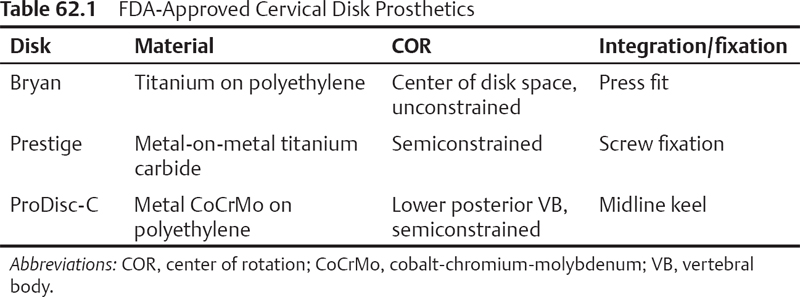
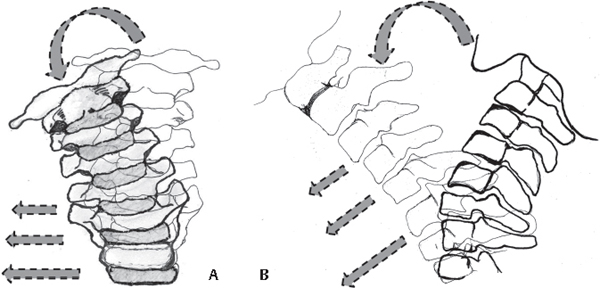
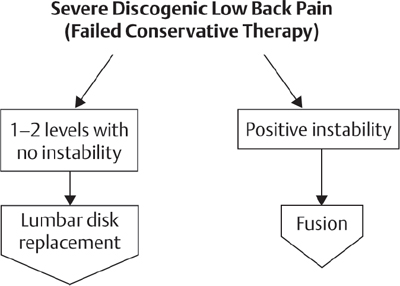
62 Despite the high success rate and long-term track record of anterior cervical decompression and fusion (ACDF) for treating degenerative cervical conditions,1 concerns persist regarding the increased biomechanical stresses at the adjacent segments.2 These concerns have resulted in interest in motion-sparing alternatives. Cervical disk arthroplasty (CDA) attempts to replicate the native disk’s kinematics, decreasing stress on adjacent vertebral levels and reducing adjacent-segment degeneration. The main theoretical advantages of disk arthroplasty are maintaining range of motion and avoiding adjacent-segment degeneration by restoring disk height and spinal alignment, and thereby the cervical spine’s biomechanical characteristics. Other benefits include less surgical morbidity compared with fusion bone grafting, lack of pseudarthrosis as a complication, native avoidance of complications from instrumentation or immobilization, and early return to function. Prostheses are classified as unconstrained, semiconstrained, or constrained (Table 62.1) based on the allowed motion relative to normal coupled motion (Fig. 62.1A,B).3 Unconstrained, or physiologic, designs do not constrain the center of rotation (COR) to a fixed point so that the locus of points that define the normal COR can be replicated. They simulate the six native degrees of freedom of movement. Most4 have a mobile polymer COR with a compressible nucleus and allow unconstrained resistance to angular motion. Semiconstrained prostheses have a mobile COR as in a ball-in-trough joint that allows five degrees of freedom of movement—three angular motions and two translations (usually in the sagittal and coronal planes)—but no compressibility. Constrained designs, with a fixed COR, have a ball-and-socket or saddle-type joint articulation and allow three angular degrees of freedom of movement without translation.5 There is no clear consensus on which design accomplishes the best results. Fig. 62.1 Artist’s sketches of coupled cervical motion (A) in the coronal plane, showing lateral bending of the vertebral body coupled with translation to the side, and (B) in the sagittal plane, showing rotation in the upper cervical spine and translation of the lower cervical vertebrae. CDA is approved by the Food and Drug Administration (FDA) for the treatment of single-level symptomatic degenerative disk disease with evidence of disk herniation between C3 and C7 causing radiculopathy and/or or myeloplathy.6–8 Contraindications to CDA include multilevel disease, cervical instability (defined as translation of > 3 mm and/or > 11 degrees of rotational difference to that of either adjacent level), post-traumatic vertebral body deficiency/deformity, and severe spondylosis (bridging osteophytes, disk height loss of 50%, and absence of motion). CDA is not an option for neck or arm pain of unknown cause or axial neck pain as the sole presenting symptom. Known allergy to implant materials (titanium, polyethylene, cobalt, chromium, molybdenum) and active local/systemic infection are absolute contraindications to CDA. General contraindications include severe osteoporosis/osteopenia; active malignancy or systemic disease, such as acquired immune deficiency syndrome (AIDS), human immunodeficiency virus (HIV), hepatitis B, hepatitis C, or type I diabetes; metabolic bone diseases or autoimmune spondylarthropathies (rheumatoid arthritis); morbid obesity (body mass index of 40); or pregnancy or trying to become pregnant in the next 3 years. The role of CDA in the treatment of adjacent-segment disease is still controversial.9 Fusion adjacent to the level and previous surgery at the level to be treated are contraindications. An aggressive discectomy with complete removal of all osteophytes, especially of the uncovertebral joint, is performed. As intervertebral motion is preserved, it is necessary to avoid potential dynamic compression in the foramen, which is not a consideration with ACDF. In a study of retrieved prostheses, the most frequent cause of revision was inadequate decompression and recurrence of symptoms.10 The posterior longitudinal ligament (PLL) is removed to ensure complete decompression, facilitate parallel distraction, restore intervertebral height, and mobilize the motion segment. Although the cartilaginous endplate is removed for CDA, the bony endplate is preserved to minimize the risk of implant subsidence. To facilitate the even insertion of the device and to allow appropriate surface contact between the endplates and the device, the vertebral endplates should be burred until there are two parallel surfaces. Over-resection of the posterior vertebral body can lead to loss of contact posteriorly and subsequent retropulsion. Avoiding kyphosis is vital to the restoration of normal cervical biomechanics. Yi et al.5 found that disk insertion angle and insertion depth were significantly correlated with postoperative sagittal imbalance. Centralization of the prosthesis is important to the success of a cervical total disk arthroplasty. Proper midline identification and placement of the device are critical; in contrast, a graft for ACDF can be placed eccentrically. For CDA, careful fluoroscopic evaluation in the anteroposterior and lateral planes to ensure proper visualization of the disk space in the lateral view is crucial.4 If body habitus precludes clear visualization of the interspace, fusion should be strongly considered. Overdistraction of the interbody space should be avoided because it may lead to nerve root stretch, facet joint overload, and loss of motion. The highly predictable and favorable outcome of ACDF in cervical disease has always posed a strong argument against the need for CDA.2 For the past two decades, many spine surgeons have compared the efficacy and safety of CDA and fusion. A recent systematic literature review11 reported on 13 case series presenting clinical data on the effectiveness of CDA (single- and multiple-level), four randomized controlled trials comparing single-level fusion to arthroplasty, and one nonrandomized comparative study.6–8,12,13 Three randomized controlled trials represented FDA-regulated investigational device exemption (IDE) studies that evaluated the safety and effectiveness of the Prestige ST Cervical Disk System (Medtronic, Memphis, TN),13 Bryan Disk (Medtronic Sofamor Danek, Memphis, TN),6 and ProDisc-C (Synthes Spine, West Chester, PA).7 The Prestige System study concluded that it maintained physiologic segmental motion at 24 months after implantation and provided improved neurologic success, improved clinical outcomes, and a reduced rate of secondary surgeries compared with ACDF.13 The Bryan disk study showed there was no statistical difference between the ACDF and CDA groups with regard to the rate of secondary surgical procedures performed.6 Patients who received the artificial cervical disk returned to work nearly 2 weeks earlier than did those in the ACDF group.6 The ProDisc-C study showed no difference in visual analog scale scores for neck and arm pain between the CDA and ACDF groups, but ProDisc-C patients achieved equal to or greater than 4 degrees of motion or maintained motion relative to preoperative baseline at the operated level.7 There was a statistically significant difference in the number of secondary surgeries, with 8.5% of ACDF patients needing a reoperation, revision, or supplemental fixation within the 24-month postoperative period compared with 1.8% of ProDisc-C patients.7 In summary, there was level I evidence of significant improvement on the Neck Disability Index and neck and arm pain visual analog scale scores for the CDA and ACDF groups, similar mean angular motion values before and after surgery for the CDA group, faster return to work for the CDA group, and lower reoperation rates for the patients in the CDA group. Complications of the anterior approach to the cervical spine include dysphagia, hoarseness, and unilateral vocal fold paralysis, which are not specific to arthroplasty.12,14 Of more than 5500 Bryan cervical disks implanted worldwide, 11 are known to have been explanted, with four revised because of infection.10 Three of the ~ 300 implanted Prestige disks were retrieved, with one disk revised because of infection.10 Extrusion, retropulsion, and subsidence are well-known complications of CDA. Wear is affected by the type of material, duration of exposure to debris, prosthetic load and kinematics, specific joint, lubrication, host responsiveness, and particle size, shape, and concentration. The nature of fibrocartilaginous joints may mean that there is a less inflammatory response in the cervical spine than in relatively proinflammatory synovial joints. Accelerated wear and particle debris formation leading to device loosening do not appear to be an issue.10 Motion preservation after CDA is guaranteed only if spontaneous fusion can be prevented. According to McAfee et al.,15 heterotopic ossification (HO) after CDA can be classified as grades 0 to 4. Reports of HO are variable among different prostheses, ranging from 21% to 71.4%.16 One study reported 49.4% of the patients with grade 2 to 3 ossification after 1 year.17 Early HO after arthroplasty can potentially be avoided by administering nonsteroidal anti-inflammatory drugs (NSAIDs) in the immediate postoperative period.18 CDA is a reasonable alternative to ACDF for one-level disease in patients with soft disk herniations and minimal bony degenerative changes. Complete discectomy and osteophyte removal, preservation of the bony endplate, and proper positioning and sizing of the implant are critical for preservation of motion. The indications and contraindications of the procedure are currently evolving with wider use and longer patient follow-up. 1. Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 2002; 50(2):229–236, discussion 236–238 PubMed 2. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 1999;81(4):519–528 PubMed 3. Kang H, Park P, La Marca F, Hollister SJ, Lin CY. Analysis of load sharing on uncovertebral and facet joints at the C5-6 level with implantation of the Bryan, Prestige LP, or ProDiscC cervical disc prosthesis: an in vivo image-based finite element study. Neurosurg Focus 2010;28(6):E9 PubMed 4. Kouyoumdjian P, Bronsard N, Vital JM, Gille O. Centering of cervical disc replacements: usefulness of intraoperative anteroposterior fluoroscopic guidance to center cervical disc replacements: study on 20 Discocerv (Scient’X prosthesis). Spine 2009;34(15):1572–1577 PubMed 5. Yi S, Shin HC, Kim KN, Park HK, Jang IT, Yoon H. Modified techniques to prevent sagittal imbalance after cervical arthroplasty. Spine 2007;32(18):1986–1991 PubMed 6. Heller JG, Sasso RC, Papadopoulos SM, et al. Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine 2009;34(2):101–107 PubMed 7. Murrey D, Janssen M, Delamarter R, et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J 2009;9(4):275–286 PubMed 8. Nabhan A, Ahlhelm F, Pitzen T, et al. Disc replacement using Pro-Disc C versus fusion: a prospective randomised and controlled radiographic and clinical study. Eur Spine J 2007; 16(3):423–430 PubMed 9. Jawahar A, Cavanaugh DA, Kerr EJ III, Birdsong EM, Nunley PD. Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in cervical spine: results of 93 patients in three prospective randomized clinical trials. Spine J 2010;10(12):1043–1048 PubMed 10. Anderson PA, Rouleau JP, Toth JM, Riew KD. A comparison of simulator-tested and -retrieved cervical disc prostheses. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine 2004;1(2):202–210 PubMed 13. Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine 2007;6(3):198–209 PubMed 14. Campbell PG, Yadla S, Malone J, et al. Early complications related to approach in cervical spine surgery: single-center prospective study. World Neurosurg 2010;74(2-3):363–368 PubMed 15. McAfee PC, Cunningham BW, Devine J, Williams E, Yu-Yahiro J. Classification of heterotopic ossification (HO) in artificial disk replacement. J Spinal Disord Tech 2003;16(4):384–389 PubMed 16. Yi S, Kim KN, Yang MS, et al. Difference in occurrence of heterotopic ossification according to pros-thesis type in the cervical artificial disc replacement. Spine 2010;35(16):1556–1561 PubMed 17. Mehren C, Suchomel P, Grochulla F, et al. Heterotopic ossification in total cervical artificial disc replacement. Spine 2006;31(24):2802–2806 PubMed 18. Bryan VE Jr. Cervical motion segment replacement. Eur Spine J 2002;11(Suppl 2): S92–S97 PubMed Cavanaugh DA, Nunley PD, Kerr EJ III, Werner DJ, Jawahar A. Delayed hyper-reactivity to metal ions after cervical disc arthroplasty: a case report and literature review. Spine 2009;34(7): E262–E265 PubMed The authors present a case of a woman who, after initially doing well after undergoing a CDA, developed recurrence of her symptoms. Revision surgery revealed inflammatory tissue thought to be related to metal ions and similar to the tissue seen in metal-on-metal total hip arthroplasties. This represents a rare complication, but one of which surgeons should be aware. Chen J, Wang X, Bai W, Shen X, Yuan W. Prevalence of heterotopic ossification after cervical total disc arthroplasty: a meta-analysis. Eur Spine J 2011 PubMed The authors performed a meta-analysis to determine the incidence of HO after CDA. They found the prevalence of HO to be 44.6% at 1 year and 58.2% at 2 years. The prevalence of severe HO was 11.1% and 16.7% at 1 and 2 years, respectively. The clinical significance of HO has not been established. Garrido BJ, Wilhite J, Nakano M, et al. Adjacent-level cervical ossification after Bryan cervical disc arthroplasty compared with anterior cervical discectomy and fusion. J Bone Joint Surg Am 2011;93(13):1185–1189 PubMed The authors compared 21 patients who had undergone CDA to 25 patients who had ACDF. The ACDF group showed significantly higher rates of adjacent-segment ossification at both 2 and 4 years. McAfee PC, Cappuccino A, Cunningham BW, et al. Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech 2010;23(1):1–8 PubMed The authors evaluated the incidence of dysphagia among 251 patients randomized to ACDF or CDA. CDA resulted in significantly lower rates of dysphagia at 3 and 12 months postoperatively. Upadhyaya CD, Wu JC, Trost G, et al. Analysis of the three United States Food and Drug Administration investigational device exemption cervical arthroplasty trials. J Neurosurg Spine 2011 PubMed The authors performed meta-analysis of the three IDE trials comparing CDA with ACDF, with 2-year follow up. They concluded that both techniques resulted in excellent neurological improvement but that there was a higher rate of revision surgery following ACDF. There was a trend toward lower rates of adjacent-segment disease at 2 years with arthroplasty. It should be noted that all of these studies are industry sponsored.
Cervical Intervertebral Disk Arthroplasty
![]() Prosthetic Designs
Prosthetic Designs
![]() Indications and Contraindications for CDA
Indications and Contraindications for CDA
![]() Technical Considerations
Technical Considerations
![]() Outcome
Outcome
![]() Complications
Complications
Approach-Related
Specific to Arthroplasty
Infection
Prosthesis Migration
Wear
Heterotopic Ossification
![]() Conclusion
Conclusion
References
Suggested Readings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






