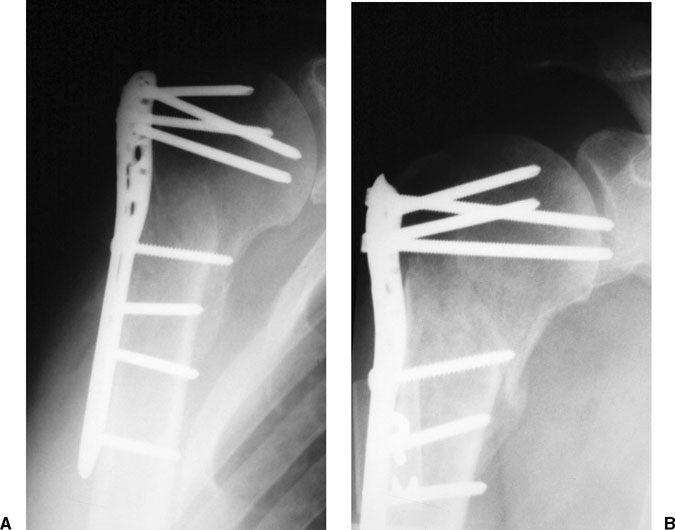
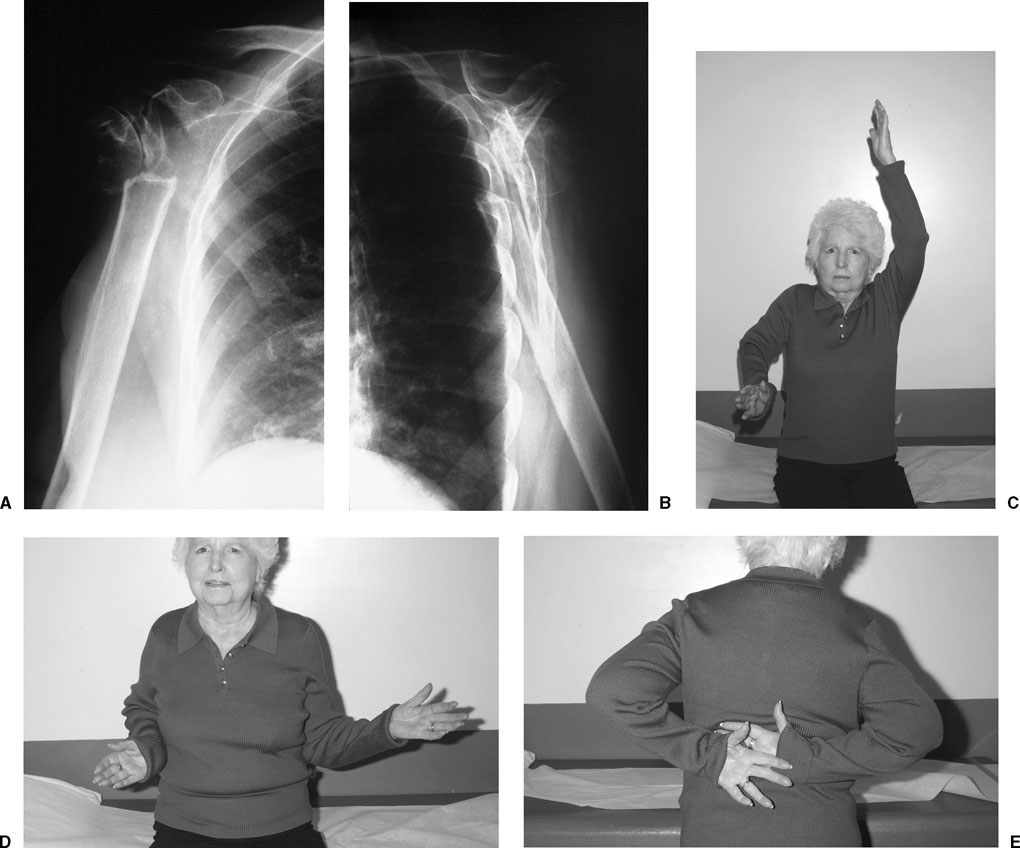
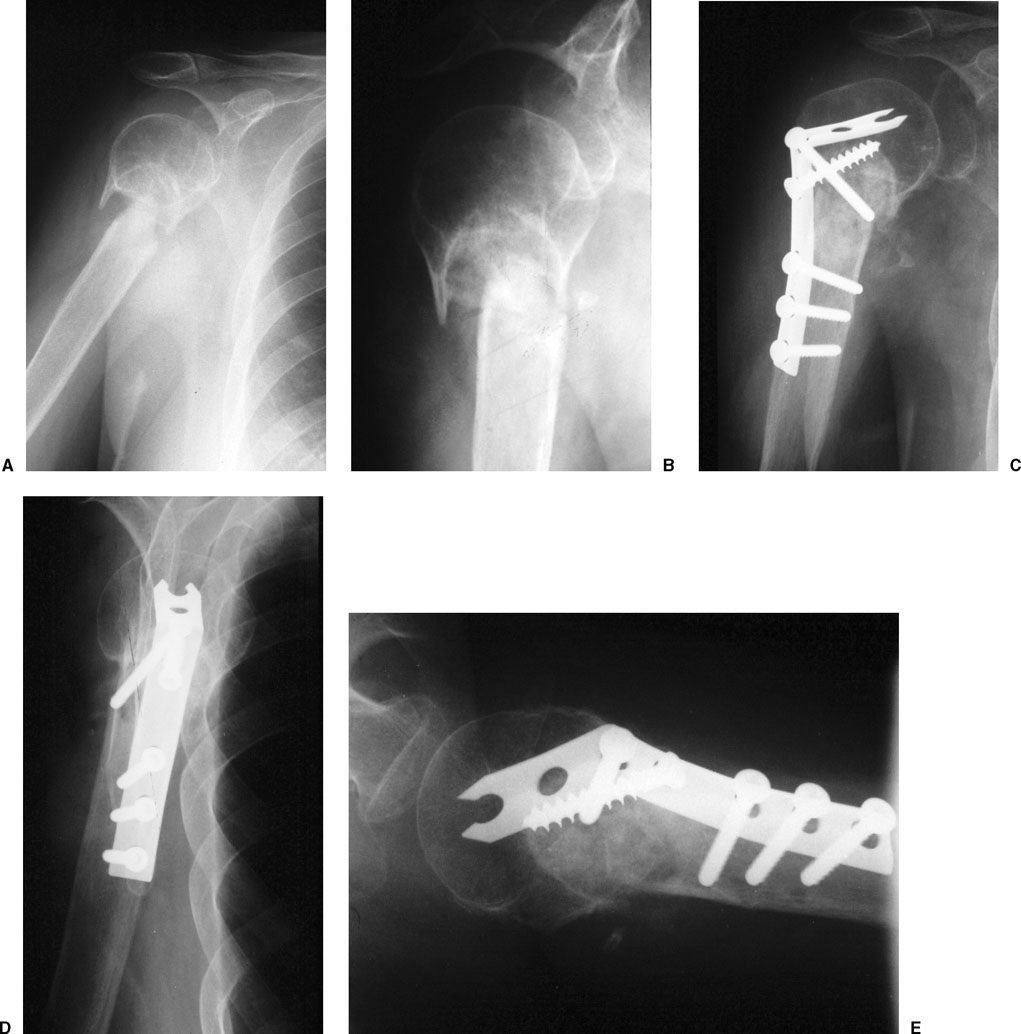
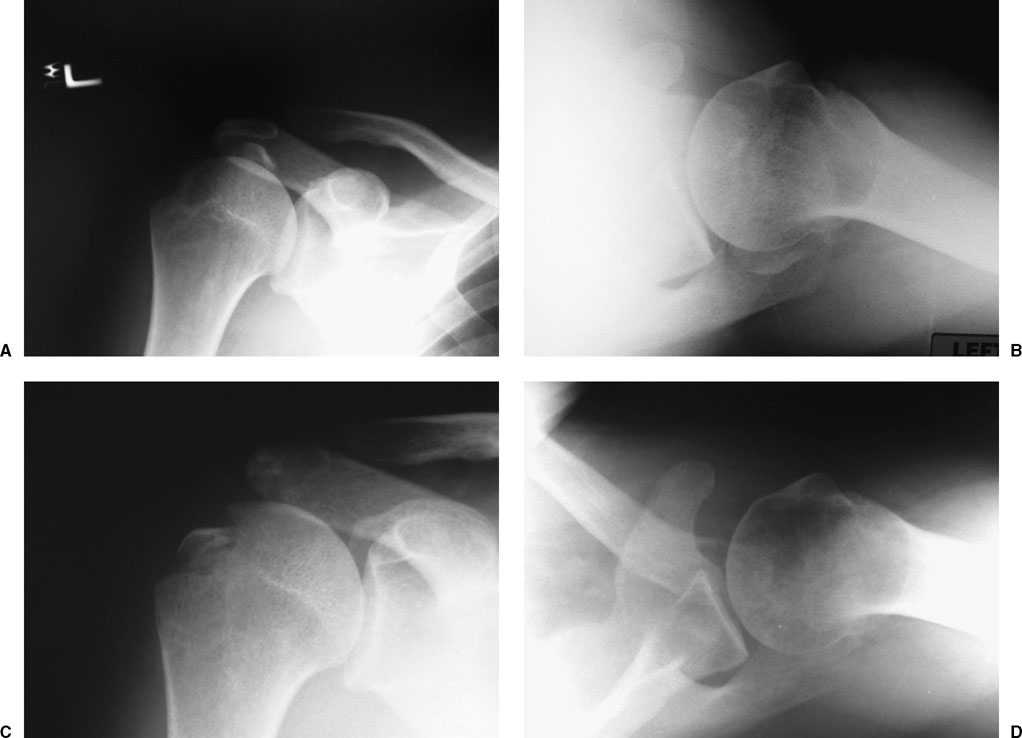
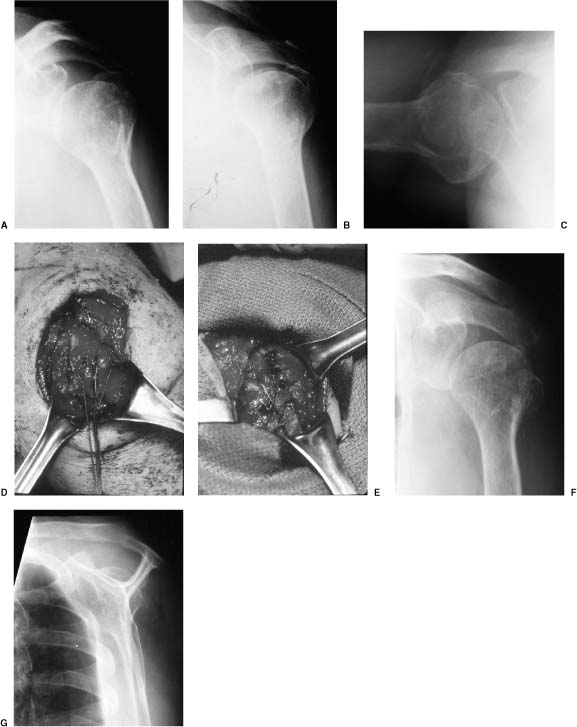
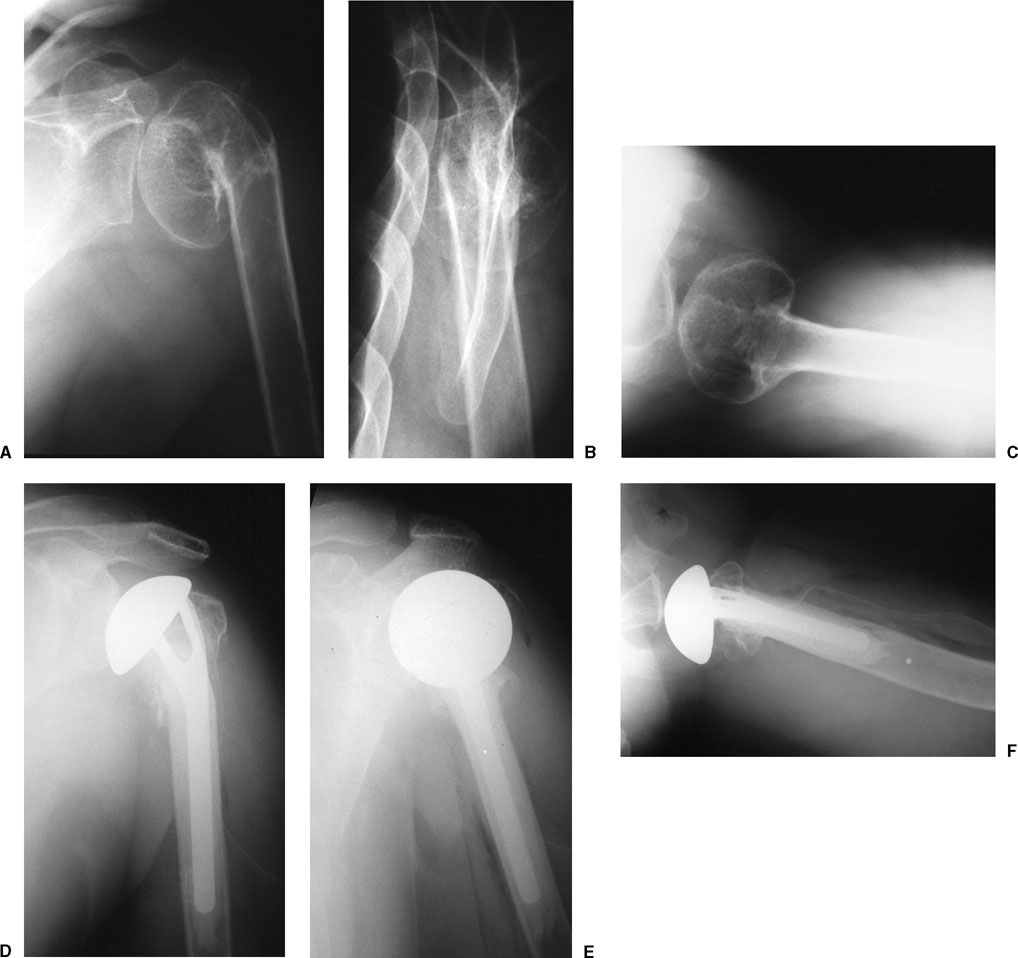
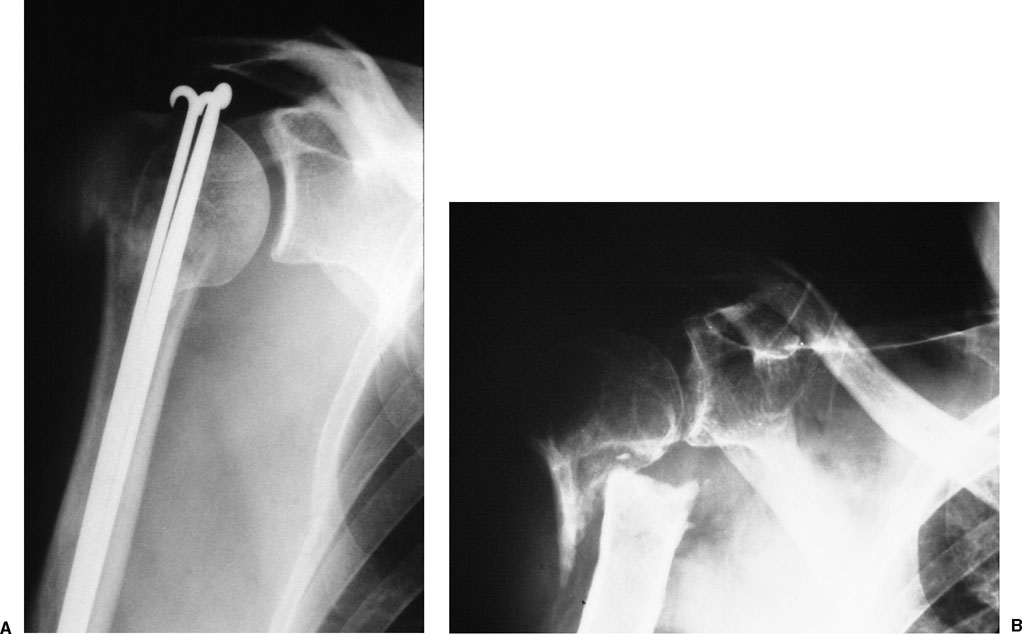
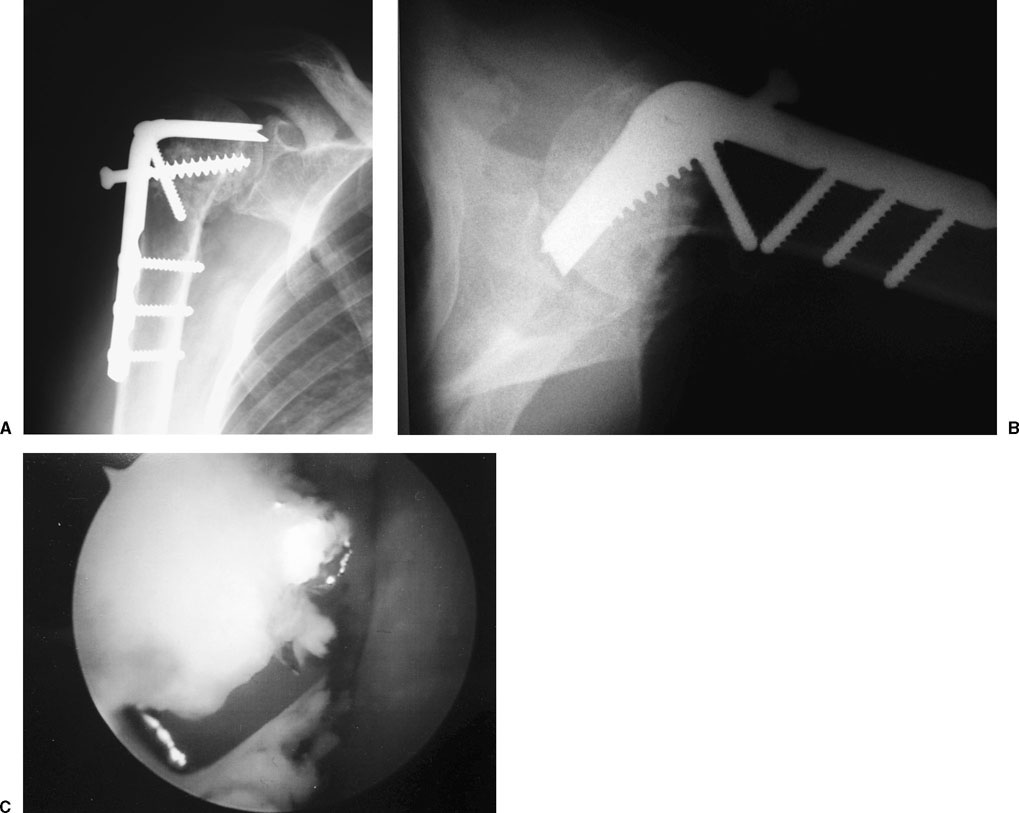
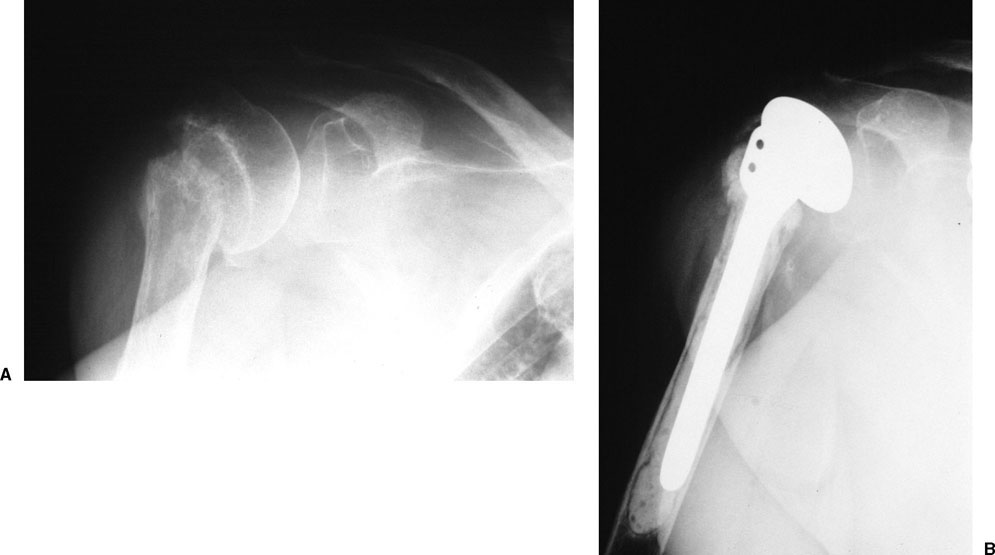
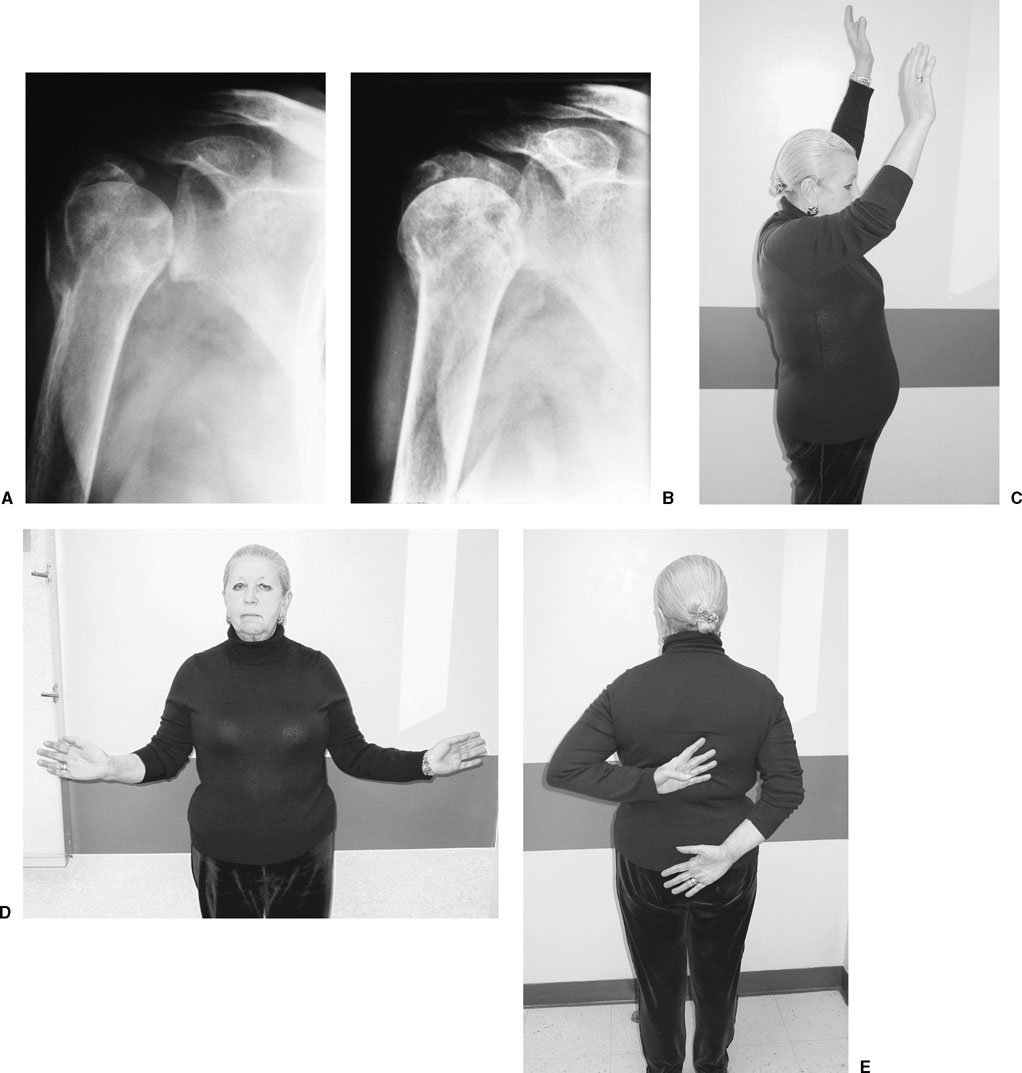
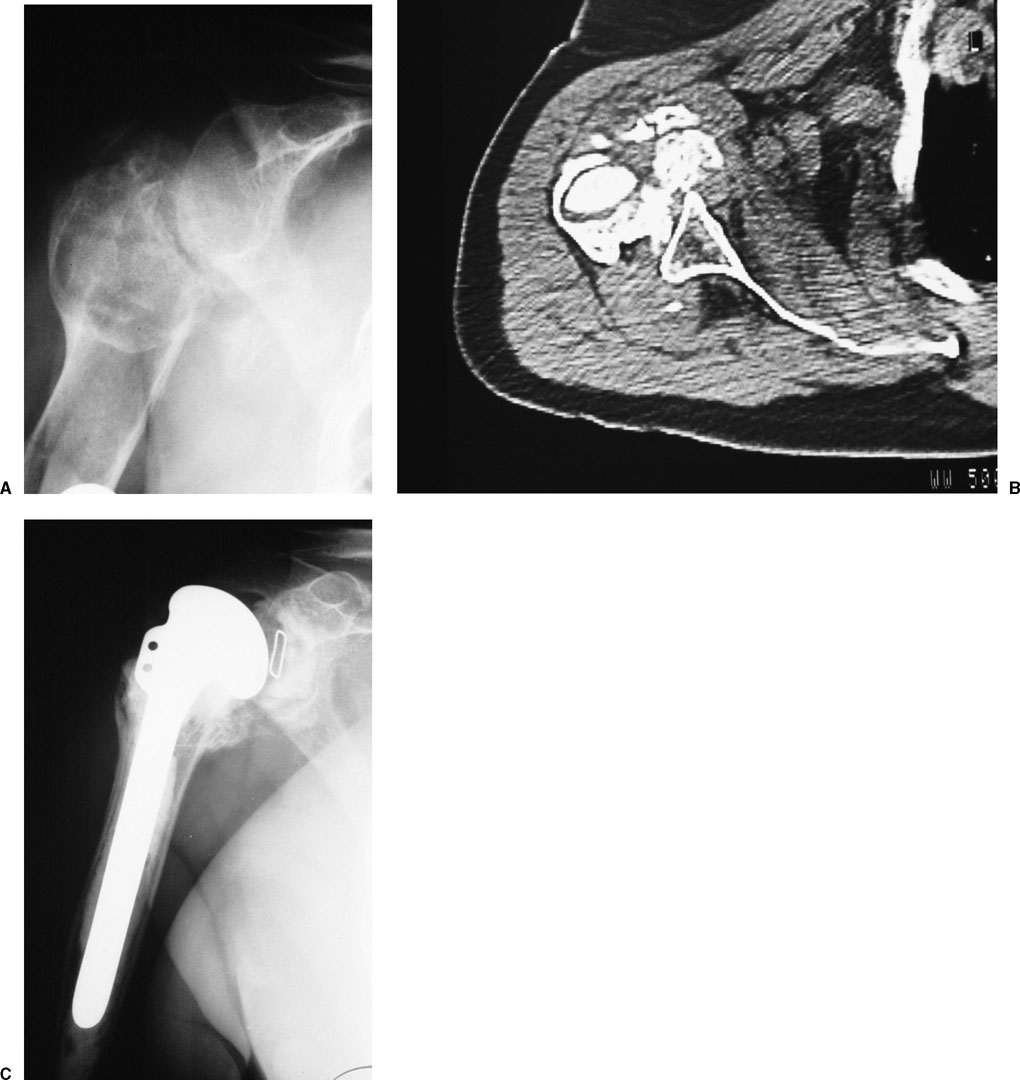
Complications associated with proximal humerus fractures can occur at the time of injury or during treatment. The operative or nonoperative management of these complications is determined by the symptoms attributed to the complication itself. Thorough evaluation of the patient with a complication following a proximal humerus fracture must include an assessment of the patient’s activity level, the degree of dysfunction associated with the complication and its effect on the patient, the patient’s expectations of treatment, and the patient’s ability to participate in the treatment plan. Early complications of operative management include loss of fixation and problems related to internal fixation devices. Bony and soft tissue abnormalities about the shoulder should be evaluated and their contribution to the symptoms and dysfunction assessed. Bony abnormalities include nonunion, malunion, incongruity of the articular surface, osteonecrosis, and heterotopic bone formation. Soft tissue abnormalities include contracture, infection, rotator cuff injury, and neurovascular compromise. Fractures that undergo open or closed reduction and internal fixation can develop problems associated with the fixation devices utilized. The problems can vary from a change in position of an implant (i.e., backing out of a percutaneously placed pin or screw) to complete loss of fixation with redisplacement of the fracture to migration of an implant into the soft tissues adjacent or distant to the shoulder. When complications of this type arise, it is essential to carefully evaluate the significance of the problem and the contributing factors to determine the appropriate treatment. Failure of fixation can occur as a result of different factors including (1) improper insertion, (2) inability to obtain secure fixation, (3) too early or too aggressive postoperative mobilization program, and (4) patient noncompliance with postoperative instructions. Follow-up radiographs should be obtained early in the postoperative period, particularly after initiation of a mobilization program. The nature and degree of loss of fixation or loss of reduction usually determines the treatment required. Minor changes—backout of a pin or screw or a slight change of fracture alignment—may benefit from modification of the postoperative program. A period of immobilization may allow fracture healing to progress sufficiently to prevent further displacement. Although this may compromise recovery of range of motion, it is preferable to a more significant loss of fixation that may result in malunion or nonunion requiring revision surgery. Stiffness in the presence of a healed fracture with acceptable alignment is preferable to an early revision procedure. When there is significant loss of fixation with displacement of the fracture, early revision is usually required (Fig. 9-1). Although each clinical situation should be evaluated individually, there are a few general principles to follow: first, the reason for the early loss of fixation should be evaluated carefully, so these factors can be controlled and prevented following the revision procedure; second, the procedure to be performed should have the best chance of a successful outcome and should minimize the need for another procedure; and third, for any procedure performed, patient compliance with the postoperative program is essential. If there is a question about whether the patient will be compliant, especially if noncompliance contributed to the initial problem, addition procedures should probably be avoided. FIGURE 9-1 A 73-year-old with a displaced, comminuted surgical neck fracture (A) underwent intramedullary fixation (B,C). Fracture reduction was not obtained and fixation was further compromised by the comminution. (D–F) Revision to proximal humeral replacement was performed 5 weeks after the initial surgery. There are a multitude of specific fixation problems that can develop depending on the type of fixation device utilized, which makes it impossible to address each potential clinical situation to be encountered. In general, however, revision open reduction and internal fixation (ORIF) should be considered in younger patients in whom there is a high likelihood of obtaining secure fixation with a revision procedure. The revision procedure should utilize a different type of fixation method than the original, unsuccessful method. If assessment of the failed fixation makes it unlikely that revision fixation can be obtained, proximal humeral replacement should be considered as the preferred approach (Fig. 9-1). It is also important to note that early revision surgery requires meticulous handling of soft tissues to avoid additional problems, specifically the increased risk for heterotopic ossification, which is discussed later in this chapter. Whenever internal fixation devices are utilized about the proximal humerus, there is the potential for hardware complications. Early implant loosening can occur, resulting in migration of an implant into the soft tissues (Fig. 9-2). This usually occurs locally, but migration to remote areas of the body has been reported. Improper placement of implants can cause problems particularly if there is violation of the articular surface (Fig. 9-3). Settling of the fracture can also result in intraarticular migration of implants early, and in some cases, later in the healing process.1 FIGURE 9-2 This 59-year-old man underwent Rush rod fixation of a surgical neck fracture. (A) The rods backed out, causing encroachment on the subacromial space and necessitating premature hardware removal 6 weeks postoperatively. (B) The fracture was not healed and a nonunion developed. Frequent postoperative radiographs should be obtained to monitor the position of the implants. Percutaneous pins should be removed when fracture healing has progressed sufficiently. Smooth pins should not be used, and care should be taken to avoid excessive advancement and backing out of the pins during insertion. When this occurs, a “track” remains, which facilitates migration. Unrecognized, intraarticular implants can result in rapid destruction of articular cartilage (Fig. 9-4). It is essential to obtain a full set of radiographs to properly evaluate the location of the implants (Fig. 9-3). These should be obtained in the operating room prior to completion of the procedure. At the time of follow-up evaluation, if there is any concern about intraarticular location of the implants, proper radiographic evaluation should be performed. In addition to appropriate orthogonal views, it may be necessary to obtain fluoroscopically positioned radiographs to confirm proper position of the implants. Incomplete radiographs will fail to identify problematic hardware, leading to unnecessary problems. FIGURE 9-3 (A) A 57-year-old man underwent locking plate fixation of a surgical neck fracture. He was unable to regain active range of motion and had persistent pain. (B) Follow-up radiographs showed that two of the screws were intraarticular in location, a finding that was not evident on earlier radiographs. FIGURE 9-4 This 66-year-old woman underwent blade plate fixation of a surgical neck fracture. Initial x-rays confirmed proper position of the implant. The patient developed pain and crepitus 4 weeks following the surgery. (A,B) X-rays showed the tip of the blade plate was in an intraarticular location. (C) Arthroscopic images show the protruding portion of the plate. The patient improved following plate removal. FIGURE 9-5 An 81-year-old woman 16 months following right surgical neck fracture that was treated nonoperatively. (A,B) Radiographs show an atrophic nonunion. The patient had minimal discomfort. (C–E) In spite of a significant loss of active motion, the patient did not feel that the symptoms and disability were sufficient to consider operative management. Nonunion most commonly occurs following surgical neck fractures, less frequently with greater tuberosity fractures, and uncommonly following three- or four-part proximal humeral fractures. Surgical neck nonunion can occur as a result of different factors. One of the most common is distraction or motion at the fracture site. Distraction can occur due to soft tissue interposition or, much less commonly, with the use of a hanging arm cast.2 Motion at the surgical neck fracture site is often due to (1) inadequate immobilization, (2) too early mobilization, and (3) inadequate fixation.3,4 Treatment of a surgical neck nonunion is determined by the symptoms associated with the nonunion. Nonoperative management may be most appropriate if the patient has minimal symptoms or disability (Fig. 9-5). If the symptoms and disability are significant, operative management should be considered, and will typically consist of ORIF (using a variety of devices) or proximal humeral replacement.5–8 Preoperative assessment must include the patient’s age and activity level, the quality of the bone of the proximal humerus, and the size of the nonunited head fragment. Methods of operative management typically include tension band fixation with modified Enders rods, blade plate fixation, or other plate and screw devices (Fig. 9-6).5,6,8 Regardless of which method is utilized, bone grafting is a necessity. FIGURE 9-6 (A,B) A 58-year-old woman with surgical neck nonunion following nonoperative management. (C–E) Open reduction and internal fixation (ORIF) with a modified blade plate and bone grafting was performed. The techniques of proximal humeral replacement varies based on the level of the nonunion and the size of the proximal fragment.7 When the proximal fragment is small, the tuberosities should be osteotomized and reattached to the prosthesis (Fig. 9-7). Mobilization of the tuberosities is essential to obtain a tension-free reattachment. When the proximal fragment is larger, it may be possible to resect the articular surface and pass the prosthesis through the proximal segment (“skewering technique”) and into the shaft. When this technique is used, it is essential to compress the fragments, avoid cement interposition at the nonunion site, and add bone graft to aid in achieving union (Fig. 9-8). If the “skewering” technique is utilized, mobilization of the proximal fragment is equally important to minimize the stresses on the nonunion site. Specific mobilization techniques should be performed in a step-by-step sequence. Both treatment approaches—ORIF and prosthetic replacement—can be technically demanding. Successful results have been achieved using both techniques.5–8 FIGURE 9-7 A 66-year-old with surgical neck nonunion. (A) The proximal fragment is small and osteopenic. (B) Proximal humerus replacement combined with tuberosity osteotomy and reconstruction was performed. Greater tuberosity nonunions can occur due to medial displacement of the fragment onto the articular surface where it is bathed in synovial fluid (Fig. 9-9). The synovial fluid lyses the fracture hematoma and interferes with the healing process. Inadequate initial radiographic evaluation can lead to a missed diagnosis, especially if the fragment is displaced posteriorly and not visualized on the anteroposterior (AP) radiographs. Patients with a greater tuberosity nonunion often present with pain and limitation of motion. Because the nonunited fragment results in a functional rotator cuff tear, weakness is also common. Treatment of the nonunited displaced greater tuberosity is more difficult than an acute repair because of the contracted rotator cuff tissues, formation of adhesions in the subacromial space, and the quality of the bony fragment. Operative management utilizes a superior approach with development of the interval between the anterior and middle portions of the deltoid and elevation of the deltoid from the anterior acromion. A more limited deltoid splitting approach can be considered, but displacement of the fragment and the difficulties of mobilization generally require a more extensive exposure. In situations when a posterior portion of the greater tuberosity is displaced into a posterior and medial position, a posterior deltoid splitting approach may be necessary for adequate visualization and mobilization. Regardless of the approach utilized, the ability to rotate the humerus significantly enhances the exposure even when relatively small incisions are utilized. After exposure of the fragment, the first step is mobilization. This requires lysis of adhesions with subacromial space release of fibrous tissues that developed adjacent to the fragment. It is often necessary to release the coracohumeral ligament at the base of the coracoid for enhanced mobilization. The fibrous tissues that fill the gap between the fragment and the intact greater tuberosity should be resected. This allows visualization of the articular surface. Fibrous tissue should be removed from the area of the intact greater tuberosity to expose the area that corresponds to the site of the fracture. Cancellous bone should be exposed along with the portion of the greater tuberosity located anterior and posterior to the fracture site. It is often helpful to enlarge the bed slightly to allow overreduction of the fragment and minimize the possibility of any residual prominence. Intraarticular mobilization is necessary, and usually consists of release of the capsule at the glenoid margin to enhance lateral advancement of the fragment. It is essential to achieve adequate mobilization of the fragment for an anatomic reduction with minimal tension. If the fragment originated from the anterior portion of the greater tuberosity, when it is reduced the arm should be able to be placed in a sling at the side without excessive tension on the repair. If a more posterior portion of the tuberosity was involved, ideally the arm should also be able to be placed in a sling without excessive tension on the repair. If this is not possible, however, it is often beneficial to use a modified sling or an orthosis that maintains the humerus in varying degrees of external rotation. This reduces the tension on the repair. Fixation of the fragment is usually accomplished with figure-of-eight repair using No. 5 nonabsorbable suture passed through the rotator cuff insertion and through the humeral cortex distal to the bed. If the fragment is small and bone quality is poor, however, it can be excised and the tendon repaired directly to bone with nonabsorbable sutures passed through bone tunnels. This is the equivalent of a tendon to bone rotator cuff repair. When the repair is completed, range of motion should be assessed to determine the parameters of the postoperative therapy program. There should be minimal tension on the fragment with the arm at the side. If this cannot be achieved, it will be necessary to modify the position of immobilization. FIGURE 9-8 (A) An 81-year-old underwent ORIF of proximal humeral shaft fracture with inadequate cerclage fixation, resulting in nonunion. (B,C) Proximal humeral replacement was performed with the prosthesis used to “skewer” the proximal fragment to obtain “intramedullary” fixation combined with fibular strut grafting and cancellous autograft. (D) Two weeks following surgery the patient fell, sustaining a distal periprosthetic fracture requiring ORIF with a plate and fibular strut graft. (E,F) Three months later both the nonunion and the fracture have healed. FIGURE 9-9 (A,B) A 43-year-old man with a greater tuberosity nonunion 6 months after an unrecognized injury. (C,D) Open reduction with soft tissue releases was performed, allowing the fragment to be reduced into its bed. Postoperatively, a passive range-of-motion program is initiated based on the parameters identified intraoperatively. Radiographs are obtained 1 week following the surgery to confirm that the fragment remains in position. A passive range-of-motion program is utilized for 6 weeks, after which time radiographs are obtained. If there is any concern about healing, a longer period of immobilization is utilized; however, at 6 weeks an active range-of-motion program can usually be instituted. At 10 to 12 weeks, stretching and strengthening exercises can be added. Malunion following proximal humeral fractures can involve the articular surface, the tuberosities, the shaft, or a combination of these segments. This bony deformity is typically associated with soft tissue abnormalities, and both factors contribute to the loss of motion. Evaluation with a complete set of standard radiographs can be supplemented with a computed tomography (CT) scan to determine the relationship of the malunited fragments to the articular surface and the shaft.9 The operative treatment of malunion is reserved for patients with persistent symptoms after nonoperative treatment fails to relieve pain or improve function and when there is strong evidence that the malunion is the primary source of the symptoms. Some patients are able to regain very good range of motion and overall function in spite of radiographs that show significant malunion (Fig. 9-10). For these patients, nonoperative management is the treatment of choice. The large spectrum of symptoms associated with proximal humeral malunions mandate that each case be considered individually. FIGURE 9-10 (A,B) A 72-year-old woman with proximal humeral malunion 6 months following fracture. (C–E) In spite of the radiographic appearance, range of motion and overall function allowed her to perform all the activities of daily living. Operative management for symptomatic malunion must address both osseous and soft tissue abnormalities. These have been classified by Beredjiklian et al.10 Type I osseous deformity is a greater tuberosity malunion of at least 1 cm; type II involves an intraarticular incongruity with a step-off greater than 5 mm; and type III is malalignment of the articular segment. Soft tissue abnormalities include type I, soft tissue contracture; type II, rotator cuff tear; and type III, subacromial impingement. The same authors document that operative management for malunion is challenging. In their series they reported 69% satisfactory results with a 28% complication rate.10 The patient with a malunited greater tuberosity may complain of pain, loss of motion, and weakness. A displaced tuberosity can result in a mechanical block of motion. If the fragment is displaced superiorly and medially, subacromial impingement will result in pain and a loss of abduction and forward elevation (Fig. 9-11). Displacement posteriorly will limit external rotation. A malunited tuberosity can also be the functional equivalent of a rotator cuff tear. Shortening of the rotator cuff interferes with the length tension relationship of the musculotendinous construct, thereby reducing function. Treatment of a malunited greater tuberosity should be based on an assessment of the associated symptoms. If stiffness is the primary problem, it is important to confirm whether the patient was compliant with a structured, supervised rehabilitation program. Although it is somewhat unlikely that stiffness associated with significant deformity superiorly or posteriorly will respond to an exercise regimen, lesser degrees of malunion may respond very well to a therapy program. However, patients with an obvious mechanical block to motion experiencing pain and stiffness will not respond to nonoperative management. When the symptoms of pain and stiffness and the associated dysfunction are significant, operative management is indicated. Operative management primarily consists of osteotomy of the malunited fragment, mobilization, and reduction into an anatomic position to obtain bony union (Fig. 9-11). In some instances, resection of the fragment and rotator cuff repair may be necessary if adequate mobilization cannot be obtained; however, this is a less attractive option than osteotomy, reduction, and fixation. The approach to a greater tuberosity malunion is similar to that described for nonunion. After exposure of the subacromial space through a superior approach, we perform an acromioplasty to increase the space within the subacromial region both for exposure as well as to avoid any subacromial encroachment postoperatively. Identification of the malunited fragment may be difficult, and intraoperative radiographs can be beneficial. The fragment can usually be identified by exposing the intact greater tuberosity anteriorly and posteriorly. The area corresponding to the origin of the fragment should be exposed. The bed is usually covered with fibrous tissue and/or bone depending on the amount of time since the injury, and it may not be easily identified. When the anterior and posterior margins of the fragment are identified, the rotator cuff can be incised longitudinally in these areas. This allows visualization of the articular surface. The junction between the fragment and the articular surface can either be visualized or at least palpated with a small elevator. Identification of this junction and the lateral extent of the fragment determine the direction and angle of the osteotomy to be performed. The osteotomy should be performed with a sharp osteotome. Care should be taken to avoid any compromise of the articular surface. In addition, it is essential that the osteotomy include an adequate fragment of bone, even if it has to be reduced in size at the time of reduction. Once the fragment is osteotomized, the attached tendon should be tagged with sutures to begin the mobilization process. Extramuscular and intraarticular releases are performed to allow the fragment to be advanced laterally to a cancellous bed that should correspond to its origin. It may be necessary to reduce the size of the fragment so it can be reduced. Slight overreduction is preferred to prevent any residual prominence. We prefer fixation with figure-of-eight tension band suture using a No. 5 nonabsorbable suture. These sutures are passed through the lateral humeral cortex distal to the bed. The drill holes for these sutures should be placed distal enough to prevent the possibility of propagation of the drill hole into the cancellous bed. When the fixation of the fragment is completed, the anterior and posterior incisions in the rotator cuff should be repaired. The shoulder should be placed through a range of motion and the stability of the fixation assessed. This will determine the parameters for the postoperative rehabilitation program. The fragment ideally should be securely fixed in position so that the arm can be placed in a standard sling. For posterior fragments, however, it may be necessary to maintain some degree of external rotation to decrease tension on the repair. Modifications of the postoperative immobilization should be determined based on these intraoperative assessments. Postoperatively, radiographs are obtained 1 to 2 weeks following the surgery to confirm that the fragment remains reduced. A passive range-of-motion program is utilized for the first 6 weeks. At that time, if radiographs confirm adequate healing, rehabilitation is progressed to an active range-of-motion program. If there is any question about healing, a longer period of immobilization should be utilized with continuation of passive range-of-motion exercises. A more vigorous stretching and strengthening program is not initiated until at least 12 weeks following the surgery. FIGURE 9-11 (A,B) A 52-year-old with greater tuberosity malunion following nonoperative management, resulting in painful, limited range of motion. The tuberosity is displaced superiorly into the subacromial space. (C) Axillary view does not show significant posterior displacement. (D,E) Treatment consisted of osteotomy, mobilization, and reattachment using tension band suture fixation. (F,G) Postoperative radiographs show the tuberosity in fixed position. A complete radiographic evaluation is required to determine the multiplanar deformity of the surgical neck malunion. The deformity typically consists of varying degrees of apex anterior angulation, internal rotation, and varus. The varus deformity limits abduction and places the greater tuberosity into a prominent superior position. Forward elevation is limited by the amount of apex anterior angulation. A complete understanding of the nature of the malunion is essential to determine an appropriate treatment plan. Operative management of surgical neck malunion should be considered in patients who have significant pain and functional limitations that interfere with their ability to perform daily activities. In surgical neck malunions, the articular surface is usually uninvolved. Therefore, corrective osteotomy, restoration of alignment, and internal fixation are preferred.5,11 The type of fixation chosen should be based on the location of the osteotomy and the bone quality. In general, we prefer to use plate and screw fixation with either a blade plate or a locking plate (Fig. 9-12). The procedure is performed using a deltopectoral approach. The soft tissue layers should be developed particularly at the deeper layers to enhance the “gliding” needed to regain range of motion. Adequate mobilization of the proximal fragment is very important. This is usually accomplished by mobilization of the subacromial space and the subdeltoid space. In some situations, however, release of the coracohumeral ligament area and excision of the coracoacromial ligament may be necessary. If there is concern about intraarticular adhesions, the rotator interval should be opened and intraarticular release is performed. It is important to mobilize the proximal fragment to avoid stresses at the osteotomy site, which could interfere with healing. After mobilization of the proximal humerus, the area of malunion should be exposed. It is important to correlate the intraoperative findings with the preoperative radiographic evaluation. To accomplish this, it is often necessary to obtain intraoperative radiographs to confirm the location and direction of the osteotomy. A single-plane osteotomy may be sufficient but usually a wedge-shaped osteotomy is necessary to obtain the required correction. The rotational component of the malunion can be corrected by rotating the fragments after the osteotomy. Rotational alignment can be determined by evaluation of the biceps tendon as it passes through the bicipital groove into the distal fragment. For fixation of the osteotomy, we prefer a blade plate or a locking plate. A guidewire should be placed in the proximal fragment, and biplanar intraoperative imaging used to confirm proper location. Compression at the osteotomy site is essential. If a wedge osteotomy is performed, the bone removed should be utilized to bone graft the site. A complete set of radiographs should be obtained intraoperatively to confirm reduction of the malunion and proper placement of the fixation device. Intraoperative assessment of fixation stability should be used to determine the parameters for the postoperative rehabilitation program. Postoperatively, the patient is maintained in a sling and started on an assisted range-of-motion program, including forward elevation and internal and external rotation. Active range of motion can be initiated approximately 6 to 8 weeks following the surgery when there is evidence of healing of the osteotomy. More vigorous stretching can be performed 10 to 12 weeks following the surgery when healing has progressed. More complex malunions occur following three-and four-part fractures. In these situations, articular incongruity, degenerative changes, and osteonecrosis can be present, making proximal humeral replacement with osteotomy and reconstruction of the tuberosities the recommended management (Fig. 9-13); however, outcomes following proximal humeral replacement in this context have been less satisfactory than when the procedure is performed for acute fractures.12 This is particularly true if the patient has had previous ORIF and when tuberosity osteotomy is required.13,14 Osteotomy and internal fixation of three- or four-part malunions has limited indications. It is generally considered in young patients with good bone quality in whom adequate fixation and healing can be obtained and in whom prosthetic replacement is less desirable. Proximal humeral replacement for three-and four-part malunions utilizes the techniques described previously. An anterior deltopectoral approach is used with mobilization of the subacromial and subdeltoid spaces. The proximal humeral anatomy must be carefully identified. The biceps tendon should be identified and tagged. This facilitates identification of the tuberosities. The lesser tuberosity with the subscapularis attached should be identified. It should be osteotomized with an adequate amount of bone to facilitate reattachment. This allows visualization of the articular surface and the greater tuberosity. Osteotomy of the greater tuberosity should include the entire tuberosity, which includes its superior and posterior portions. Based on the anatomy of the malunion, this may result in two fragments: a superior portion and a more posterior portion. Each one must be tagged at the rotator cuff tendon insertion. The articular surface identified can then be visualized. It should be osteotomized at a level that preserves as much shaft as possible. Extramuscular and intraarticular mobilization of the tuberosities is performed to allow tension-free reattachment. At this point, the reconstruction consists of the technique described in Chapter 7 for a four-part fracture. It is important to emphasize the need for adequate mobilization of tuberosities with secure fixation to the prosthesis, the shaft, and to each other. The removed articular surface should be used to bone graft the tuberosity reattachment site to enhance healing. In some long-standing malunions, there may be significant degenerative changes of the glenoid, although in our experience this has been uncommon. When present, placement of a glenoid component is indicated. FIGURE 9-12 (A,B) A 43-year-old man with surgical neck varus malunion following nonoperative management. Forward elevation was limited to 80°. (C–E) Following corrective osteotomy and blade plate fixation combined with soft tissue releases, forward elevation increased to 160°. FIGURE 9-13 (A-C) A 57-year-old man with proximal humerus malunion 1 year after injury. (D–F) Proximal humeral replacement was performed with osteotomy and reattachment of the tuberosities. Osteonecrosis occurs more commonly after three-and four-part fractures and fracture-dislocations than less complex injuries. The arcuate artery, a terminal branch of the anterior circumflex humeral artery, provides the main blood supply to the humeral head. The rotator cuff insertions and the medial periosteal blood vessels provide secondary blood supply.15,16 Osteonecrosis can develop from disrupting the blood supply at the time of fracture or as a result of additional devascularization secondary to operative management. Four-part fractures that disrupt the soft tissue attachments to the articular surface have the greatest risk for osteonecrosis. Neer3 reported osteonecrosis in six of eight four-part fractures, and therefore, advocated prosthetic replacement. Although this was a very small series, it resulted in significant treatment recommendations. Subsequent reports have documented a 20 to 75% incidence of osteonecrosis depending on the pattern of displacement and the fracture involved.17–21 Valgus-impacted fractures without lateral displacement of the articular surface do not develop osteonecrosis as frequently because the intact medial periosteal hinge often maintains the blood supply to the articular surface.22,23 Less comminuted fractures of the proximal humerus have lower rates of osteonecrosis because the soft tissues with their associated vascular supply remain attached to the articular segment. The incidence in three-part fractures and fracture-dislocations has reported to vary from 3 to 25%.3,24,25 Sturzenegger et al21 found that ORIF of three-part fractures with plates and screws resulted in a higher incidence of osteonecrosis than those treated with limited internal fixation. Lee and Hansen18 also reported that following ORIF, osteonecrosis may not be apparent for up to 2 years following surgery. When osteonecrosis develops following ORIF, collapse of the articular surface can result in prominence of the internal fixation device, which results in secondary damage to the glenoid articular surface.1 Even though the incidence of osteonecrosis following three-and four-part fractures can be significant, it is important to understand that it is not always associated with significant symptoms. Gerber et al26 reported that osteonecrosis of the articular surface with anatomically reduced tuberosities provided results equivalent to humeral head replacement performed for acute fractures. Wijgman et al25 reported that 17 of 22 patients with osteonecrosis following ORIF of three- or four-part fractures maintained good or excellent Constant scores irrespective of the radiographic changes present. Symptomatic osteonecrosis of the humeral head following proximal humeral fracture can be treated in different ways. The most important consideration is the degree of pain and disability. Mild symptoms can be treated nonoperatively with antiinflammatory medication, nonnarcotic analgesics, and a therapy program to maintain or improve range of motion. When the degree of pain and disability is significant, however, operative management is indicated and will usually consist of humeral head replacement or total shoulder replacement based on the degree of involvement of the glenoid. An important component of the preoperative assessment is an understanding of the degree of deformity of the proximal humerus that may be present. This is particularly important with respect to the position of the tuberosities and the surgical neck and shaft. If the tuberosities are in near-anatomic position and there is no significant shaft malalignment, prosthetic replacement can be performed without corrective osteotomies. If there is significant deformity of the proximal humerus, however, then corrective osteotomies will be necessary. This adds to the complexity of the procedure and increases the potential for complications. Significant residual displacement of the tuberosities requires osteotomies and mobilization to allow reattachment with minimal tension. This decreases the risk of fixation failure and redisplacement postoperatively. The decision to proceed with glenoid resurfacing is based on both the preoperative assessment of the symptoms and the intraoperative assessment of the glenoid articular surface (Fig. 9-14). The results of prosthetic replacement for osteonecrosis following fracture depend primarily on the degree of proximal humeral deformity and the need for corrective osteotomies. Proximal humeral replacement for chronic fracture problems (osteonecrosis and other complications) has less satisfactory outcomes and a greater incidence of complications compared with prosthetic replacement for acute proximal humeral fractures.12 Neurologic injury associated with proximal humeral fractures can occur as a result of the injury, a closed reduction maneuver, or operative management. Assessment of nerve function at the time of the initial evaluation is essential, although it can be difficult due to the pain associated with the injury. Every effort must be made, however, to obtain a complete neurologic assessment at the time of injury that includes the axillary, suprascapular, and musculocutaneous nerves and terminal branches of the brachial plexus.27,28 Clinically significant nerve injuries have been reported in 9 to 50% of proximal humeral fractures3,28–30; however, Visser et al31 performed a prospective electromyographic (EMG) study in patients following proximal humerus fractures and documented that 67% of patients had evidence of nerve injuries, with most patients having more than one nerve affected. Of these nerve injuries, 86% involved the axillary nerve and 72% involved the suprascapular nerve; 82% of displaced fractures had an associated nerve deficit; however, 59% of nondisplaced fractures also had EMG evidence of nerve compromise. In this study, all deficits resolved, but recovery of shoulder function was prolonged.31 Fracture-dislocations are more commonly associated with nerve injury (77%) than simple glenohumeral dislocations (48%). Fracture-dislocations also have a greater incidence of multiple nerve involvement and the potential for more significant nerve injury.32,33 Several studies have documented an increased incidence of nerve palsy following proximal humeral fracture in elderly patients. Although permanent nerve palsies occur in up to only 8% of patients sustaining these fractures, they are reported in up to 50% of cases when the fracture and the nerve injury are secondary to blunt trauma to the lateral aspect of the shoulder.27,31,34 This combination of factors results in direct injury to the nerve. Nerve injury can occur as a result of treatment by closed manipulation or operative management. The risk of nerve injury with closed reductions is relatively small. It generally occurs in association with repeated attempts at closed reduction.3 Operative management carries an increased risk of nerve injury, although the incidence remains relatively small.12 In each of these situations, it is essential to document neurologic function at the time of injury and prior to any closed manipulation or operative management. With this approach, nerve compromise as a result of the injury can be clearly differentiated from nerve injury as a result of treatment.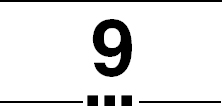
Complications of Proximal Humeral Fractures
 Early Failure of Fixation and Implant Complications
Early Failure of Fixation and Implant Complications

Nonunion

Malunion
Osteonecrosis
Nerve Injury
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree