18
Cervical Root Compression
Bradley M. Thomas, John M. Olsewski, and Jerry G. Kaplan
History and Clinical Presentation
A 49-year-old right hand dominant electrician presented with complaints of progressive weakness in his right arm. He also described having pain in his neck extending down the front of his arm to his hand. He was having difficulty lifting objects with his right hand and performing repetitive-type motions, with weakness of his right shoulder and biceps. He reported occasional numbness in his thumb and index finger while at work.
He did not recall any trauma to his neck or arm. He denied bowel or bladder dysfunction, and was not experiencing disturbances in his gait. On further questioning he denied any history of smoking, diabetes, or hypertension. He also denied night pain.
PEARLS
- Spurling’s maneuver reproduces a patient’s arm pain and paresthesias by turning the patient’s head toward the symptomatic side and extending the neck. This position decreases the size of the neuroforamina.
- Use an EMG to differentiate first-degree shoulder problems from a C5 root problem.
- Biceps weakness may be the first sign of rotator cuff disease, although a herniated C6 root can give similar findings.
PITFALLS
- Patients with sensory changes in the thumb and index finger may have carpal tunnel syndrome and not a C6 radiculopathy.
- Check for a local Tinel’s and Phalen’s sign.
- An incomplete cervical spine exam in a patient with upper extremity problems often leads to an incorrect diagnosis.
- A full cervical spine x-ray series should be used to see on oblique films encroachment on the foramina by osteophytes.
Physical Examination
Examination revealed a patient in no acute distress, with a full range of motion of the cervical spine. Reproduction of his right arm pain was elicited with extension of the neck and rotation of his head to the right (Spurling’s maneuver). He appeared to have mild deltoid wasting on his right with prominence of his acromion. Motor testing was symmetric with 5/5 strength in bilateral deltoids, biceps, triceps, wrist flexors, wrist extensors, finger flexors, finger extensors, and hand intrinsics. His deep tendon reflexes were 2+ and symmetric, with the exception of the biceps reflex, which was depressed on the right side compared with the left. He had a negative Hoffman’s sign and his gait was within normal limits. Tinel’s and Phalen’s testing of the median nerve at the wrist were not provocative.
Diagnostic Studies
Radiographs taken included an anteroposterior, lateral, obliques, and flexion/extension laterals of the cervical spine. There is evidence of multilevel degenerative changes, with principal changes at the C5-C6 level. These changes include loss of C5–6 disk height on the lateral and narrowing of the C6 neural foramen with encroachment on the foramina by osteophyte on the oblique views (Fig. 18–1). Magnetic resonance imaging (MRI) of the cervical spine showed evidence of multilevel mild cord impingement with disk herniation at C3–4, C4–5, C5–6, and C6–7, along with focal increased signal intensity within the cord at the C5–6 level on the T2-weighted images consistent with cord edema (Fig. 18–2). There is also bilateral foraminal narrowing on the axial images at the C5–6 level (not shown). A needle electromyogram (EMG) was performed, which showed membrane instability of the C6 innervated muscles on the right side. C5, C7, and C8 muscles were normal. The nerve conduction studies did not exhibit peripheral nerve slowing as evidence for peripheral nerve compression.
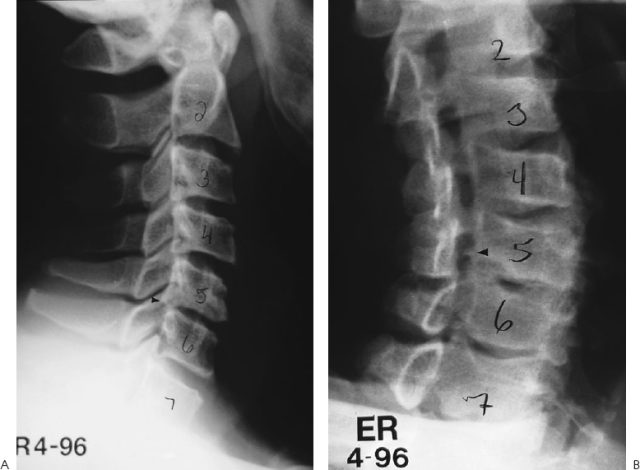
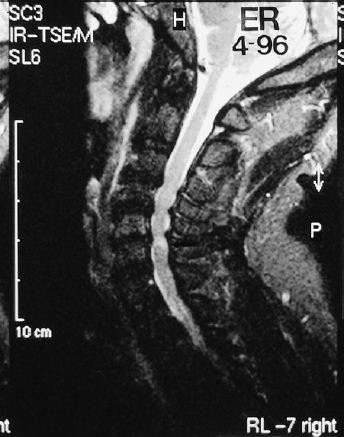
Figure 18–2. T2-weighted sagittal magnetic resonance imaging (MRI) of the cervical spine shows disk herniations at C3 lumen 4, C4–5, C5–6, and C6–7, along with focal increased signal intensity within the cord at the C5–6 level on the images consistent with cord edema.
Differential Diagnosis
Carpal tunnel syndrome
Rotator cuff tear
C5 radiculopathy
C6 radiculopathy
Brachial neuritis
Thoracic outlet syndrome
Diagnosis
C6 Radiculopathy
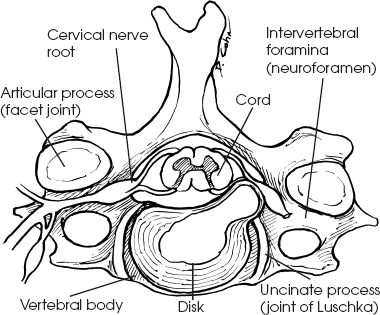
Cervical radiculopathy represents impingement of an exiting cervical nerve root generally caused by herniated disk material or from degenerative cervical spondylosis, or commonly a combination of the two. In cases where the etiology is a herniated disk, the symptoms are more acute in onset and may be exacerbated by coughing or other Valsalva-type maneuvers. Cervical spondylosis as a cause for radiculopathy has an insidious onset, with degenerative changes occurring at the disk and the zygapophyseal and neurocentral joints (Fig. 18–3). Other causes of cervical root irritation or compression include intraspinal tumors, infection, inflammatory arthritic changes, and chemical irritation from neurohumeral factors.
The presentation of cervical radiculopathy begins with varying degrees of pain, paresthesias, and motor weakness in the neck and upper extremity. Significant neck pain is often associated with the radicular pain and sensory changes, which generally follow a dermatomal distribution. Breast pain and angina-like symptoms should also be considered as potential radicular complaints. Weakness and reflex changes are also root specific, but significant overlap exists in the muscular innervation of the upper extremity and may occasionally be confusing. Table 18–1 outlines the clinical symptoms and findings seen with individual root involvement, and other potential causes for similar findings.