CHAPTER 17 Cervical Spine
Surgical Approaches
Surgical Anatomy
Surface Anatomy and Skin
An understanding of the relationship of surface landmarks to anatomic structures in the neck is useful for localizing vertebral levels. The hyoid bone lies at the level of C3, the thyroid cartilage lies at the level of C4, and the cricoid cartilage lies opposite C6.1 Gentle but firm palpation laterally allows inspection of the transverse processes. Superiorly, the transverse process of the atlas is most prominent and is found just anterior and inferior to the mastoid process. To help differentiate it from the skull, rotation of the head shows the atlas moving independently from the skull. The anterior tubercle of the transverse process of the sixth cervical vertebra, Chassaignac tubercle, is an important palpable landmark. Posteriorly, in the midline, the first bony prominence palpated inferior to the occiput is the spinous process of the second vertebra. The next palpable spinous processes are typically from the sixth and the seventh vertebrae, with the seventh being the most prominent.
Osseous Anatomy and Bony Articulation
The axis, or C2, is characterized by an odontoid process or dens that projects upward anteriorly, articulating with the posterior aspect of the anterior arch of the atlas as a synovial joint. At its narrowest portion, at the base of the dens, the coronal and sagittal plane diameters are 8 to 10 mm and 10 to 11 mm.2,3 Posteriorly, the axis has a large lamina and a bifid spinous process, which serve as attachments for the rectus major and inferior oblique muscles. The zone between the lamina and the lateral mass of the axis is indistinct, and posteriorly the neural arch connects to the body by large pedicles that are 8 mm wide and 10 mm long.4 Lying directly anterolateral to the pedicle is the vertebral artery, which runs through the foramen transversarium. The pedicle of the axis projects 30 degrees medially and 20 degrees superiorly from a posterior-to-anterior direction.3
The bony articulations of the upper cervical spine (occiput-C1-C2) are unique and warrant special attention (Fig. 17–1). The atlanto-occipital articulation is a shallow ball-and-socket joint allowing for considerable motion mostly in flexion, extension, and lateral bending. The greatest degree of flexion and extension of any cervical articulation occurs at this level (25 degrees).5 Lateral displacement is minimized because the lateral wall of the cup-shaped articulation of the atlas is higher than the medial wall. The superior articular surface of the atlas projects cephalad and medially, articulating with the occipital condyle, which projects caudad and laterally. Conversely, the inferior articular surface of the atlas projects caudad and medially and articulates with the laterally projecting superior facet of the axis. As a result of this bony configuration, axial loads on the atlas tend to result in horizontal displacement of the lateral masses.6
The atlantoaxial articulation provides about 50% of rotatory motion of the cervical spine.5,7 The transverse ligament, which spans across the arch of the atlas, holds the odontoid process against the anterior arch of the atlas, creating a pivot joint with a synovial membrane and capsular ligaments anteriorly and posteriorly to the dens. This transverse ligament is the principal stabilizing structure for the atlantoaxial articulation and averages 21.9 mm in length.8 The transverse ligament has superior and inferior extensions, which form the cruciform ligament of the atlas, connecting it to the anterior edge of the foramen magnum and posterior aspect of the C2 body. To allow more rotatory motion, the inferior facets of the atlas are flatter and more circular than the superior facets and face inferiorly to articulate with the axis.
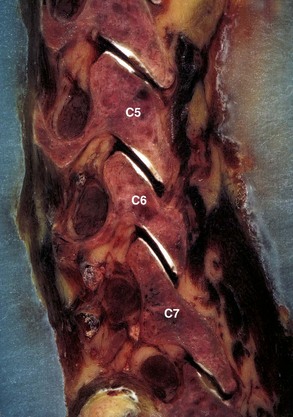
The inferior surface of the vertebral body is convex in the coronal plane and concave in the sagittal plane, with the anterior lip occasionally overlapping the inferior vertebra.8 Conversely, the superior surface of the vertebral body is convex or straight in the sagittal plane and concave in the coronal plane, creating projections on either side of the lateral superior surface, called the uncus, or hook. These processes project upward and conform to small grooves in the inferolateral border of the cephalad vertebra, forming the uncovertebral joints, or joints of Luschka. The width and depth of the vertebral surfaces average 17 mm and 15 mm from C2 to C6 and increase to about 20 mm and 17 mm at C7. Vertebral heights on the posterior wall in the mid-sagittal plane range from 11 to 13 mm.9
The pedicles project posterolaterally from the vertebral body and join the lamina to form the vertebral arch. From C3 to C7, the angulation of the pedicles varies from 8 degrees below to 11 degrees above the transverse plane and decreases from 45 degrees to 30 degrees in relation to the sagittal plane.9 The width and height of the pedicles increase slightly in size from C3 to C7, and average diameters are 5 to 6 mm and 7 mm. The lateral wall of the pedicle is thinner than the medial wall and should be taken into consideration if attempts at pedicle fixation are considered in this region.10–12
In the lower cervical spine, the neural foramina are bounded anteriorly by the uncinate process, the posterolateral aspect of the intervertebral disc, and the inferior portion of the vertebral body; posteriorly by the facet joint and superior articular process of the vertebral body below; and superiorly and inferiorly by adjacent pedicles. Vertebral notches located on the superior and inferior aspect of each pedicle contribute to the size of the neural foramina, which are 9 to 12 mm in height, 4 to 6 mm in width, and 4 to 6 mm in length and are aligned 45 degrees to the sagittal plane.13,14 They can be visualized radiographically with oblique views, with the right neural foramina outlined on the left posterior oblique view and the left neural foramina outlined on the right posterior oblique view.
The spinal canal is triangular and at all levels in the cervical spine is significantly greater in the medial-to-lateral dimension than in the anterior-to-posterior dimension. The cross-sectional area of the spinal canal is largest at C2 and smallest at C7, with a sagittal diameter of about 23 mm at C1 and 20 mm at C2, decreasing to 17 to 18 mm at C3-6 and to 15 mm at C7.7 This is one reason that the passage of sublaminar wires is safer in the upper cervical spine than in the lower cervical spine.
The lateral mass, an important structure for posterior cervical plate-screw systems, forms at the junction of the lamina and the pedicle and gives rise to the superior and inferior articular processes. These processes project upward and downward and are angled approximately 45 degrees cephalad from the transverse plane and gradually assume a more vertical position as they descend into the thoracic region (Fig. 17–2). The articular process of the superior facet faces posteriorly, whereas the inferior facet of the upper vertebra faces anteriorly, and the facets oppose one another to form a zygapophyseal joint. The facet joints are true diarthrodial joints with articular cartilage and menisci surrounded by a fibrous capsule lined by a synovial membrane. The interfacet distances are relatively constant between levels, with individual variations ranging from 9 to 16 mm (average 13 mm).4,15
The cervicothoracic junction is a transition region, with C7 having similar anatomic characteristics at T1 and T2. The dimensions of the vertebral body and the sizes of the transverse processes and spinous processes are larger at C6 and C7. Additionally, dimensions of the spinal canal decrease at C6 and C7, representing a distinct transition to the thoracic region. The articulating facet joint between C7 and T1 resembles the thoracic facet joint, and the lateral mass of C7 is thinner than that of upper levels. Morphologic characteristics of pedicles of C7, T1, and T2 were obtained with respect to diameters, depths, and medial angulations. Inner diameters of the pedicles at C7, T1, and T2 from medial to lateral plane averaged 5.2 mm, 6.3 mm, and 5.5 mm. Medial angulations were 34 degrees, 30 degrees, and 26 degrees at C7, T1, and T2.9,16 These morphologic characteristics should be remembered when performing transpedicular procedures in the cervicothoracic region.
Ligaments
The transverse ligament is the major stabilizer of the atlantoaxial complex (Fig. 17–3). It attaches laterally to tubercles located on the posterior aspect of the anterior arch of C1, where it blends with the lateral mass. Secondary stabilizers include the thick alar ligament, which arises from the sides of the dens to the medial aspects of the condyles of the occipital bone, and the apical ligament, which arises from the apex of the dens to the anterior edge of the foramen magnum. In some individuals, an anterior atlantodental ligament exists connecting the base of the dens to the anterior arch of the atlas.17 The tectorial membrane, the superior continuation of the posterior longitudinal ligament, covers the dens and all the occipitoaxial ligaments and extends from the posterior body of C2 to the basilar portion of the occipital bone and the anterior aspect of the foramen magnum.
The bodies of the lower cervical vertebrae (C3-7) are connected by two longitudinal ligaments and the intervertebral discs. The anterior longitudinal ligament is a strong band that attaches from the skull, as the anterior atlanto-occipital membrane, and continues caudad over the entire length of the spine down to the sacrum. The anterior longitudinal ligament is thinner and more closely attached at the intervertebral disc margins than at the anterior vertebral surfaces.18 The anterior longitudinal ligament also sweeps around and envelops the lateral aspect of the vertebral bodies under the longus collis muscle, and the lateral extension is continuous with the deep layer of the posterior longitudinal ligament in the region of the intervertebral foramina.
The posterior longitudinal ligament, lying within the vertebral canal on the posterior aspect of the vertebral body and intervertebral disc, is wider in the upper cervical spine than the lower cervical spine.18 Superiorly, it is continuous with the tectorial membrane, and as it descends it widens over the intervertebral discs and narrows behind each vertebral body. The posterior longitudinal ligament supplies additional strength and stability to the posteromedial fibers of the anulus. There is an area of relative weakness in the posterolateral corners of the disc, however, at the junction of the posterior longitudinal ligament and uncinate process; as a result, it is the site of most cervical disc herniations.19 According to Hayashi and colleagues,20 the posterior longitudinal ligament is double-layered, and the deep layer sends fibers to the anulus fibrosus and continues laterally to the region of the intervertebral foramina. The superficial or more dorsal layer of the posterior longitudinal ligament is adjacent to the dura mater and continues as a connective tissue membrane, which envelops the dura mater, nerve roots, and vertebral artery, suggesting that this membrane may serve as a protective barrier.
Intervertebral Discs
Intervertebral discs are present between vertebrae except at the atlantoaxial level. Each intervertebral disc is an avascular structure that consists of the nucleus pulposus at the interior of the disc, the outer anulus fibrosus, and the cartilaginous endplates adjacent to the vertebral surfaces. The nucleus pulposus functions as a shock absorber, and the anulus fibrosus maintains the stability of the motion segment. With increasing age, the margin between the nucleus pulposus and anulus fibrosus becomes less distinct, and often by age 50 the nucleus pulposus has become a fibrocartilaginous mass similar to the inner zone of the anulus fibrosus.21
The anulus has an outer collagenous layer, in which the fibers are arranged in oblique layers of lamellae. The outermost fibers of the anulus fibrosus are contiguous with the anterior and posterior longitudinal ligaments and are firmly attached to the adjacent vertebral endplates. The fibers of the lamella run perpendicular to the fibers of the adjacent lamella. The collagen fibers in the posterior portion of the disc run more vertical than oblique, and this may account for the relative frequency of radial tears seen clinically. The discs are shaped to conform to the surface of the bodies; the superior surface of the disc is concave, and the inferior surface of the disc is correspondingly convex in the coronal plane. The discs are also slightly thicker anteriorly than posteriorly, which contributes to the lordotic posture of the cervical spine. The cervical intervertebral discs allow some translational movement in the sagittal plane, but the uncinate processes resist lateral movement. The uncinate process, located in the posterolateral aspect of the disc, also helps prevent disc herniations in this area. Degeneration of the anulus fibrosus (Fig. 17–4) in the cervical region is similar to the lumbar region in that concentric, transverse, and radial tears of the anulus occur, and the radial tear in the posterior aspect of the disc may be more clinically significant.
The cartilaginous endplate is a layer of hyaline cartilage resting on the subchondral bone and serves as a barrier between the pressure of the nucleus pulposus and the adjacent vertebral bodies. This cartilage is a growth plate and responsible for endochondral ossification during growth (Fig. 17–5). The cartilaginous endplates also allow the insertion of the inner fibers of the anulus fibrosus and the diffusion of nutrients from the subchondral bone to the disc.
Neural Elements
The cervical cord emerges from the foramen magnum as a continuation of the medulla oblongata. There is considerable variation in size of the spinal cord; however, in general, owing to the increased nerve supply to the upper limbs, the cervical cord enlarges from C3 and becomes maximal at C6. Maximal transverse diameters of 13 to 14 mm have been reported,22 with transverse areas ranging from 58.3 ± 6.7 mm2 at C623 to 85.8 ± 7.2 mm2 at C4-5.24
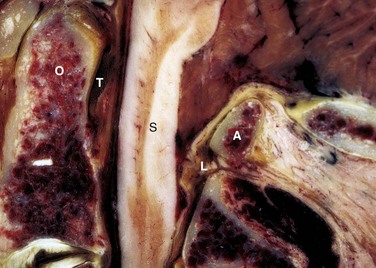
The dorsal sensory rootlets enter the cord through the lateral longitudinal sulcus, and the ventral motor rootlets exit the cord through the ventral lateral sulcus. The six or eight rootlets at each level leave the spinal cord laterally to lie in the lateral subarachnoid space bathed in the cerebrospinal fluid. The rootlets join to form the dorsal and ventral root, which together enter a narrow sleeve of arachnoid and pass through the dura to become a nerve root at each level. The cervical nerve roots that form from the ventral and dorsal nerve rootlet extend anterolaterally at a 45-degree angle to the coronal plane and inferiorly at about 10 degrees to the axial plane.14 The nerve roots enter the intervertebral foramina by passing directly laterally from the spinal canal adjacent to the corresponding disc and over the top of the corresponding pedicle. The anterior root lies anteroinferiorly adjacent to the uncovertebral joint, and the posterior root is close to the superior articular process. The nerve root is positioned at the tip of the superior articular process in the medial aspect of the neural foramen, and it courses more inferiorly to position over the pedicle in the lateral aspect of the neural foramen (Fig. 17–6).
The roots occupy about one third of the foraminal space in the normal spine but much more in the degenerative spine. The roots are located in the inferior half of the neural foramen normally, but the nerve roots occupy a more cranial part of the foramina, and the size of the foramen is diminished if the neck is fully extended.25 The upper half of the neural foramen contains fat and small veins.26 The nerve root is enlarged in the distal aspect of the intervertebral foramen, and the dorsal root ganglion is located just distal to the foramen.27 The dorsal root ganglion is located between the vertebral artery and a small concavity in the superior articular process. Just distal to the ganglion and outside the intervertebral foramen, the anterior and posterior roots join to form the spinal nerve. The spinal nerve divides into dorsal and ventral primary rami branches.
The gray rami from the sympathetic cervical ganglion join the ventral primary rami. There are interconnections between gray rami, the perivascular plexus around the vertebral artery, and the sympathetic trunk, all of which give contributions to the ventral nerve plexus to innervate the anterior longitudinal ligament, outer anulus fibrosus, and anterior vertebral body.28,29 The dorsal nerve plexus receives contributions from the sinuvertebral nerves, which originate from the gray rami and perivascular plexus of the vertebral artery. The dorsal nerve plexus innervates the posterior longitudinal ligament, and the sinuvertebral nerves give branches to the posterior part of the anulus and the ventral part of the dura. The sinuvertebral nerves innervate two or more discs or motion segments.
Vascular Structures
The major blood supply of the cervical cord and the cervical spine is the vertebral artery. Variations of the course of the vertebral artery have been reported.30 In most cases, the vertebral artery originates from the first part of the subclavian artery and begins its ascent behind the common carotid artery between the longus colli and the anterior scalene. In the lower cervical spine, the vertebral arteries are crossed by the inferior thyroid artery and on the left by the thoracic duct. The vertebral arteries course anterior to the ventral rami of the seventh and eighth cervical nerves and the C7 transverse process before entering the C6 transverse foramen, where they ascend within the transverse foramen of C6-C2.
In the foramen magnum region, the vertebral artery gives branches anteriorly that join together to form the single anterior spinal artery, whereas the paired posterior spinal arteries are branches from the posterior inferior cerebellar arteries. The anterior and posterior spinal arteries are the major blood supplies of the spinal cord. The posterior spinal arteries give rise to plexiform channels that are arranged transversely on the dorsum of the cord. The anterior spinal artery supplies most of the spinal cord except the posterior columns.31 The spinal cord also receives blood supplies from radicular arteries or medullary feeders from the vertebral arteries and ascending cervical arteries.31 The segmental arteries that are branches of the vertebral artery are present at each level to supply the vertebrae and surrounding tissues, but only a few segmental vessels give rise to radicular arteries or medullary feeders to the spinal cord. These vessels have a variable distribution, but medullary feeders are more commonly present at C6 and C3 from the left and C5 and T1 from the right.18
Musculature
The musculature of the cervical spine can be grouped into the anterolateral and posterior muscle groups. The anterolateral muscles of the neck include platysma muscle, sternocleidomastoid muscle, hyoid muscles, strap muscles of the larynx, scalene muscles, longus colli muscle, and longus capitis muscle. The posterior musculature is subdivided into superficial, intermediate, and deep muscle groups.32
The posterior muscles of the neck are divided into superficial, intermediate, and deep groups.32 The most superficial muscle is the trapezius, which originates from the external occipital protuberance and the medial nuchal line of C7-T12 spinous processes and inserts on the spine of the scapula, the acromion, and the lateral aspect of the clavicle. The trapezius is innervated by the 11th cranial nerve and functions to extend the head. The intermediate muscles beneath the trapezius muscle are the splenius capitis and splenius cervicis, which originate from the spinous processes of the lower cervical and upper thoracic spines and insert on the transverse processes of the upper cervical spine and the mastoid process. In the deep layer, the erector spinal muscles continue into the cervical region, which includes the iliocostalis laterally; the longissimus cervicis and longissimus capitis centrally; and the spinalis cervicis, semispinalis capitis, and semispinalis cervicis medially. Beneath the semispinalis muscles lie the multifidus from C4-7 and rotatores muscles, which cross only one segment from the transverse processes to the spinous processes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree