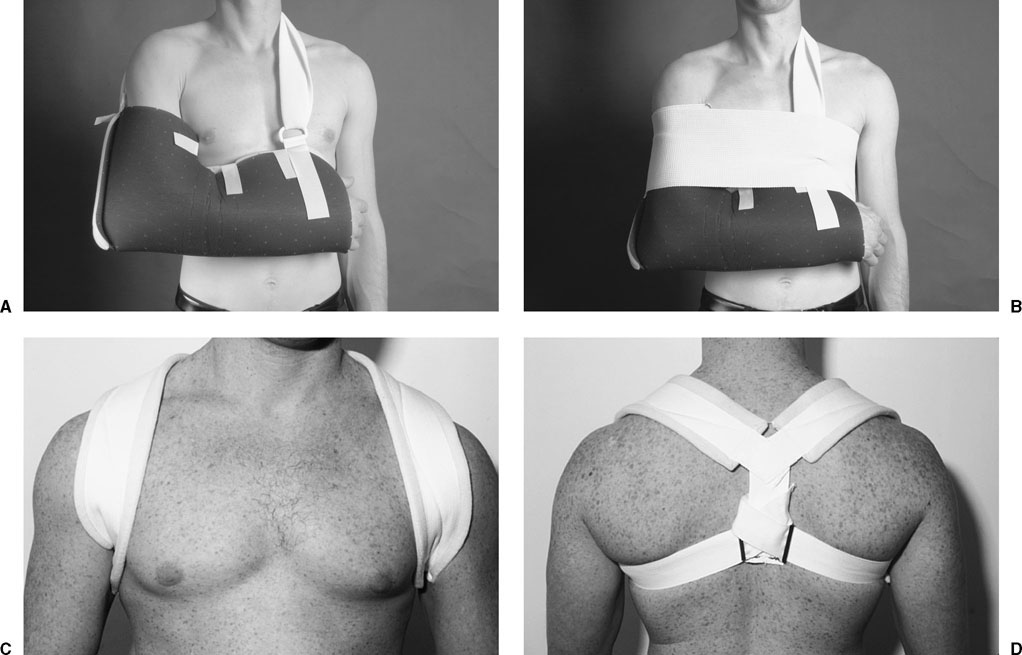
FIGURE 10-9 Immobilization methods include simple sling (A), sling and swath (B), and figure-of-eight bandage (C,D).
In 1981 Zenni et al,11 after reviewing the literature, described the following indications for open reduction and internal fixation of clavicle fractures: (1) neurovascular compromise due to posterior displacement and impingement of the bony fragments on the brachial plexus, subclavian vessels, or even the common carotid artery; (2) widely displaced fracture of the lateral third of the clavicle with disruption of the AC ligaments; (3) severe angulation or comminution of a fracture in the middle third of the clavicle; (4) the patient’s inability to tolerate prolonged immobilization; and (5) symptomatic nonunion following nonoperative treatment.
Lateral-Third Fractures
Nonoperative treatment of lateral-third clavicle fractures is appropriate for type I and type III injuries. Type II injuries are analogous to AC joint separations. Closed treatment should be reserved for those injuries with limited displacement and no evidence of skin compromise. The method of treatment appropriate for these fractures depends on the location of the fracture relative to the AC ligaments. This was the impetus for Neer’s classification system and treatment recommendations.

FIGURE 10-10 Type I lateral clavicle fracture showing minimal displacement.
Type I
The ligaments are intact in type I clavicle fractures, and displacement is therefore generally minimal (Fig. 10-10). We treat these patients with a sling for comfort and begin mobilization as pain permits. Patients typically require a sling for 3 to 4 weeks. Active assisted range of motion of the shoulder is started as the patient is able to tolerate; forward elevation of the shoulder is limited to less than 90° for the first 2 weeks and then advanced as described previously.
Type II
The most important parameter determining the treatment of type II lateral clavicle fractures is the degree of displacement. Some authors have indicated that all type II fractures require operative management. In our experience, all type II fractures do not require operative treatment. We have found that if the bone ends are in contact, healing can be expected even if there is some degree of displacement. In this situation, nonoperative management consisting of sling immobilization and progressive range of motion as described can result in healing of the fracture with a satisfactory functional outcome (Fig. 10-11). When there is significant displacement such that the bone ends are not in contact, operative management is indicated. Of course, the decision to proceed with operative management is made based on a careful consideration of patient factors as well. In most situations, however, when there is wide displacement of type II lateral clavicle fractures, operative management is indicated.
A variety of techniques have been described for the operative management of type II lateral clavicle fractures, which primarily consist of reducing the medial fragment to the lateral fragment. This is accomplished by using either coracoclavicular fixation (Fig. 10-12) or fixation across the AC joint, through the lateral fragment, and into the medial fragment (Fig. 10-13). Although both AC and coracoclavicular techniques have been used successfully, we prefer the coracoclavicular method primarily because it avoids compromise of the AC joint and does not require a second procedure for hardware removal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





