Cervical spine fractures
Complexity of geriatric fractures
Assessment of the geriatric cervical spine
General principles of non-operative treatment
Principles of surgical treatment
Treatment of cranio-cervical injuries
Treatment of atlanto-axial injuries
Treatment of subaxial spine injuries
Fractures in patients with ankylosed spines
INTRODUCTION
The geriatric population is expanding, experiencing a longer lifespan and becoming more vigorous later into life with activities such as driving and recreation. With this increase in an active elderly population, cervical spine injuries are becoming a more important part of trauma care. Morbidity and mortality can be decreased with improved awareness of cervical spine injuries and the initiation of appropriate treatment more rapidly. Also, recognition of the unique characteristics of the geriatric spine will help clinicians discern acute injury and provide appropriate care and treatment.
This chapter will review the epidemic of cervical spine injuries in the elderly. The methods of evaluation and radiologic examination will be discussed emphasizing the best available medical evidence. Common classification systems and how they can be applied to geriatric fractures are presented with discussion of how common fracture types behave differently in the geriatric population. These include fractures in patients with ankylosed spine, type 2 odontoid fractures and central cord syndrome. Finally, complications are discussed.
EPIDEMIOLOGY
The geriatric population is increasing by 6% per annum in the United States, while the incidence of cervical fractures in patients above 65 years of age is growing by 21% per annum or 3.5 times faster. The rate of increase was linearly proportional to age so that older groups (>85 years) had even higher fracture rates.1 Further, in a retrospective review of high energy trauma, cervical spine injuries were associated with the highest mortality rates of all orthopaedic injuries with a mortality rate of 47% for cervical spine fractures with neurological deficit and 44% for C2 fractures.2 In a review of another level 1 trauma centre, the mortality rate was 24% for geriatric cervical spine fractures and less than a third were able to return home after injury.3 For fractures that had a neurological deficit the mortality rate was 50%.3
The most common mechanism for trauma in the elderly population is falls, occurring in up to 75% of cases.4 Other common mechanisms include motor vehicle collisions in which the patient is a driver, passenger or pedestrian. Patients commonly have pre-existing comorbidities including hypertension, congestive heart failure, diabetes, dementia, stroke, arrhythmias and chronic obstructive pulmonary disease (COPD), although this association does not imply causality.4 Geriatric patients having ground level falls are more likely to have intracranial haemorrhage, and alcohol intoxication is not as likely as compared to younger patients.5
COMPLEXITY OF GERIATRIC FRACTURES
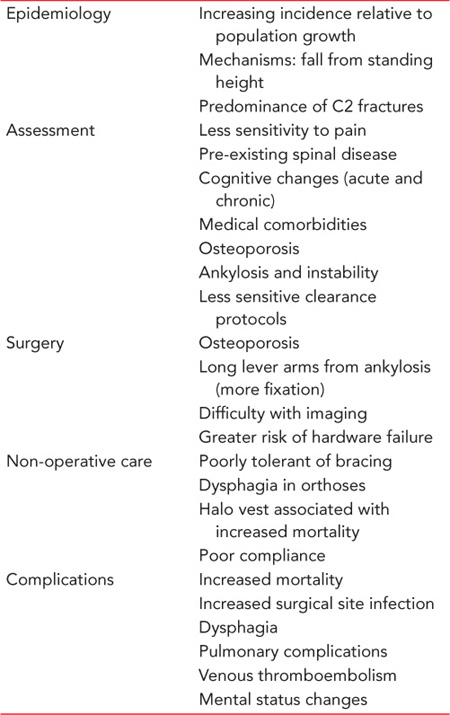
Geriatric patients tolerate trauma poorly and have much lower survival rates and greater complications than younger patients with similar levels of trauma. Many complexities account for this problem including medical comorbidities, declining cognitive abilities, osteoporosis, pre-existing disability and poor social networking (Table 30.1).
Geriatric patients sustaining cervical spine injuries have significantly more medical comorbidities such as hypertension, heart disease, diabetes, lung disease and cognitive medical problems than younger patients.6 Treatment requires balancing treatment of medical comorbidities with spinal care. It is recommended that a multidisciplinary team be created to co-manage these patients similar to programs established for hip fractures.6,7 The medical comorbidities are significant risk factors for the morbidity and mortality associated with spinal fractures in the elderly.
Osteoporosis
Poor bone mineral density (BMD) (whether diagnosed or undiagnosed) predisposes to injury and may complicate surgical reconstruction. It is important to assess the quality of bone in planning treatment as well as for long-term management to prevent further fractures. Surgical strategies to reduce risk of hardware failure include use of more fixation levels and correct balancing to achieve proper alignment, thus reducing unwanted bending moments. Combined anteroposterior surgery, although not desirable, may be needed. Similarly, external mobilization may be required despite its risk of complications.
Table 30.1 Special considerations in geriatric cervical spine fractures
Cognitive changes are commonly seen in geriatric cervical spine patients which may be a major factor producing the fall. If possible, these should be addressed before discharge to avoid future falls. Careful attention to medications, in particular avoiding benzodiazepine and opioids, should be considered. Physical and occupational therapy should focus on balance and fall prevention programs.
ASSESSMENT OF THE GERIATRIC CERVICAL SPINE
Geriatric patients require similar diagnostic protocols to evaluate the cervical spine as all other patients. However, important differences may make the process more difficult and less precise in this population. In general, geriatric patients have less pain, making clinical assessment by history and palpation less sensitive. Further, they are more likely to have long-standing cognitive changes or acute mental status changes reducing clinical discrimination by clinical examination. Medical comorbidities and pre-existing spinal disease require experienced physicians to differentiate these from injury processes.
Screening
Current guidelines by the Eastern Association for the Surgery of Trauma (EAST) recommend that patients meeting National Emergency X-Radiography Utilization Study (NEXUS) criteria do not require radiologic screening.8 The NEXUS criteria are based on a normal cognitive state, no neck pain or tenderness, no neurologic signs or symptoms and no distracting injuries. Distracting injuries include craniofacial trauma, burns, long bone and pelvic fractures, large joint dislocations, thoracic trauma and shock. Distracting injuries significantly reduce the sensitivity of the NEXUS criteria.9 Patients meeting all the criteria are considered low risk and do not require radiographic evaluation. Touger et al. evaluated 2943 elderly patients and compared these to 31,000 non-elderly patients using NEXUS criteria.8 Cervical spine injury was twice as common in the elderly patients. The percentage of patients cleared clinically (meeting NEXUS criteria) was similar between the two groups. The predominant geriatric fracture type was a C2 fracture. Two geriatric patients who were low risk based on NEXUS criteria had occult C2 lateral mass fractures and were treated successfully non-operatively. More recently, Goode et al. questioned the effectiveness of NEXUS criteria in geriatric patients with blunt (high energy) trauma as compared to falls from standing height (low energy).10 They found a significantly higher incidence of cervical spine injury in high energy trauma: 12.8% compared to 4.5%. The sensitivity and positive predictive value of NEXUS criteria in elderly patients were low (65.9% and 19.3%, respectively) and significantly lower than in non-geriatric patients. The authors concluded that NEXUS criteria should not be used in blunt trauma geriatric patients and these patients should undergo CT evaluation regardless of whether they meet NEXUS criteria.
Clinical assessment
The clinical evaluation of the geriatric trauma patient includes special attention given to identifying spinal injuries. The mechanism of injury gives clues to the potential risk of cervical spine injury. However, with concurrent stiffening of the spine from aging and low BMD in elderly patients, even low energy mechanisms may result in significant spinal injuries. The presence or absence of pain and transient or persistent neurologic changes should be noted. The patient’s ability to ambulate after the trauma may give some insight into spinal stability. Physical exam should include observation for signs of cranial or facial trauma which is common in patients with ground level falls. These include contusion about the head and face and facial fractures. The cervical spine is assessed by palpation for tenderness in the midline and then along each lateral mass.
Patients with low-energy falls who meet NEXUS criteria may be cleared without further radiologic imaging.8 After it has been determined that the patient meets NEXUS criteria, they can be checked for pain with neck range of motion. This is best tested using the Canadian C-Spine Rule where right and left rotation is performed actively by the patient under physician supervision.11 Keep in mind that geriatric patients have a high predominance of fractures at C2 and, therefore, may have pain or be unable to perform rotational maneuvers.
Neurologic assessment of all patients should be performed according to criteria described in the Guide to the Neurologic Evaluation of the Spinal Injury Patient by the American Spinal Injury Association (ASIA) (Figure 30.1).12 The neurologic exam includes cranial nerve assessment, motor and sensory tests in the lower and upper extremities, and examination of the perineum. Reflexes are less helpful in geriatric patients unless there are signs of hyperreflexia which may indicate an upper motor neuron lesion from spinal cord compression or injury. In patients with neurologic deficits, the degree of spinal cord impairment is recorded using the ASIA Impairment Scale (Table 30.2). The neurologic exam should be recorded as in Figure 30.1.
Spinal cord injuries are devastating, especially to the elderly where the chance of mortality is greater than 80%. Various spinal cord injury patterns are seen. A complete cord injury is where there is no motor sensory function below the level of injury. Incomplete patterns include anterior cord, Brown-Sequard, central cord and posterior cord syndromes. Anterior cord syndrome causes loss of function of distal motor and pain and temperature functions due to injury of the anterior two-thirds of the spinal cord. Only posterior cord function remains. The prognosis is extremely poor. Brown-Sequard syndrome is a hemicord injury where there is ipsilateral loss of motor function and contralateral loss of sensory function. Central cord syndrome is a common injury pattern seen in elderly patients due to pre-existing cervical stenosis. In this syndrome there is greater loss of upper extremity function than lower extremity function. This pattern of neurologic injury is due to the lamination of axonal tracks where the upper extremities are more medial and thus affected to a greater degree in central cord syndrome than the more laterally placed lower extremity tracts. This prognosis is variable and many patients can make a significant recovery. Posterior cord syndrome is rare; there is only loss of dorsal column function and thus light touch, proprioception and vibration.
The severity of neurologic injury is classified by the ASIA motor score and the ASIA impairment scale.12 The ASIA motor score is based on muscle examination of five key muscle groups in both the upper and lower extremities (Figure 30.1). Each muscle group is scored from 0 to 5. The bilateral sum of all scores ranges from 0 to 100. The ASIA impairment scale is important for prognosis (Table 30.2). An ASIA A is a complete motor sensory quadriplegia, while an ASIA E is normal. ASIA B–ASIA D are incomplete injuries with ASIA B being complete motor loss below the zone of injury but spared distal sensory function. ASIA C and D have retained motor and sensory function with the former having <grade 3 function and the latter ≥grade 3 function.
Radiologic imaging
Radiologic imaging is indicated in patients who fail NEXUS criteria, that is, patients who are symptomatic with pain or neurologic dysfunction, have cognitive impairment or have distracting injuries. Multidetector CT is the diagnostic procedure of choice when evaluating the cervical spine in geriatric patients. Reformations can be created in the axial, sagittal and coronal planes. The overall sensitivity is 99% in identifying cervical spine injury and far better than plain radiography.9 MRI is not useful as a screening tool but is indicated to evaluate soft tissues such as the posterior ligamentous complex, the presence of spinal cord compression or extent of spinal cord injury, progressive neurologic deterioration, and for preoperative planning.13 Many radiographic findings are age related and in these cases MRI can be useful to differentiate these from acute injuries. In addition, in patients with a facet dislocation, a herniated disc may be present and MRI should be used prior to reduction in the neurologically intact patient.
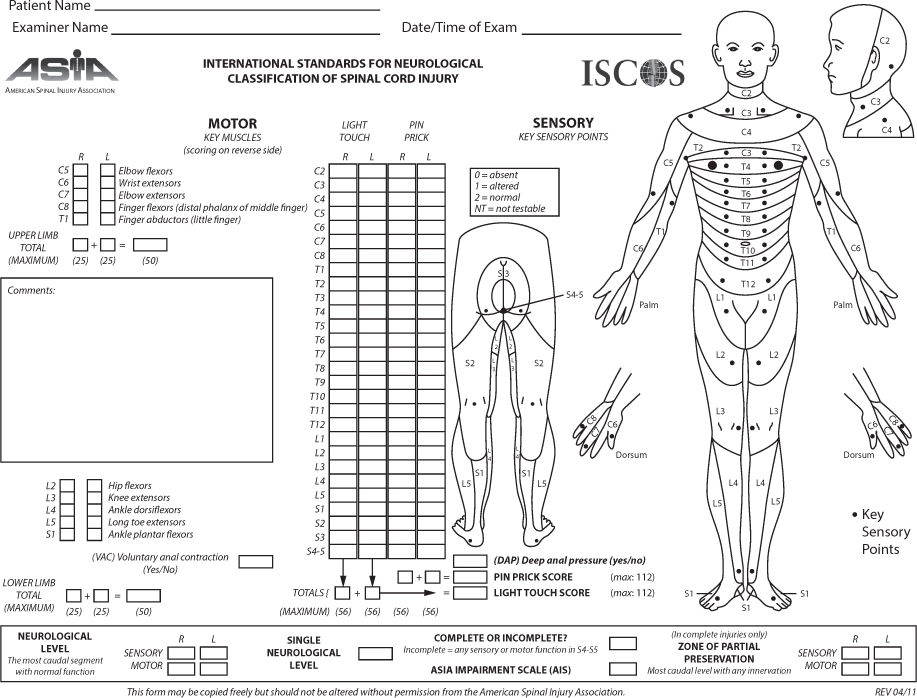
Figure 30.1 American Spinal Injury Association (ASIA) International Standards for Neurologic Classification of Spinal Cord Injury. (Reprinted with permission from American Spinal Injury Association.)
Table 30.2 American Spinal Injury Association Impairment Scale (AIS)
A | No sensory or motor function is preserved in the sacral segments S4–5. |
B | Motor loss complete, retained sensory function below level of injury including sacral region. |
C | Motor function is preserved below the neurological level and more than half of key muscle functions have a muscle grade less than 3. |
D | Motor function is preserved below the neurological level and more than half of key muscle functions have a muscle grade ≥3. |
E | Normal motor and sensory function. |
The interpretation of spine imaging is problematic in geriatric patients. Age related changes may be difficult to differentiate from subtle acute trauma. It is not uncommon for patients to have severe facet degenerative change, especially at C3–4 and C4–5 and have small amounts of anterior subluxation which could be thought secondary to trauma. Further, pre-existing kyphotic changes need to be differentiated from posterior ligamentous injuries. Bony erosive change especially about the dens may predispose to fracture or may even be associated with chronic fracture creating concern for the presence of a new fracture.14 Ankylosed segments from diffuse idiopathic spinal hyperostosis (DISH), surgery or ankylosing spondylitis are predisposed to fracture. Even minor incomplete fractures may be associated with significant instability. Hyperextension injuries may occur through the disc space which may show a normal appearing disc height but which is abnormal for that patient. Differentiating such pre-existing changes from acute trauma is difficult and requires careful examination, experience, interpretation of imaging and patience. Often the patient is immobilized in a collar allowing time to pass until further evaluation as the clinical course may ultimately dictate the status of the cervical spine. MRI may be indicated for specific areas of concern, such as disc or posterior ligamentous injury.
Assessment of bone quality
All geriatric patients with fractures should have assessment of bone quality. This is consistent with the American Orthopedic Association’s ‘Own the Bone’ initiative where orthopaedic surgeons are trained in diagnosing and beginning basic treatment of metabolic bone disease in fragility fracture patients. In most geriatric cervical spine patients, CT has been performed including the thoracolumbar spine. These imaging studies can provide an opportunity to estimate whether patients have osteopenia or osteoporosis. The World Health Organization’s criterion for osteoporosis is a DEXA T score of less than –2.5, while osteopenia is between –1 and –2.5. Normal bone density is T scores greater than –1. However, patients having fragility fractures, including those of the cervical spine, are diagnosed as osteoporotic, despite T scores being greater than –2.5.
If available, thoracolumbar CT can be used to estimate BMD. All CT determines the X-ray attenuation coefficient for each voxel of tissue scanned. This is termed the Hounsfield unit (HU) and is the amount of X-ray energy absorbed per voxel of tissue. For bone, HU is directly related to the BMD. HUs are scaled with air equal to –1000 and water equal to 0. Cortical bone is generally 300–500, while normal cancellous bone is greater than 125.
HUs can be measured using the tool platform of most picture archiving and communication systems (PACS). An elliptical region of interest (ROI) is drawn as large as possible on an axial section of the mid-body of a non-fractured lumbar spine vertebral body (Figure 30.2). The ROI should include only trabecular bone without degenerative changes or bony defects. The PACS tool will report an average HU. Schreiber et al. reported HUs in patients with normal BMD based on DEXA T score.15 Normal T scores (greater than –1.0) had HU >118 while osteopenic patients (T score less than –1 to more than –2.5) had thresholds between 93 and 108, and osteoporotic had HU <95. Patients with an abnormal HU should be considered for further evaluation of their metabolic bone disease, including DEXA.
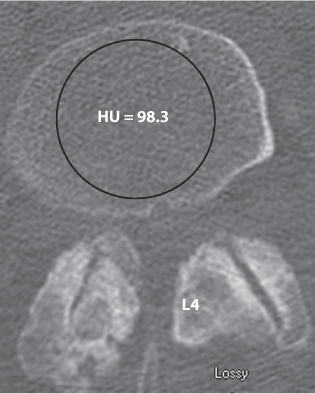
Figure 30.2 A region of interest (ellipse) is drawn in the L4 mid-vertebral body of an 84-year-old man with a C2 fracture. The picture archiving and communication systems (PACS) software reports mean Hounsfield units of 98.3 which is low indicating, at a minimum, osteopenia.
Another important consideration is calcium and vitamin D serum levels. After trauma, these values change due to production of acute phase reactive proteins and may not be reliable indicators of normal steady state conditions. Although recent recommendations are to check these levels during initial hospitalization, it may be more appropriate to evaluate them 4–6 weeks later. In the majority of patients, it is safe to simply prescribe calcium supplementation (1200 mg/day) based on dietary conditions and 2000 units of vitamin D3.
Sarcopenia is the loss of muscle mass from aging and is strongly correlated with BMD and risk of falls. Sarcopenia is increasingly being identified as a potential cause of fracture and an opportunity for treatment. Evaluation of nutrition and counseling may be considered to aid management of osteoporosis and also for fracture healing.
DEXA is the gold standard to diagnose osteoporosis and osteopenia. While useful to definitively diagnose and monitor treatment, it has no role during the acute hospitalization of patients with geriatric fractures and should be delayed until follow-up. Vertebral fracture assessment and trabecular bone scores are new quantitative techniques that may aid in evaluating quality of bone.
Vertebral artery injury
The vertebral arteries arise from the subclavian artery and ascend into the neck. The cervical components of vertebral arteries are divided into four segments. Segment one (V1) is the extra spinal part extending from the subclavian artery to where the vertebral artery enters the spine at the C6 foramen transversarium. Part V2 is where the vertebral artery ascends within the subaxial spine in the foramen transversarium up to C2. In the V3 segment, the vertebral artery ascends vertically from the C2 transversarium to the C1 foramen transversarium and then turns posteriorly and medially lying on the cranial surface of the lateral arch of the atlas. Segment V4 of the vertebral artery turns rostrally, penetrates the dura and passes anteriorly to the medulla combining with the contralateral vertebral artery to form the basilar artery. Normally, the left side is more dominant than the right side.
In geriatric patients, atherosclerosis and poor vessel compliance can create anomalies of the vertebral artery and make the vessels more prone to injury during blunt trauma. Additionally, pre-existing cerebrovascular disease may compromise cranial blood flow in patients with blunt cervical trauma associated with cervical spine fractures. Blunt head and neck trauma has recently been identified as a potential factor for stroke from vertebral artery injury and screening protocols have been developed.16,17 Cervical spine fractures are a significant risk factor for vertebral artery injury. Specific fracture types include any fracture of C1, C2 or C3, occipito-cervical dissociation, subaxial fracture dislocation, subluxations and fractures that involve the foramen transversarium. It is recommended that patients having these fractures undergo cerebrovascular imaging, preferably with CT angiography (CTA). MRA may be performed alternatively, but is not as sensitive as CTA.
The diagnosis and treatment of vertebral artery injuries is controversial among spine surgeons. Although up to 25% of patients with cervical spine fractures may have a vertebral artery injury, it is not clear if these are clinically significant or result in neurologic injury (stroke).17 Therefore a question remains if these should be diagnosed and treated. Neurologic injuries from the vertebral artery in cervical spine patients include death from brain stem stroke, ‘locked-in’ syndrome and asymptomatic cerebellar strokes. However, the majority of patients with vertebral artery injuries associated with cervical spine fractures are asymptomatic without evidence of stroke or have incidental cerebellar or small brain stem lesions on imaging.18 It is felt that in the majority of symptomatic patients, vertebral artery injuries were caused directly from the initial blunt trauma.18 No information is available that provides evidence that treatment of a vertebral artery injury associated with cervical spine fracture is beneficial. Recent guidelines recommend patients at high risk for vertebral artery injury should undergo CTA. If the patient is asymptomatic then it is recommended that anti-platelet therapy be administered if not contraindicated.18
CLASSIFICATION OF INJURY
Cervical spine injuries are classified similarly to those in non-geriatric patients. Common names are assigned based on morphologic features. After a morphologic description, the severity of injury is estimated. Because of the unique anatomic features, the cervical spine will be divided into cranio-cervical, atlanto-axial and subaxial.
Cranio-cervical injury
Cranio-cervical injuries include occipital condyle fractures and occipital cervical disassociation. Occipital condyle fractures are secondary to head impaction and are usually associated with traumatic brain injury and/or cranial nerve (CN) injury especially CN VI, VII, IX, XI and XII.19
Occipital condyle fractures are classified based on morphology.19 However, the stability is determined by the status of the alar ligaments. The alar ligaments extend from the lateral tip of the dens to the anterior medial aspect of the occipital condyle and are essential for cranio-cervical stability. Just lateral to this is the hypoglossal neuroforamen containing the CN XII which explains the higher incidence of this CN palsy in association with cranio-cervical injuries.
The type I occipital condyle fractures are comminuted fractures of the occipital condyle and are generally stable. Type II is the extension of a basilar skull fracture to involve the occipital condyle. Rarely, the entire occipital condyle is displaced resulting in an unstable fracture. Type III are avulsion fractures at the attachment of the alar ligaments. These are stable if the occipital C1 articulations are congruous and non-displaced. If displaced, then patients have cranio-cervical disassociation, which is present in about one-third of type III cases. Bilateral type III fractures have significant potential for instability.
Cranio-cervical disassociation is injury to the alar ligament, tectorial membrane and bony attachments so that the cranium is separated from the upper cervical spine. Other terms used are cranio-cervical instability and atlanto-axial instability. In geriatric patients cranio-cervical disassociation is rare and when associated with neurologic injury is usually fatal. The classification of cranial cervical disassociation is now functionally based on severity of injury.20 Type I are injuries where alignment on CT between the occipital condyle C1 lateral masses is normal but on MRI abnormal edema is present in the alar ligaments and tectorial membrane. Type II injuries have normal CT alignment, but displace under a diagnostic trial of traction. Type III are displaced between the occiput condyles in C1 greater than 2 mm.
Atlanto-axial injury
The atlanto-axial spine is highly mobile accounting for 50% of axial rotation and 10–15 degrees of flexion-extension. It is the most common location of injury in geriatric patients. The most common mechanisms are falls from standing height where the patient strikes the face or cranium. This produces hyperextension forces in the upper cervical spine. The hyperextension force may cause impingement between the occiput and C1–C2 spinal process and result in C1 posterior arch fracture. If the impact is more cranial, then axial directed forces are created which can cause a comminuted atlas fracture or so-called ‘Jefferson’s fracture’. Further, in hyperextension the anterior arch of C1 impinges on the dens which can cause an odontoid fracture. These may be predisposed by erosive changes secondary to degenerative changes which are common in approximately 50% of geriatric odontoid fractures. Many odontoid fractures in geriatric patients are actually acute injuries superimposed on chronic insufficiency fractures.14,21 These are associated with neurologic injuries in about 30% of patients.22 From similar mechanisms, forces may be directed more posteriorly, causing fracture in the posterior body or in the posterior elements of C2. These are referred to as hangman’s fractures or traumatic spondylolisthesis of the axis. Comminuted fractures, especially in the C1/C2 lateral masses and C2 body, are much more common than in younger patients.
ATLAS INJURIES
Atlas injuries are classified by location, including anterior and posterior arch fractures, bursting fractures (Jefferson) and lateral mass fractures. In the latter two patterns, stability is determined by the status of the transverse ligament which connects the two lateral masses behind the dens. When disrupted, the lateral masses can be unstable relative to each other and displace laterally over time. This is present when greater than 7 mm of combined displacement of the C1 lateral mass relative to C2 is seen on coronal CT or open mouth radiographs.
AXIS FRACTURES
The axis is the most common cervical vertebra injured in geriatric patients.3 The most common mechanism of injury is forced hyperextension usually from ground level falls. The patterns of axis injuries include odontoid fractures, traumatic spondylolisthesis of the axis and axis body fractures.
Odontoid fractures are classically classified by Anderson and D’Alonzo.23 Type I are avulsion fractures from the alar ligaments attachment at the tip of the dens. Unless associated with cranio-cervical injuries, these are stable. Type II are fractures to the waist of the dens and in general have a poorer prognosis (Figure 30.3). Type III are fractures of the dens extending into the C2 vertebral body (Figure 30.4). Grauer et al. further refined the classification of the type II fracture into a non-displaced, oblique pattern which is favourable for screw fixation, that is, the obliquity goes from anterior superior to inferior to posterior inferior, and type III which is unfavourable for screw fixation with the opposite oblique pattern or comminution of the C2 body.24
Traumatic spondylolisthesis of the axis represents a continuum of injury. Initially, bending forces create a fracture in the pars interarticularis or pedicle or even posterior body of C2. Further loading causes a C2–3 disco-ligamentous injury. The fractures can be non-displaced or displaced with subluxation or translation through the C2–3 disc space. A rare, but more severe, injury is the traumatic spondylolisthesis associated with C2–3 facet dislocation. Atypical fractures are more common in the elderly where the fracture extends more anteriorly into the vertebral body rather than the pars. Also, fractures may occur at different locations on each side, but in all cases there is separation of the posterior elements from the C2 body (Figure 30.5).
A more common injury in geriatric patients is C2 body fractures which are often comminuted. Benzel proposed three types but each have many variations. Type I are coronal-oriented vertical fractures. A type II is a sagittal-oriented vertical fracture. A type III fracture is a horizontally-oriented low transverse body fracture. In many cases, the fracture patterns will extend into the lateral masses and across the body of the vertebra (Figure 30.6).
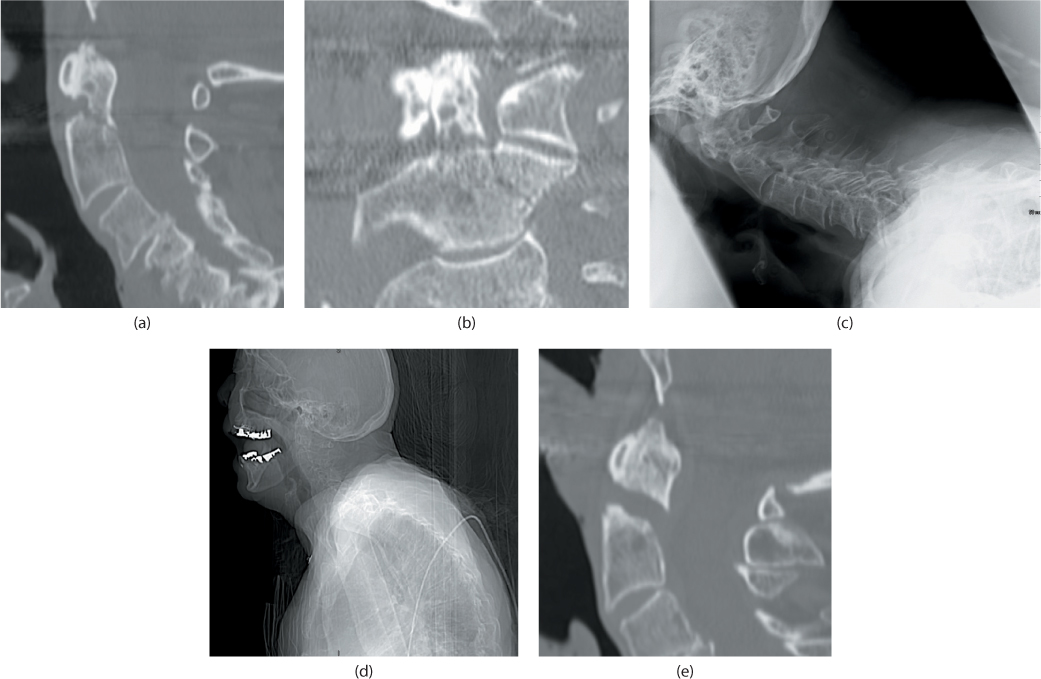
Figure 30.3 (a) Sagittal CT scan demonstrating an insufficiency fracture through the dens waist in 88-year-old man who had a ground level fall. Note erosions at the odontoid base which predispose to fracture. (b) Coronal reconstruction demonstrating erosive disease around the dens. A fracture through the dens waist and a left-sided C2 lateral mass fracture. (c) Upright radiograph taken in brace. Notice the patient’s difficulty holding his head up and he has progressively increased sagittal plane imbalance with his cervical spine alignment almost perpendicular to the weight-bearing axis. This increases shear forces making displacement more likely. (d) A scout film from CT scan shows this patient having severe spinal imbalance. Note the anterior translation of his head and neck due to thoracic and lumbar kyphosis. (e) At 12 months, the patient has a clear non-union as seen in the sagittal CT scan. He had minimal symptoms and was treated non-operatively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








