Chiari and Salvage Osteotomy for the Treatment of Symptomatic Acetabular Dysplasia
Catharina Chiari
Rainer Kotz
Reinhard Windhager
Background and Rationale
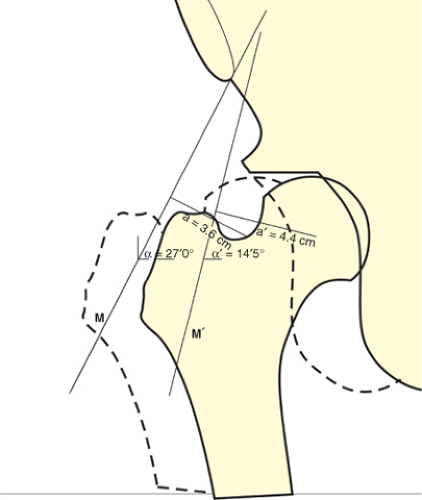
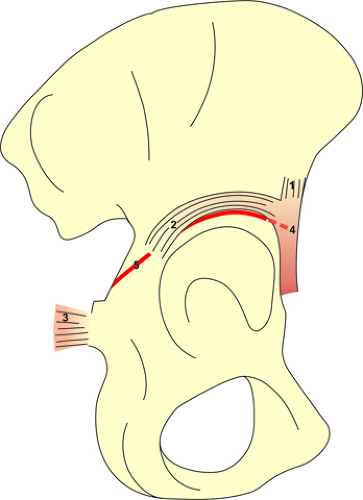
The surgical principle of the Chiari pelvic osteotomy (PO) is a medial displacement of the intact hip joint, which is achieved by an osteotomy just above the acetabulum thus creating a roof for coverage of the femoral head. The interposed joint capsule transforms into fibrocartilage. The procedure was performed first by Karl Chiari at the Vienna University Clinic of Orthopaedics in 1952. The concept was developed because of unsatisfying results of the previously popular shelf operations (1,2), especially in adolescents and adults with hip dysplasia and subluxation of the femoral head. Those techniques were able to build a roof above the femoral head, but not to correct its position, which is crucial to achieve normal biomechanical function by restoring the physiologic lever arm of the pelvitrochanteric muscles (Fig. 34.1) (4). Originally, Chiari applied his technique in a variety of indications including congenital dislocation of the hip in young children, hip dysplasia with or without subluxation of the femoral head in children, adolescents, and adults as well as osteoarthritis of dysplastic hip joints. Later, Chiari himself restricted his indications concerning the treatment of young children under the age of 4 years, where the healthy cartilaginous roof has enough potential of building a functional roof and therefore techniques like the Salter (5), Pemberton (6), or Dega (7) osteotomies have the advantage of providing head coverage by hyaline cartilage (8). Today, the field of indications for the Chiari osteotomy has further narrowed by the introduction of reorientation osteotomies of the acetabulum (9,10) and total hip arthroplasty. Therefore, careful selection of the patients who will benefit from this technique is key for a successful outcome.
Indications
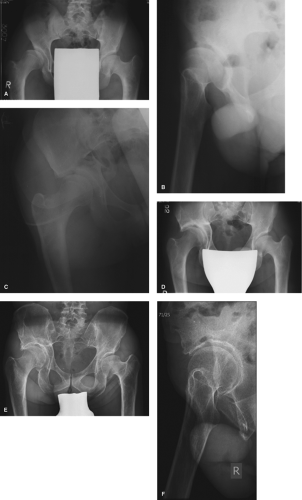
Nowadays the Chiari osteotomy is considered a salvage procedure. In general, this type of osteotomy is used for the reconstruction of incongruent hip joints. Severe neglected developmental dysplasia of the hip (DDH) is a classic indication (Fig. 34.2A–F). Very shallow acetabula with a short roof do not provide enough bone socket for reorientation osteotomies. Typically, the femoral head is lateralized or subluxed by a gliding movement, which leads to insufficiency of the gluteal muscles. The Chiari osteotomy addresses the
cranial instability by forming a bony shelf with interposition of the joint capsule underneath and at the same time restores biomechanics by medializing the femoral head to a more physiologic position. In cases where a secondary acetabulum is present the osteotomy is performed just above it (Fig. 34.3A–C). The age group of these patients reaches from late childhood to early adulthood. Early osteoarthritis after DDH is an indication in the younger patient (less than 45 years). Only slight to moderate changes of the cartilage with a well-preserved joint space should be present (11,12). Apart from DDH, the Chiari PO is a useful operation for patients with neuromuscular disorders, who develop hip subluxation. Especially in walkers the hip function is improved by stabilizing the femoral head cranially by the newly formed shelf. In most of those cases a capsulorrhaphy and varisation osteotomy on the femoral side need to be performed simultaneously. Another group of patients, who benefit from this procedure are patients with severe femoral head deformities causing hip joint incongruity such as sequelae of Perthes disease or avascular necrosis of the femoral head (idiopathic or as a complication of DDH). Posttraumatic or postinfectious hip deformities represent rare indications.
cranial instability by forming a bony shelf with interposition of the joint capsule underneath and at the same time restores biomechanics by medializing the femoral head to a more physiologic position. In cases where a secondary acetabulum is present the osteotomy is performed just above it (Fig. 34.3A–C). The age group of these patients reaches from late childhood to early adulthood. Early osteoarthritis after DDH is an indication in the younger patient (less than 45 years). Only slight to moderate changes of the cartilage with a well-preserved joint space should be present (11,12). Apart from DDH, the Chiari PO is a useful operation for patients with neuromuscular disorders, who develop hip subluxation. Especially in walkers the hip function is improved by stabilizing the femoral head cranially by the newly formed shelf. In most of those cases a capsulorrhaphy and varisation osteotomy on the femoral side need to be performed simultaneously. Another group of patients, who benefit from this procedure are patients with severe femoral head deformities causing hip joint incongruity such as sequelae of Perthes disease or avascular necrosis of the femoral head (idiopathic or as a complication of DDH). Posttraumatic or postinfectious hip deformities represent rare indications.
Contraindications are advanced dysplastic osteoarthritis of the hip and age over 44 years (11). The Chiari PO should not be performed in patients with a hip flexion less than 90 degrees, as range of motion tends to deteriorate after the surgery (8,13).
Clinical Presentation and Preoperative Preparation
Physical examination should include exact documentation of range of motion. Especially, limited flexion less than 90 degrees is a contraindication. Limping is present in most patients and can be caused by muscular insufficiency or pain. A positive Trendelenburg sign confirms insufficiency of the gluteal muscles. In those patients preoperative physiotherapy with strengthening of the pelvitrochanteric
muscles will facilitate postoperative rehabilitation. Pain needs to be assessed, which usually increases with longer walking distances and prolonged standing and can also continue at rest.
muscles will facilitate postoperative rehabilitation. Pain needs to be assessed, which usually increases with longer walking distances and prolonged standing and can also continue at rest.
Conventional radiographs including a standing AP pelvis and a false-profile view (14) are used for preoperative planning. The osteotomy starts at the lateral edge of the acetabulum and continues ascending 15 degrees to the Hilgenreiner line (Fig. 34.4). Congruency of the joint, the shape of the femoral head, and its coverage are assessed. The center edge (CE) angle (15) and the vertical-center-anterior (VCA) margin angle (14) are measured to quantify lateral and anterior head coverage. Grading of osteoarthritis (16) should also be performed. Long leg standing x-rays are obtained to measure leg length discrepancies, which are often present because of asymmetric head–neck shaft angles or subluxation of the femoral head. Nowadays radial sequencing magnetic resonance with currently developed cartilage imaging sequences can be a useful tool to obtain more detailed information about the condition of the cartilage and labrum (17). Computer tomography with 3D reconstruction is ordered in special cases where bony deformities need further assessment.
Ideally, the patient donates two blood units in advance. Usually blood loss is limited and stops after medial displacement of the osteotomy, however there is always the risk of increased bleeding from the bone and vessel injuries.
Patient information is important, as the patient needs to be aware that this kind of surgery does not restore a healthy hip joint and future total hip replacement will be necessary in most of the cases. The patient must be informed about all possible complications (discussed below) and about the fact that range of motion can deteriorate after the surgery. Limping is noted in many patients postoperatively and they must be aware that intensive rehabilitation is necessary to gain back muscular function. In female patients with bilateral osteotomies child delivery can be compromised and cesarean section is advised (18).
Surgical Technique
We describe the original technique that has been unchanged at the Department of Orthopaedics of the Medical University of Vienna except for transfixation of the osteotomy by Kirschner wires, which was introduced in 1982 (4,8,13,19). More recently screws are preferred for even more stable fixation.
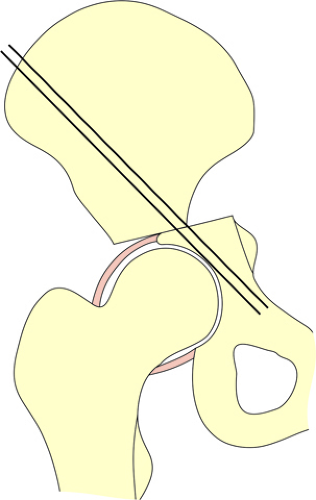
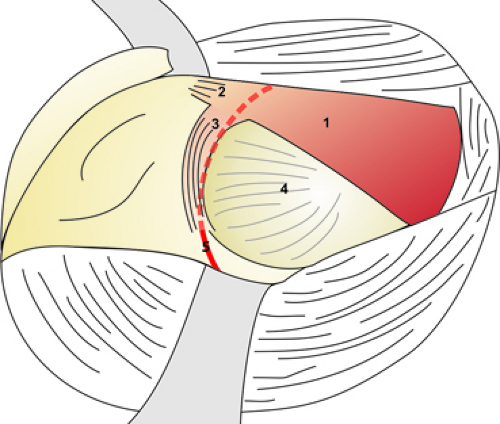
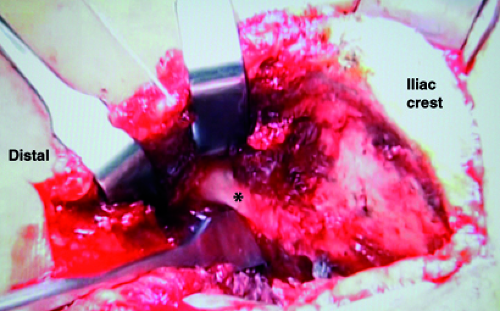
The patient is positioned on a traction table. The affected hip is abducted 20 degrees and rotated outward 30 degrees. Thus, the gluteal muscles are relaxed and the major trochanter is moved backward, which allows for more space along the anterolateral route. An image intensifier is inserted to the operation field from the contralateral side of the table. It is advisable to check its position and the image quality before draping. The skin incision is located 3 cm lateral to the iliac crest and is about 10 cm long. It starts 5 cm proximal to the anterior superior iliac spine and is continued slightly curved along the direction of the tensor fasciae latae muscle. The incision of the tensor fascia should be performed rather laterally to protect the lateral femoral cutaneous nerve. The fascia is cut to its origin at the iliac crest, the muscle should be dissected carefully only as far as needed for sufficient exposure of the acetabulum. The tensor muscle is retracted laterally. Then the iliac crest is exposed subperiosteally. First the muscles on the inner side of the pelvis are pushed back and a curved periosteal elevator, which always is in contact with the bone, is advanced to the sciatic notch. The rasp is replaced by a blunt retractor to protect the sciatic nerve. Additionally, a sponge is placed on the medial side of the iliac wing to minimize blood loss and enhance protection of the sciatic nerve. We recommend the use of specially developed 2-cm wide flexible radiolucent spatula, which can be bent to custom (20). Then the tensor fasciae latae muscle and the anterior part of the gluteus medius muscle are pushed back until the joint capsule is exposed, blunt dissection of the gluteus minimus muscle is carried out to sufficiently visualize the capsule. A second retractor is passed from the lateral side into sciatic notch for protection of the gluteal vessels and nerves. The tips of the both retractors should touch each other in the sciatic notch (Fig. 34.5). The reflected rectus tendon is dissected from the capsule with curved scissors to prepare the osteotomy site. The location of the osteotomy is precisely between the capsular attachment to the iliac bone and the reflected rectus tendon. The dorsal aspect of the reflected tendon needs to be incised as it crosses the osteotomy line (Fig. 34.6). The image intensifier is used
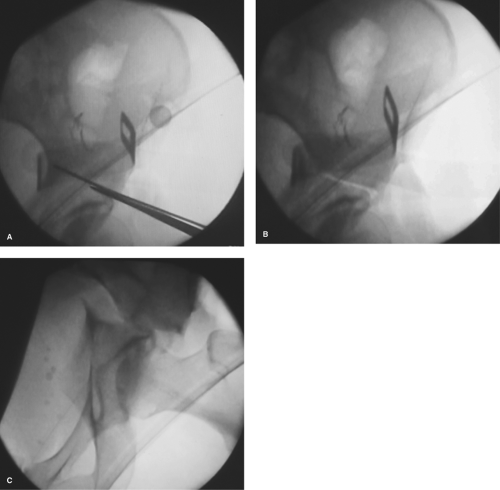
for monitoring the osteotomy. We do not recommend the use of a Gigli saw as it is technically impossible to achieve a correct ascending and curved orientation of the osteotomy. A straight chisel is inserted between the reflected rectus tendon and the joint capsule at the most cranial point of the curved osteotomy line (Fig. 34.7). In some cases drilling a K-wire can be helpful to mark the direction of the osteotomy, the chisel can be inserted underneath, which prevents it from slipping off cranially (Fig. 34.8A). The entry point should be checked with the image intensifier. The lateral cortex is opened in a curved line, first anteriorly ending below the anterior inferior iliac spine and then posteriorly ending in the sciatic notch just above the insertion of the sacrospinal ligament. Throughout the osteotomy it is crucial to direct the chisel 10 to 15 degrees upward toward the inner table of the iliac bone. The position of the chisel needs to be changed several times, which is facilitated by using two or three chisels next to each other and exchanging them alternately. The osteotomy is completed through the medial cortex (Fig. 34.8B). The completion of the osteotomy should be checked under image control by pivoting the chisel and thus slightly distracting the osteotomy gap. Horizontal or downsloping osteotomies need to be avoided at all means, as they will prevent medialization of the distal fragment. Too steep osteotomies have the risk of injuring the sacroiliac joint. After removal of the retractors medialization of the hip joint is achieved by forced abduction under release of the traction and neutral rotation (Fig. 34.8C). After the displacement maneuver the hip abduction should be reduced to 30 degrees. The amount of displacement is correct when the femoral head is fully covered by the bony shelf. Excessive displacement can be reduced by traction. Except for rare cases with instability Chiari did not use any internal transfixation of the osteotomy, but applied a hip spica cast in abduction for 3 to 4 weeks. Since 1982 two parallel 2-mm Kirschner wires are inserted from dorsolateral to ventromedial through the iliac crest into the distal fragment, therefore the plaster cast is not necessary (13). Since recently we use cannulated short-threaded screws for osteosynthesis. Deep drains should be
avoided to prevent excessive blood loss from the osteotomy, a subcutaneous drain can be used. Abdominal wall muscles and abductor muscles are connected by sutures to cover the iliac crest. This enhances the stability of the osteotomy and allows firm closure of the wound.
for monitoring the osteotomy. We do not recommend the use of a Gigli saw as it is technically impossible to achieve a correct ascending and curved orientation of the osteotomy. A straight chisel is inserted between the reflected rectus tendon and the joint capsule at the most cranial point of the curved osteotomy line (Fig. 34.7). In some cases drilling a K-wire can be helpful to mark the direction of the osteotomy, the chisel can be inserted underneath, which prevents it from slipping off cranially (Fig. 34.8A). The entry point should be checked with the image intensifier. The lateral cortex is opened in a curved line, first anteriorly ending below the anterior inferior iliac spine and then posteriorly ending in the sciatic notch just above the insertion of the sacrospinal ligament. Throughout the osteotomy it is crucial to direct the chisel 10 to 15 degrees upward toward the inner table of the iliac bone. The position of the chisel needs to be changed several times, which is facilitated by using two or three chisels next to each other and exchanging them alternately. The osteotomy is completed through the medial cortex (Fig. 34.8B). The completion of the osteotomy should be checked under image control by pivoting the chisel and thus slightly distracting the osteotomy gap. Horizontal or downsloping osteotomies need to be avoided at all means, as they will prevent medialization of the distal fragment. Too steep osteotomies have the risk of injuring the sacroiliac joint. After removal of the retractors medialization of the hip joint is achieved by forced abduction under release of the traction and neutral rotation (Fig. 34.8C). After the displacement maneuver the hip abduction should be reduced to 30 degrees. The amount of displacement is correct when the femoral head is fully covered by the bony shelf. Excessive displacement can be reduced by traction. Except for rare cases with instability Chiari did not use any internal transfixation of the osteotomy, but applied a hip spica cast in abduction for 3 to 4 weeks. Since 1982 two parallel 2-mm Kirschner wires are inserted from dorsolateral to ventromedial through the iliac crest into the distal fragment, therefore the plaster cast is not necessary (13). Since recently we use cannulated short-threaded screws for osteosynthesis. Deep drains should be
avoided to prevent excessive blood loss from the osteotomy, a subcutaneous drain can be used. Abdominal wall muscles and abductor muscles are connected by sutures to cover the iliac crest. This enhances the stability of the osteotomy and allows firm closure of the wound.
Postoperative Rehabilitation Protocol
First postoperative day: isometric exercises; second postoperative day: removal of the drainage, passive motion of the hip joint with continuous passive motion (CPM), sitting, and standing. Then the patient is mobilized nonweight bearing until the K-wires are removed after 3 to 4 weeks. Partial weight bearing is conducted until the osteotomy is healed. When screws are used for osteosynthesis weight bearing should only start after healing of the osteotomy. Intensive training of the gluteal muscles should be started right after the surgery. If limping is not resolved by outpatient therapy, the patient should be referred to an inpatient rehabilitation program.
Perioperative Medication
Anticoagulation treatment is performed according to the protocol of total hip arthroplasty. As a gold standard we use low–molecular-weight heparin (LMWH) until full weight
bearing. Novel oral anticoagulants (NOACs) are approved for hip arthroplasty. For pelvic osteotomies they would be used off-label and bear the risk of postoperative bleeding, which cannot be controlled by an antidote. Perioperative antibiotic prophylaxis is administered until the second postoperative day.
bearing. Novel oral anticoagulants (NOACs) are approved for hip arthroplasty. For pelvic osteotomies they would be used off-label and bear the risk of postoperative bleeding, which cannot be controlled by an antidote. Perioperative antibiotic prophylaxis is administered until the second postoperative day.
Simultaneous Femoral Procedures
Intertrochanteric varus-producing osteotomies can be indicated in cases with subluxation and a high neck shaft angle. Distal advancement of the greater trochanter is sometimes necessary to improve tension of the pelvitrochanteric muscles. Korzinek and Muftic´ (21) showed in a clinical and biomechanical study that lateralization and distalization with or without varisation gives better results in terms of gluteal muscle force. Valgus osteotomies according to the principles of Pauwels (22) were performed by Chiari himself in cases with an oval femoral head, where he considered that the shelf of the PO would lead to high contact pressures at the apex of the femoral head. We currently do not recommend such a procedure. Abduction and adduction radiographs as well as an arthrogram are recommended for preoperative planning of femoral osteotomies. The PO is usually done first to avoid stressing the femoral osteosynthesis (23). However, it is not proved that intertrochanteric osteotomies improve the long-term result (13).
Complications and Technical Issues
The sciatic nerve can be injured intraoperatively. In this case nerve palsy is present immediately after the surgery and the patient needs to be revised as soon as possible. Nerve decompression is performed via a dorsal approach and if a nerve discontinuity is detected the nerve is reconstructed microsurgically. If sciatic nerve palsy occurs at an interval after the operation the most likely cause is a hematoma, which can be confirmed by ultrasound or CT imaging. In those cases conservative treatment is usually sufficient. Lesions of the femoral or peroneal nerve are also possible, although less likely. Injury of the lateral cutaneous femoral nerve can happen at the approach or at wound closure. The nerve should be revised and decompressed up to 3 months postoperatively.
Flexion contractures can be caused by scarring and shrinkage of the tensor fasciae latae and sartorius muscle at their insertion (8). Intra-articular adhesions also produce joint stiffness. This situation especially occurs when the capsule is damaged intraoperatively and the tissue for interposition under the shelf is destroyed. Those complications were more frequent at the time when a plaster cast was used for immobilization. Since internal fixation is used, CPM exercises are started on the first day after surgery to maintain full range of motion.
A wrong level of the osteotomy causes complications. A too low osteotomy level can lead to injury of the capsule with the risk of joint stiffness as mentioned above. Meticulous preparation of the reflected rectus tendon is key, as this is the only orientation guideline at this point of the operation. Preparation of the capsule can be difficult when the femoral head is subluxed and a secondary acetabulum is present. In those cases the osteotomy needs to be performed a little higher to avoid too much pressure on the femoral head (Fig. 34.3). Prior traction and reduction of the femoral head is not recommended as they have the risk of avascular necrosis of the femoral head (8




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree