Fractures of the scapula are relatively uncommon injuries representing about 0.5 to 1.0% of all fractures and only 3 to 5% of shoulder fractures.1 Due to the uncommon nature of these injuries, experience in the management of scapula fractures has been limited. Scapula fractures are usually the result of high-velocity blunt trauma and often present in the setting of polytrauma. Peak incidence is in males between the ages of 30 and 40 years.2–7 Scapula fractures are commonly the result of motor vehicle accidents (MVAs) and high-energy falls.2–8 The most common location of scapula fractures is the body, followed by the neck, glenoid, and then acromion.2–7 Thirty percent of fractures may have intraarticular involvement.9 Three important factors—soft tissue coverage, mobility, and location—enable the scapula to be relatively resistant to fracture. A significant amount of protection is provided by the thick, muscular, soft tissue envelope surrounding the scapula (see Fig. 2-8 in Chapter 2). The scapular and periscapular muscles provide a soft tissue cover that helps dissipate forces imparted to the scapula by the specific mechanisms of injury. The mobility provided by the scapulothoracic articulation enables injury forces to be dissipated to adjacent structures. Its axial location, as opposed to an appendicular location, posterior to the thoracic cage further adds to its relative resistance to injury. In this location, it is not subjected to bending or torsional forces, which are the most common mechanisms of fracture in the appendicular skeleton. Due to its relatively protected anatomy and mobility of the scapula, injuries to the scapula require a high-energy mechanism and frequently occur as part of a constellation of injuries of the ipsilateral thoracic cage that can include rib fractures and severe pulmonary injuries. The most important aspect in the management of scapular fractures is the prompt recognition of associated injuries to the ipsilateral lung, chest wall, thoracic cage, and shoulder girdle, which are reported to occur in greater than 80% of scapular fractures.2–6,8 Concomitant injuries include intrathoracic and thoracic wall injuries, brachial plexus injuries, vascular injuries, and scapulothoracic dissociation (Table 11-1). A scapular fracture with a concomitant first rib fracture is a particularly serious injury pattern because of its association with pulmonary and neurovascular compromise.3 The most extreme example of an ipsilateral shoulder girdle injury is a scapulothoracic dissociation, which warrants special mention. It is the anatomic equivalent of a closed forequarter amputation and is the result of violent, high-energy, blunt trauma that disrupts all static and dynamic stabilizers of the shoulder girdle (Fig. 11-1).10 Osseous or ligamentous injuries lead to disruption of the acromioclavicular (AC) and sternoclavicular joints. The dynamic stabilizers are injured due to complete or near-complete tears of the deltoid, pectoralis, and periscapular musculature. Vascular disruption and brachial plexus avulsion is common.11 The extremity is often flail, insensate, and pulseless. Fortunately, this devastating, life-and limb-threatening injury is rare. These associated injuries have far greater significance than the scapula fracture in the initial evaluation and management of these patients. The scapula is a flat, triangular bone enveloped in layers of muscle. The scapula and the complex of muscles that surround it provide a critical role in the mechanics and kinematics of the shoulder girdle. It is the origin of the rotator cuff muscles, deltoid muscle, biceps, and the long head of the triceps. It also is the site of insertion for the trapezius, levator scapulae, rhomboids, serratus anterior, and pectoralis minor, all of which hold the contoured scapula against the posterior chest wall (see Fig. 2-1 in Chapter 2). Through its three true joints and one muscular articulation, it is not only the sole link between the upper extremity and the axial skeleton, but also a mobile platform upon which the proximal humerus is balanced as the upper extremity moves. Various ligaments originating from the scapula serve as important static stabilizers of the shoulder girdle. The coracoclavicular (CC) ligaments prevent superior migration of the distal clavicle to stabilize the AC articulation. The joint capsule, glenohumeral ligaments, and coracohumeral ligaments stabilize the glenohumeral joint in various directions and arm positions, whereas the coracoacromial ligament serves as a superior static restraint to humeral head stability.
Scapula Fractures
 Relevant Anatomy
Relevant Anatomy
| Associated Injuries | Incidence (%) |
|---|---|
| Rib fractures | 27–54 |
| Pulmonary contusion | 11–54 |
| Clavicle fractures | 23–39 |
| Pneumothorax | 11–38 |
| Brachial plexus injuries | 5–13 |
| Vascular injuries (usually subclavian or axillary vessels) | 1 |
| Scapulothoracic dissociation | <1 |
Goss12 has introduced the concept of the superior shoulder suspensory complex (SSSC) to emphasize the function of the scapula in maintaining the normal stable relationship between the shoulder girdle/upper extremity and the axial skeleton. The scapula is suspended from the lateral end of the clavicle by the CC and AC ligaments. These are the only fixed attachments of the scapula to the axial skeleton. The SSSC is a ring composed of the glenoid, coracoid process, CC ligaments, distal clavicle, AC joint, and acromial process. The superior strut is the middle clavicle, and the inferior strut is the lateral scapular body and spine (Fig. 11-2).

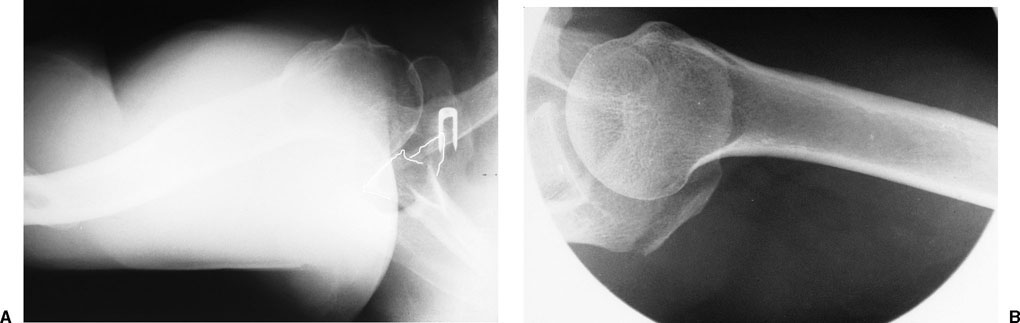
FIGURE 11-1 Anteroposterior (AP) chest radiograph of a scapulothoracic dissociation. The arrow demonstrates the widened medial border of the laterally displaced scapula. Note the associated clavicle fracture. The lateral fragment of the clavicle cannot be visualized because of the significant lateral displacement.
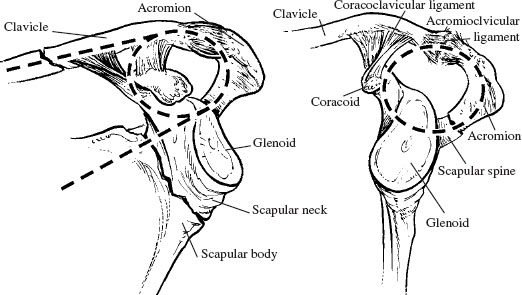
FIGURE 11-2 The diagrams demonstrate the oblique and lateral views of the two struts and the one ring of the superior suspensory shoulder complex (SSSC). The two struts consist of the clavicle and scapular neck. The ring consists of the distal clavicle, acromioclavicular ligaments, acromial process, glenoid fossa, coracoid, and coracoclavicular ligaments.
A disruption of one part of the ring (i.e., scapular neck fracture, glenoid fracture, or clavicle fracture) still maintains the structural integrity of the shoulder girdle complex with the axial skeleton (Fig. 11-3A); however, a double disruption of the SSSC (i.e., associated scapular neck fracture and clavicle fracture) produces an inherently unstable relationship between the shoulder girdle complex and the axial skeleton and has been termed “the floating shoulder” (Fig. 11-3B,C).12 Double disruptions may take a variety of forms from purely osseous or ligamentous disruptions to a combination of both. Double disruptions may also range from pure ring or strut injuries to a combination of both. Williams et al13 have disputed the concept of shoulder instability following a double disruption of the SSSC in biomechanical testing of sequentially sectioned cadaveric shoulders. They found that pure strut injuries (ipsilateral clavicle and scapular neck fractures) did not produce an unstable shoulder without an additional ligamentous disruption of the ring (coracoacromial or AC ligaments).
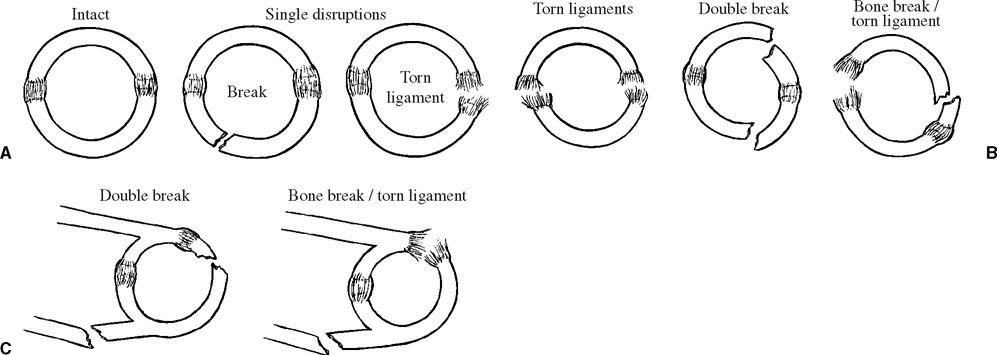
FIGURE 11-3 The diagrams demonstrate an intact ring, a single disruption, and double disruption of the SSSC. (A) A single disruption maintains stability of the shoulder girdle. (B,C) A double disruption of the SSSC represents an inherently unstable shoulder girdle.
Several important neurovascular structures lie in close proximity to the scapula (see Fig. 2-11 in Chapter 2). Due to the mobility of the scapula and the lack of fixed attachments of the scapula to the axial skeleton, neurovascular structures are at risk for injury. The brachial plexus and axillary artery are in close contact with the undersurface of the coracoid and lie deep to the pectoralis minor tendon. In high-energy mechanisms of injury, these structures may be tethered as they course from the thoracic outlet, past the anterior aspect of the shoulder girdle, and into the upper extremity. The suprascapular neurovascular structures pass through the incisura scapula, or scapular notch. The notch is bridged by the transverse scapular ligament, and the suprascapular artery and nerve pass over and under this ligament, respectively. The suprascapular nerve is especially vulnerable both to direct injury due to an extension of a scapular neck fracture into the scapular notch and to indirect injury due to traction caused by fracture displacement. Similarly, the axillary nerve may sustain direct or indirect injury due to a displaced scapular neck fracture. Finally, the dorsal scapular and accessory nerves found in association with the branches of the transverse cervical artery along the medial border of the scapula are vulnerable to injury in displaced fractures of scapular body.
 Clinical Evaluation
Clinical Evaluation
The most important aspect of the initial clinical evaluation of the patient with a scapular fracture is the prompt recognition and management of any associated injuries. Given the high association of concomitant injuries (80 to 95%) to the thorax, neurovascular structures, and shoulder girdle, an isolated fracture of the scapula is diagnosis of exclusion. Full Advanced Trauma Life Support (ATLS) evaluation is routinely performed. The mechanism of injury, level of consciousness, and Glasgow Coma Scale score are all documented.

FIGURE 11-4 Clinical photograph of a 38-year-old man who sustained a displaced left scapular body fracture, demonstrating the soft tissue injury associated with this high-energy mechanism.
FIGURE 11-5 Chest radiograph of a displaced left scapular body fracture with an ipsilateral pulmonary contusion.
The clinical assessment begins with a systematic and careful examination for associated injuries, which may be potentially life threatening or limb threatening. Detailed examination of the mediastinum and thorax is performed to evaluate pulmonary contusions, tension pneumothorax, and rib fractures.
A focused examination of the shoulder is then performed. Physical findings can be subtle with minimal deformity, as in a nondisplaced fracture of the acromion process, to obvious with gross deformity, as in a potentially life-and limb-threatening scapulothoracic dissociation. Careful assessment and documentation of soft tissue injury including abrasions, open wounds, closed degloving injuries, and muscular trauma is critical. Skin surface abrasions lead to bacterial contamination and may delay or preclude surgical intervention (Fig. 11-4). Deeper soft tissue injury can also lead to wound healing problems after surgery. Patients typically present with the upper extremity in an adducted, immobile position, and supported by the contralateral hand. There is usually diffuse tenderness and swelling about the shoulder girdle with limited, painful range of motion. Crepitus in the scapula is difficult to elicit, given the significant soft tissue coverage; however, crepitus and a palpable step-off in the clavicle may be obvious based on its subcutaneous location and should be specifically evaluated.
A comprehensive neurologic examination is performed to identify any brachial plexus pathology. Not only is the function of the musculocutaneous, radial, median, and ulnar nerves tested, but also particular attention is paid to the axillary and suprascapular nerves due to their close anatomic relationship with the scapula. It is often difficult to evaluate the function of these nerves in the acutely injured patient; however, serial exams should be performed after the initial evaluation to identify a potential deficit. A careful examination is conducted also to detect any vascular injury and to assess limb viability. Although easily performed in the awake patient, this evaluation is more difficult in the patient with a significant head injury.
Radiographic Evaluation
The trauma series consisting of an anteroposterior (AP) chest radiograph, lateral cervical spine radiograph, and AP pelvis radiograph is standard in the evaluation of the polytrauma patient with a scapular fracture. Often, the scapular fracture is first identified on the AP chest radiograph (Fig. 11-5). The chest radiograph should be considered an essential part of the evaluation because of the high incidence of associated injuries to the thorax and its contents. Scapulothoracic dissociation can also be diagnosed on the chest radiograph when the nonrotated film demonstrates significant lateral displacement of the scapula as measured by the distance from the sternal notch to the medial border of the scapula or to the glenoid margin.14
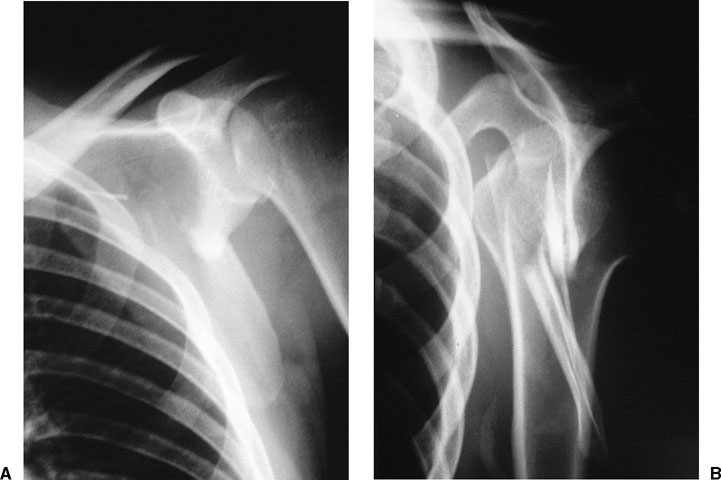
FIGURE 11-6 Anteroposterior (A) and scapular lateral (B) of a displaced scapular body fracture.
FIGURE 11-7 Axillary radiographs of a displaced glenoid (A) demonstrating anterior subluxation of the humeral head and (B) a fracture of the posterior portion of the acromion.
The radiographic evaluation specific to scapula fractures includes the standard shoulder trauma series of the shoulder, consisting of not only AP and lateral views of the affected shoulder in the plane of the scapula (Fig. 11-6), but also an axillary view. The axillary view can be particularly helpful in identifying acromial fractures or in determining glenohumeral subluxation associated with an intraarticular glenoid fracture (Fig. 11-7). Further radiographic images that may be helpful in certain situations include oblique views to better delineate fracture lines of the scapula, a 45° caudal tilt view to better identify fractures of the clavicle, and a 45° cephalic tilt view to better identify fractures of the coracoid (Fig. 11-8).

FIGURE 11-8 Additional radiographic view with a 45° cephalic tilt to identify a fracture of the base of the coracoid.
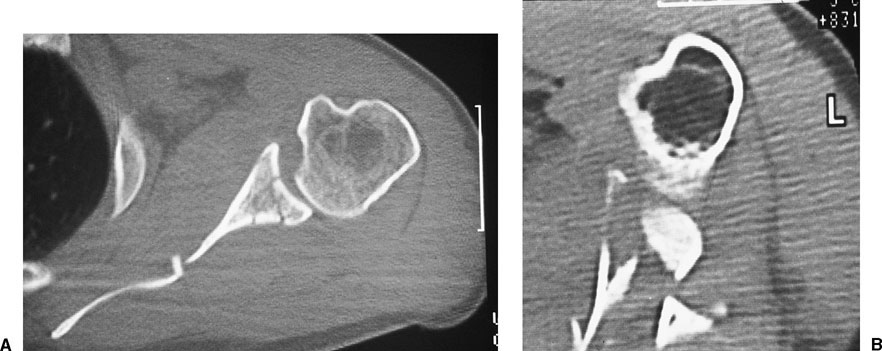
A computed tomography (CT) scan with two-dimensional reconstruction in the sagittal and coronal planes can provide additional anatomic detail and can better delineate the personality of the scapula fracture. It is especially important in intraarticular glenoid fractures to assess the amount of intraarticular involvement as well as the degree of displacement of the humeral head (Fig. 11-9). It is also especially helpful in preoperative planning when considering operative management. CT scan with three-dimensional reconstruction provides excellent reproductions of fracture patterns and may provide important information in complex cases (Fig. 11-10); however, their direct benefits in determining a treatment plan have yet to be determined.
 Classification
Classification
Scapular fractures are commonly described according to the anatomic location (Fig. 11-11). Scapular body fractures are most commonly encountered, accounting for 50 to 60% of scapular fractures in most series. Scapular neck fractures occur in about 25% of cases, followed by glenoid, acromion, spine, and coracoid fractures, in decreasing order of frequency.2–8,15 In many cases, fractures represent some combination of these different types. The most common combinations include body fractures with extraarticular extension into the neck, and intraarticular glenoid fractures with extraarticular extension into the neck and body. Ada and Miller2 introduced an anatomic classification based upon their review of fracture patterns in 116 scapular fractures. Scapular fractures were divided into four types and classified according to the anatomic location of the fracture (Table 11-2).
FIGURE 11-9 Computed tomography (CT) scan of a scapular body fracture with a nondisplaced intraarticular component (A) and a scapular body fracture with a comminuted and displaced glenoid component (B).
Other classification systems have focused on specific fracture locations. Eyres et al16 classified coracoid fractures according to the degree of extension of the fracture into the base of the coracoid. Types I, II, and III do not involve the body of the scapula and can be treated non-operatively. Type IV fractures involve the body of the scapula, and type V involve the glenoid fossa. Operative management is indicated for types IV and V fractures. Kuhn et al17 introduced a classification system of acromial fractures. Acromial fractures were divided into three types: nondisplaced (type I), displaced (type II), and displaced with subacromial impingement (type III). Surgical treatment was recommended only for type III fractures.
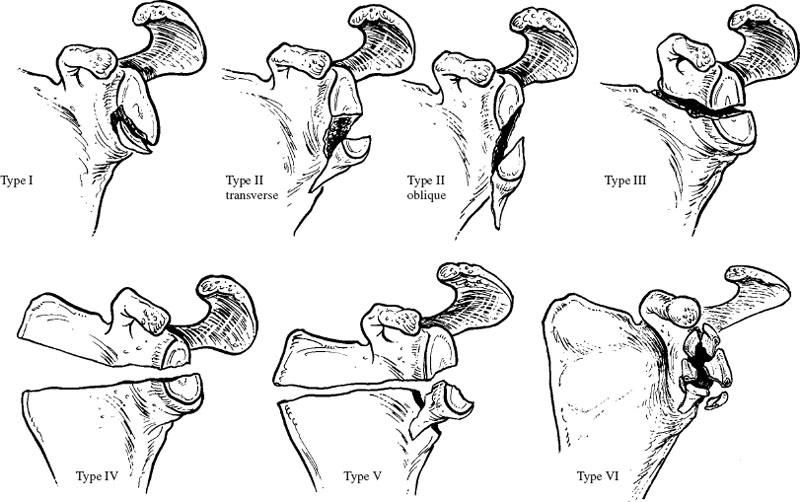
Ideberg18 introduced a classification system specifically for intraarticular fractures of the glenoid and based on fracture pattern (Fig. 11-12). Five types have been described and are classified according to the location of the exiting fracture line (Table 11-3). In type I fractures, there is an avulsion fracture of the anterior rim of the glenoid. In type IIA fractures there is a transverse fracture through the glenoid fossa exiting inferiorly, and in type IIB there is an oblique fracture through the glenoid fossa exiting inferiorly. In type III there is an oblique fracture through the glenoid that exits superiorly and is often associated with an AC joint injury. In type IV fractures there is a transverse fracture exiting the medial border of the scapula. Type V fractures represent a combination of type II and type IV injury patterns. Goss19 added a modification to the Ideberg classification and included a type VI glenoid fracture to differentiate severely comminuted glenoid fractures.

FIGURE 11-10 Three-dimensional CT reconstruction of a displaced scapular neck and body fracture.
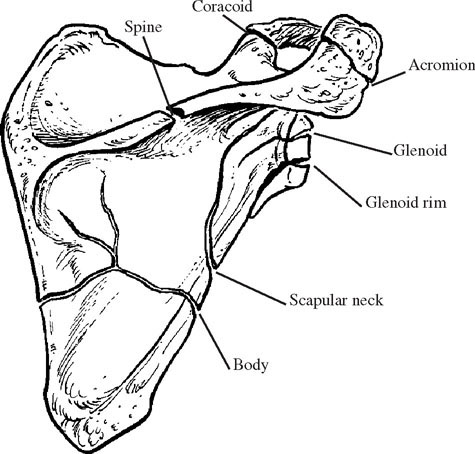
FIGURE 11-11 The anatomic classification of scapular fractures.
| Type I | Acromion, scapular spine, coracoid process fractures |
| Type II | Scapular neck fractures |
| Type III | Glenoid fractures |
| Type IV | Scapular body fractures |
The Orthopaedic Trauma Association (OTA) has introduced the most comprehensive classification of scapular fractures (Table 11-4).20 Fractures are classified into either extraarticular (Fig. 11-13A) or intraarticular involvement (Fig. 11-13B). Extraarticular (type A) fractures are further subclassified into fractures of the scapular processes (A1), body (A2), and complex (A3). Intraarticular (type B) fractures are subclassified into impacted glenoid (B1), nonimpacted glenoid (B2), and complex glenoid (B3) fractures. The clinical utility of this slightly cumbersome classification scheme is based on the fact that nearly all scapular fractures can be classified. Double disruptions of the SSSC, or “floating shoulder” injuries, can be classified under extraarticular complex (A3) injuries. Intraarticular glenoid fractures with extraarticular extension into the neck or body can be classified under intraarticular complex (B3) injuries.
| Glenoid Fractures | Exiting Fracture Line(s) | Description |
|---|---|---|
| Type 1 | Anterior to glenoid fossa | Avulsion fracture of glenoid rim |
| Type 2 | Inferior to glenoid fossa | Type 2A: Transverse Type 2B: Oblique |
| Type 3 | Superior to glenoid fossa | Usually oblique fracture Often associated with acromioclavicular (AC) joint injury |
| Type 4 | Medial border of scapula | Transverse fracture |
| Type 5 | Inferior to glenoid fossa and medial border of scapula | Combination of types 2 and 4 |
| Type 6 | Severe comminution Modification of original classification |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree