Cemented Femoral Revision in Total Hip Arthroplasty
A View in the 21st Century
Bryan Nestor
Key Points
Introduction
Cemented femoral revision has fallen out of popularity as uncemented revision methods have matured. Cemented femoral revision with impaction bone grafting is a special technique that is discussed later. Cemented femoral revision now is used mostly in elderly patients with low activity demands and good remaining cancellous bone, which provides for cement interdigitation with the bone and hence a good mechanical interlock (Fig. 94-1). Cemented revision is also used in special cases in which the old cement mantle is intact and is well bonded to the bone, allowing a “cement-in-cement” technique after removal of the previous prosthesis from the cement.
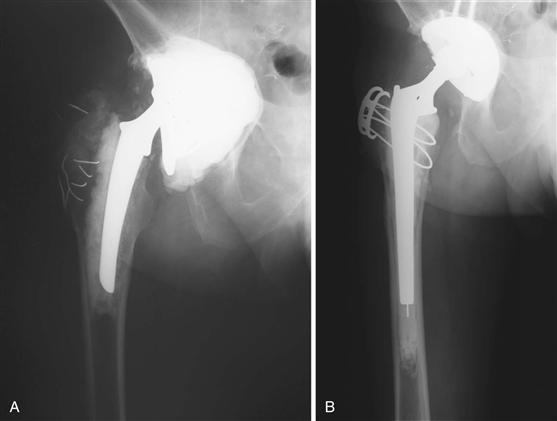
Figure 94-1 A, Hip radiograph of patient with loose femoral stem and good remaining cancellous bone. B, Radiograph after revision with cemented calcar replacement femoral component. Note that the good cancellous bone allowed creation of a good bone-cement interface.
Early Experience
Not long after the introduction of cemented total hip arthroplasty, aseptic loosening was recognized as the major cause of failure. Early experience with cemented revisions led most to observe that the results of revision would be less satisfactory than those attained with primary total hip arthroplasty.1–3 Even by the end of the first decade of total hip arthroplasty in the late 1970s, it was recognized that the best opportunity to attain good long-term fixation was the “first time around,” and that most early failures would have been done differently based on recognized technical advances.3
In one of the earliest reports of cemented revision total hip arthroplasty by Hunter and associates, only one fourth of patients had a good or excellent result with early follow-up, and results were confounded by the presence of infection. Ultimately, one third of patients were diagnosed with infection, and Girdlestone resection was the final treatment for 31 of 140 revision hip arthroplasties.2 Amstutz and colleagues reported on 88 patients, of whom 73% underwent cemented femoral revision, and outlined the significant complexity of revision hip arthroplasty with increased blood loss, increased operative time, and increased complications compared with primary hip arthroplasty.1 Even more disappointing was the 9% incidence of re-revision at short-term follow-up, with an additional 20% showing substantial progressive radiolucencies.1 Kavanagh and coworkers reviewed 206 hip revisions and reported a mechanical failure rate of 18% and a re-revision rate of 8%.4 Pellicci and associates reported similar results for 110 hips in 107 patients with a mechanical failure rate of 14% and progressive radiolucencies in 26%.3 However, with longer follow-up, this same series of patients had a 29% failure rate.5 Marti and associates reported 85% survival of cemented revisions at 14 years using early techniques from 1974 to 1983.6
Numerous studies subsequently documented the high incidence of re-revision, mechanical loosening, and radiographic radiolucencies with early cemented femoral revision techniques and long-term follow-up.7–11 Correlating with the high rate of radiographic radiolucencies, the use of roentgen stereophotogrammetric analysis confirmed a very high rate and extent of femoral component migration following cemented revision, particularly in cases with severe bone loss.12,13
Lessons Learned
As the experience with cemented femoral revision grew, a number of lessons learned from the initial experience contributed to improved clinical results.
Lesson 1: Longer stems can improve cemented femoral fixation
One of the early observations pointed out the advantage of using longer stems that bypassed proximal bone deficiencies and attained fixation in better quality bone distally. Progression of radiolucencies was observed by Callaghan and associates to be significantly less in femoral revisions performed with long-stem prostheses (150 to 230 cm in length).14 Similarly, using early cement techniques, Turner and colleagues reported decreased progression of femoral radiolucencies and decreased mechanical failure with use of long-stem implants.15 Crawford and coworkers, using a long stem in a series of 74 femoral revisions performed after 1985, most of which had severe bone loss, found no mechanical failures at a mean follow-up of 5.75 years in 45 hips in which the stem had at least 10 cm of distal fixation.16 Others using contemporary cement techniques have shown a decreased risk of re-revision when a long-stem femoral component is used.17,18 Repten and colleagues demonstrated improved survival when the stem extended beyond the most distal extent of bone loss by at least one diameter.18 Hultmark demonstrated that long-stem fixation had a 93% survival rate free of mechanical loosening compared with a 79% survival rate for standard stems at 10 years.17 In a biomechanical study using a three-dimensional finite element model, Mann and coworkers showed that a femoral component that bypassed the cancellous bone defect by two femoral diameters was most effective in reducing adverse stresses in the cement mantel and motion and stresses at the cement-bone interface.19 Further increases in stem length had only a minor effect.19
Lesson 2: Cemented re-revision does poorly
Another early observation was that cemented re-revisions resulted in even less satisfactory clinical and radiographic results than index cemented femoral revisions with a high rate of subsequent mechanical failure.15,20,21 The poorer results were felt to be secondary to progressive loss of the micro-interlock between cement and cancellous bone. In a biomechanical study, Dohmae and associates demonstrated that bone-cement interface shear strength was reduced to 20.6% of primary strength with the first revision and to 6.8% of primary strength with the second revision.22
Lesson 3: Bone loss and time to failure are risk factors for failure
A number of studies have demonstrated a correlation between the prognosis for cemented femoral revision and the degree of bone loss.17,22,23 This is reflected by the difficulty of obtaining a good cement mantle as defined by Mulroy and Harris.17,24 Davis and colleagues in a study on 48 cemented femoral revisions for failed uncemented femoral components reported a loosening rate of 29% with minimum 5-year follow-up.25 The high rate of failure was likely secondary to extensive loss of cancellous bone and to the use of standard length stems in most cases (41/48).25 Perhaps directly or indirectly related to bone quality, Malchau and coworkers, reporting the results of 16,577 cemented femoral revisions in the Swedish Registry, with and without impaction grafting, noted a 3.3 times increased risk of re-revision when the first revision was performed within 5 years of the index arthroplasty.26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








