FIGURE 22-1. A: Hip radiograph of elderly patient with failed loose uncemented press-fit hemiarthroplasty. Note the good remaining cancellous bone and large canal diameter. B: Hip radiograph after revision with cemented femoral component. Note the good bone-cement interface.
Other circumstances may favor cemented fixation of a revision stem, particularly if previous radiation, metabolic bone disorders, or chronic exposure to bone inhibiting substances are suspected of contributing to ingrowth failure of an uncemented primary implant. Abnormal femoral geometry that precludes the use of uncemented components may call for a cemented revision (Fig. 22-2), as might a history of unexplained thigh pain in an otherwise well-fixed uncemented stem. Finally, in patients undergoing revision for infection, cemented techniques may be selected for additional antibiotic delivery; however, this should not take precedence over achieving stable fixation in situations where an inadequate cancellous bed exists.
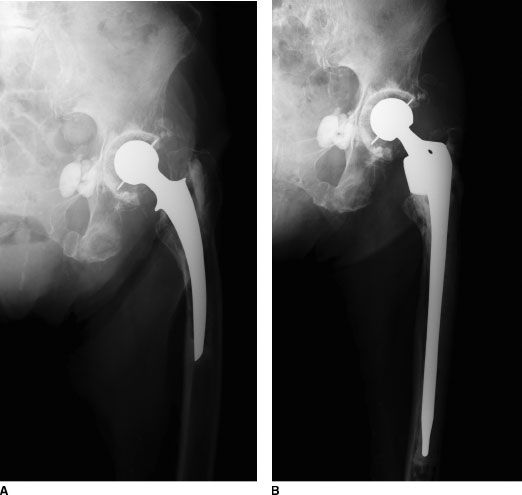
FIGURE 22-2. A: Hip radiograph of elderly patient with loose stem, large diameter femoral canal, poor cortical bone quality, and femoral deformity. B: Radiographs after revision with calcar replacing long-stem femoral component.
Conventional cemented femoral revision now is used in North America mainly in older, relatively low-demand patients in whom certain specific circumstances are present; these include an intact cortical tube of bone, remaining cancellous bone in the intramedullary canal to provide for cement interdigitation, a very large femoral canal diameter, and situations in which antibiotic-loaded cement provides a definite advantage. Circumstances that favor an uncemented femoral component, even in an older individual, include good cortical bone strength and cases in which an extended greater trochanteric osteotomy will be beneficial for implant extraction. A good example of a candidate for cemented femoral revision might be an older patient with poor bone quality and a failed loose Austin Moore type hemiarthroplasty.
Cement-in-cement revision techniques should be employed when an existing bone-cement interface has stood the test of time and remains in a pristine condition (Fig. 22-3). Stems that have failed secondary to debonding between the implant and the cement mantle or secondary to implant fracture within an intact cement mantle are excellent candidates for this revision technique. Furthermore, in instances where a polished cemented stem needs to be removed for acetabular exposure, modification of version, or correction of a discrepant limb length (and this can be performed without damaging the existing cement mantle), a cement-in-cement technique can be utilized for stem replacement or reinsertion.
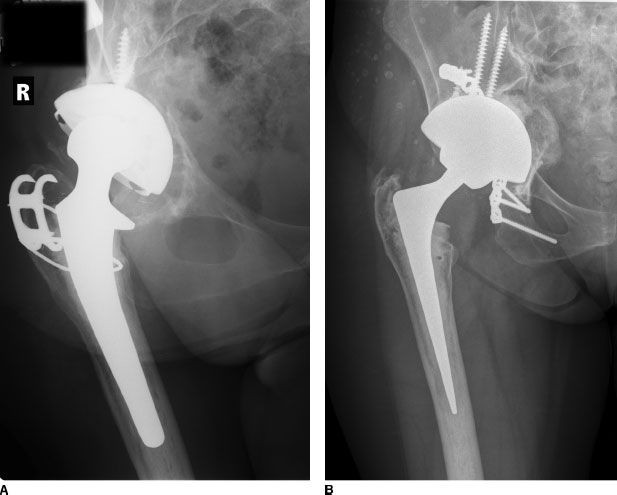
FIGURE 22-3. A: Hip radiograph of patient with loose cup and pelvic discontinuity. At operation, the stem was found to be debonded from the well-fixed cement mantle. B: Hip radiograph after acetabular revision and femoral revision using cement-in-cement technique. The old cement mantle was preserved, and a new modular stem with improved femoral offset and modular head was cemented into the previous cement mantle.
TECHNIQUE
Conventional Cemented Revision Before surgery, preoperative planning is performed to choose optimal implant size and length. If proximal bone is deficient, a calcar replacement design may be considered. Preoperative radiographs are scrutinized to identify the locations of any cement or sclerotic bone that will need to be removed to accommodate the new stem.
The hip is exposed through the surgeon’s preferred approach, and the previous cement mantle, if present is removed. Membrane within the femoral canal is removed meticulously with backbiting hand instruments. Any remaining membrane leads to an immediate radiolucent line on radiographs and complete lack of bone-cement bond in that area. Use of canal reaming is discouraged as this will remove remaining cancellous bone and macrostructure from the femoral canal, leading to a polished, smooth, round canal that provides little micro- or macrostructure for cement interdigitation. If a neocortex is present around the previous implant, as is commonly the case in a failed uncemented hemiarthroplasty and in some failed cemented implants, it is removed with power burrs and backbiting hand instruments. This step is important because it uncovers the underlying cancellous bone necessary for cement interdigitation. Areas of hard sclerotic bone may also be macrotextured with a power burr or hand instruments to improve cement fixation.
Usually little canal preparation with broaches is needed, but in some cases minimal broaching to properly shape the canal is helpful. Broaches should be used cautiously if the bone is sclerotic to avoid fracture.
Trial implants are placed, and trial reductions are performed. Usually radiographs are obtained with trial implants in place to assess implant alignment and length. The trial implants may not be rotationally stable in the femoral canal, which can reduce the information gained from trial reduction, but at a minimum the surgeon needs to ascertain if appropriate leg length restoration can be gained using the proposed implant.
A cement restrictor is placed at an appropriate depth in the femoral canal. If a standard-length stem is being used, a conventional off-the-shelf polyethylene plug usually works well. When a long-stem implant is being used that requires plug placement beyond the isthmus, sometimes an oversized off-the-shelf polyethylene plug will gain fixation. If not, a cement plug can be fashioned using a bolus of approximately 10 mL of cement delivered with a long, task-specific cement syringe. The canal is irrigated with pulsatile lavage and dried with suction followed by sponges soaked in dilute epinephrine solution, followed by dry sponges. Sponges are inserted so that a “tail” always protrudes from the canal to minimize risk that one will be left in place during cementation.
Cement is mixed under vacuum conditions. In almost all revision cases, the senior author prefers to add appropriate doses of antibiotic(s) to the cement. The cement is injected into the femoral canal, after dry sponge removal, using a cement gun. The cement is injected in retrograde manner and then pressurized with the gun using cone-shaped rubberized canal “pressurizers” to occlude the canal around the cement gun barrel. Next the real femoral implant is advanced gradually into the cement and seated at the appropriate level. The goal is to advance the implant into the cement late enough in the cement curing cycle that some resistance is felt, which indicates the cement is being further pressurized, but early enough in the cement cycle to make sure the implant can be fully seated without excessive force. Care must be taken during implant insertion to insure appropriate implant axial alignment and to insure appropriate rotational implant alignment, that is, anteversion. The implant is held securely until cement has fully hardened, and during this process excess cement is removed. Another trial reduction is then carried out, optimal modular head neck length is chosen, and then a real head is affixed to the implant.
Cement-in-Cement Before surgery, radiographs are carefully scrutinized to determine if the patient meets the narrow indications, noted above, for this technique. Templating is performed to choose implant size and to determine if a new implant will fit in the previous cement mantle.
After the surgical exposure of choice, the previous femoral implant is removed. The cement mantle is examined to make sure it is intact. A burr is used to freshen the interior of the accessible cement mantle. A trial implant is placed to see if it will fit in the old cement mantle. If not, space for a new implant may be created by judiciously expanding the internal size of the old cement mantle with a power burr, reamers, or ultrasonic instruments. Once trial reduction demonstrates that a new implant can be placed in adequate position, which adequately restores leg length, a new implant can be cemented in place. Before cementation, the canal of the cement mantle is carefully dried with sponges. Cement, in most cases loaded with an appropriate dose of antibiotics, is mixed under vacuum conditions and injected into the canal early in the cement curing cycle. More liquid cement can bond more effectively to the old cement mantle, which is an essential component for success of this technique. The new stem is then inserted slowly into place, optimizing implant axial and rotational alignment. After cement has hardened, trialing with modular heads and placement of the final chosen modular head is routine.
RESULTS
Cementation techniques have evolved greatly since their inception, and this progress has translated into improved results following cemented femoral revision. Reports in the literature must therefore be weighed based on the cementation techniques that were used to perform the revisions contained within those series. Toward this end, results are grouped into early or historical series, which employed first generation cementation techniques and more recent series, which employed second and third generation techniques. Furthermore, the role of specific factors including patient age, patterns of bone loss, cement mantle grade, and stem length need to be considered in isolation when analyzing the results of cemented revision to properly appreciate their impact on outcomes.
Early Results: First Generation First generation cementation techniques employing hand-mixed cement, minimal canal preparation, and manual cement insertion, without a distal cement plug, resulted in a high rate of early failure from aseptic loosening. Amstutz et al.12 reported a 4.3% rate of femoral loosening leading to revision and a 33% rate of overall femoral mechanical failure in a series of 66 hips revised with first generation cementation techniques at a mean follow-up of 2 years. Callaghan et al.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








