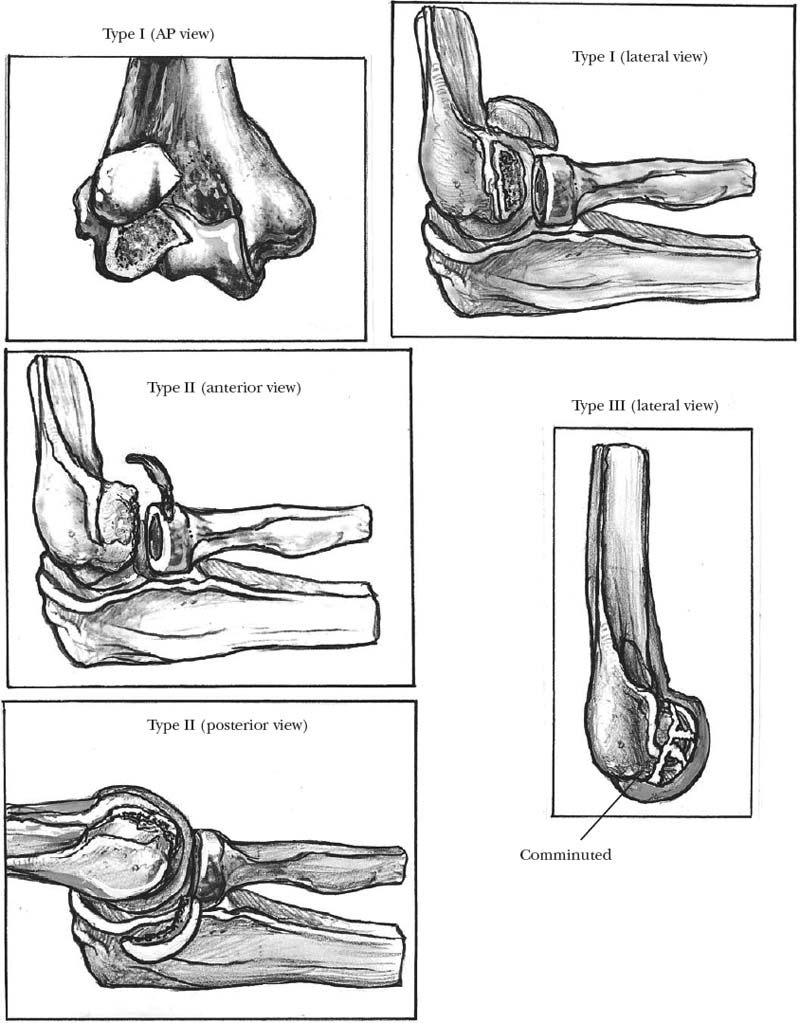
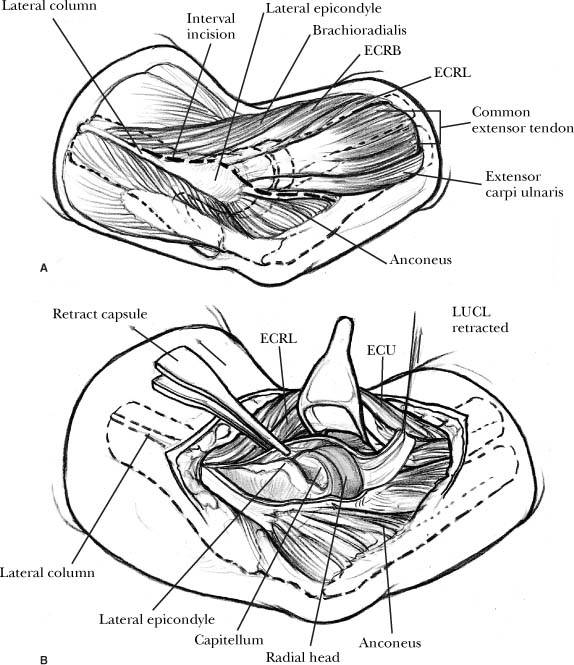
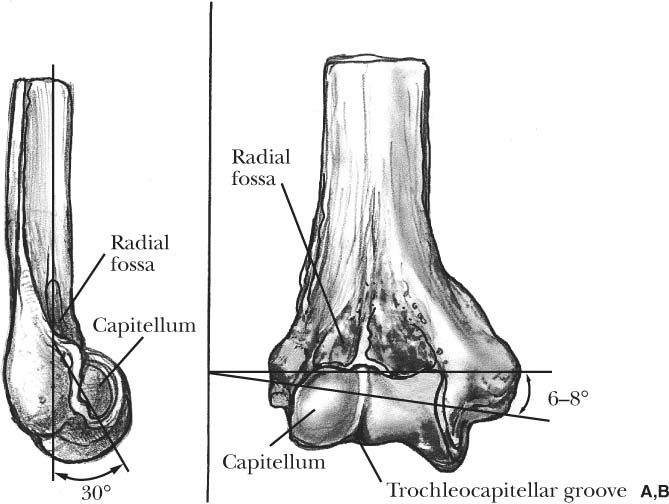
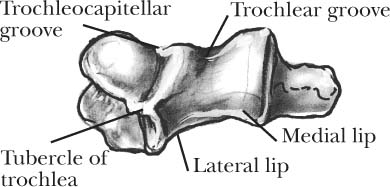
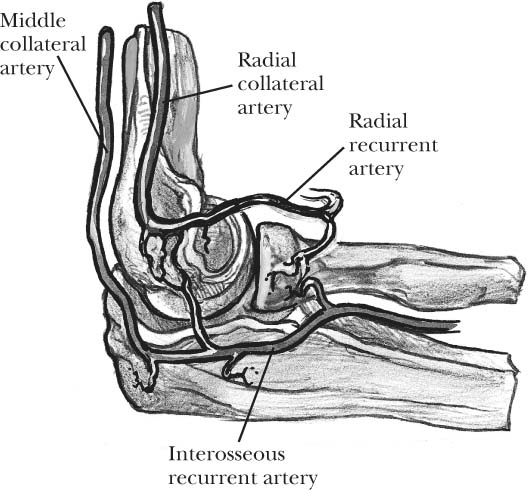
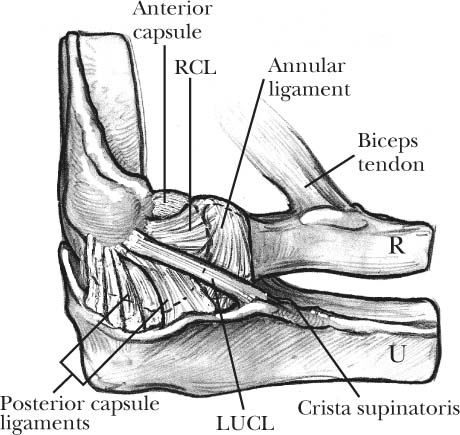
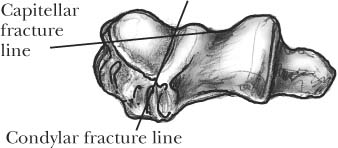
3 The capitellum represents the distal extension of the lateral column of the humerus. The spherical shape of the capitellum articulates with the concave radial head. The matching contour and intervening cartilage provide load transmission and proximal radioulnar joint stability. Maximum contact and load transference occur during forearm pronation and valgus stress.1 Fractures of the capitellum disrupt this pivotal articulation and interfere with normal lateral column function. The size of the fracture fragment and integrity of the surrounding articulations directly influence fracture management. This chapter will discuss various aspects of capitellum fractures and provide guidelines for surgical management. The capitellum (Latin for “little head”) is the first epi-physeal center of the elbow to ossify and represents the lateral extension of the distal humerus.2,3 The capitellum is directed in an anterior direction about 30 degrees with respect to the long axis of the humerus (Figure 3-1). The center of rotation about the capitellum is displaced 12 to 15 mm anterior to the humeral shaft axis and is collinear with the trochlear axis.4 The capitellum is nearly spherical in shape and lined with a 2 mm thick layer of articular cartilage along its anterior surface. The posterior aspect of the capitellum is devoid of articular cartilage.5 The lateral border merges with the lateral epicondyle. The radial fossa lies just above the capitellum, and the radial head approximates into this depression during full flexion. The radial head articulates with the anterior surface of the capitellum when the elbow is positioned in flexion. The contact area shifts to the inferior surface of the capitellum during elbow extension. The trochleocapitellar groove separates the capitellum from the trochlea and provides stability to the elbow3,6 (Figure 3-2). The radial head articulates with the groove throughout the arc of flexion and during forearm rotation.5 Extraosseous and intraosseous vessels generate the blood supply to the distal humerus. The intraosseous circulation is segmental to each particular area.7 The lateral arcade is formed by an anastomosis between the radial collateral, middle collateral, radial recurrent, and interosseous recurrent arteries (Figure 3-3). Posterior perforating vessels that stem from the lateral arcade supply the capitellum and the lateral aspect of the trochlea. These small osseous branches perforate the capitellum along its posterior aspect and provide its sole blood supply. The posterior perforating vessels should be preserved during fixation of capitellum fractures. Ligaments that are crucial to elbow stability cloak the lateral surface of the elbow. The lateral collateral ligament complex consists of the radial collateral ligament, the lateral ulnar collateral ligament, and the annular ligament8 (Figure 3-4). Any surgical approach to the lateral side of the elbow must respect these essential ligaments. Violation of only the anterior or posterior half of the lateral collateral ligament does not result in posterolateral instability of the elbow. In contrast, complete disruption results in debilitating posterolateral instability about the elbow.8 During a lateral surgical approach to capitellum fractures, the surgeon must be aware of the lateral collateral ligament complex.9 FIGURE 3-1. The capitellum is directed in an anterior direction about 30 degrees with respect to the long axis of the humerus. (A). Lateral view. (B). Anterior view. FIGURE 3-2. The trochleocapitellar groove separates the capitellum from the trochlea and provides stability to the elbow. FIGURE 3-3. Blood supply to the lateral column is provided by the lateral arcade formed by an anastomosis between the radial collateral, middle collateral, radial recurrent, and interosseous recurrent arteries. FIGURE 3-4. The lateral collateral ligament complex consists of the radial part of the lateral collateral ligament (RCL), the ulnar part of the lateral collateral ligament (LUCL), and the annular ligament. FIGURE 3-5. Lateral (A) and anteroposterior (B) x-rays of concomitant elbow dislocation and capitellum fracture. Similar to the radial head, the capitellum contributes to valgus stability of the elbow. In a cadaver, isolated excision of the capitellum produces a minimal increase in valgus motion.10 Concomitant release of the medial collateral ligament, however, yields considerable valgus instability. These biomechanical data suggest that excision of the capitellum has a negligible effect on valgus motion as long as the medial collateral ligament injury is intact. Concomitant loss of the capitellum and medial collateral ligament will result in progressive cubitus valgus deformity over time. Capitellum fractures are rare and account for about 0.5 to 1% of all elbow fractures.3,11 Capitellum fractures are more common in females, which may be secondary to an increased carrying angle or underlying osteoporosis.3,11–13 Cubitus recurvatum may also be a predisposing factor, as hyperextension subjects the protruding capitellar prominence to a shear force.14 Capitellum fractures occur primarily in individuals older than 12 years of age. In younger children, the lateral condyle or supracondylar area is more susceptible to injury.14–17 The mechanism of injury is a fall on an outstretched hand with axial compression, forearm rotation, and elbow flexion.2,10,12,18 This trauma produces an axial force in the radial head that shears the capitellum from the distal humerus with a variable amount of underlying bone. The force through the radial head explains the occasional association between fractures of both the capitellum and the radial head. Subtle differences in the amount of axial load, the position of forearm rotation, and the amount of elbow flexion generate variations in fracture pattern and fragment position.19 Additional mechanisms of injury have been proposed, including a direct force applied to the posterior aspect of the forearm with the elbow in flexion and a direct fall onto a flexed elbow.2–4,10,20,21 Capitellum fractures can occur in isolation or may be associated with a concomitant radial head fracture or elbow dislocation19,20–25 (Figure 3-5). Rupture of the medial collateral ligament can occur during injury and must be recognized to prevent progressive valgus instability after capitellum excision.26 Associated nerve and vascular injuries are rare. Capitellum fractures are coronal shear fractures of the distal humerus that disrupt the lateral column. The entire fracture is intra-articular and does not involve the epicondyle or metaphysis.21,27 The size, configuration, and amount of comminution may vary, although the fracture plane is similar. In contrast, lateral condyle fractures occur in the sagittal plane and include the lateral epicondyle and the metaphysis (Figure 3-6). FIGURE 3-6. Capitellum fractures occur in the coronal plane, and lateral condyle fractures occur in the sagittal plane. Capitellum fractures can be classified into four types, according to the size of the fracture fragment and extent of the fracture line (Table 3-1 and Figure 3-7). A type I (Hahn-Steinthal) fracture is a coronal fracture with a large fragment containing substantial subchondral bone (Figure 3-8). The fracture fragment may include the adjacent lip of the trochlea.10,25 A type I fracture is the most common pattern of capitellum fracture.2,10,28,29 A type II (Kocher-Lorenz or Mouchet) fracture is less common and represents a sleeve fracture with minimal bone. Only a shell of anterior cartilage is present with a thin layer of subchondral bone.2,10,11,30–32 Mouchet32 described this fracture as an “uncapping” of the capitellum. Type III is the least common capitellum fracture. The capitellum is either comminuted or compressed secondary to considerable axial load3,12 (Figure 3-9). The articular surface can be impacted into the humeral metaphysis. McKee et al20 described an additional type of isolated capitellum fracture (type IV) (Figure 3-10). This fracture propagates further medial and includes a major portion of the trochlea. Disruption of the lateral half of the trochlea disrupts the integrity of the ulno-humeral joint. The distal fragment often migrates and rotates in a proximal direction. This fracture pattern is associated with elbow instability and must be recognized as a distinct entity. The “double-arc sign” is a pathognomonic lateral x-ray finding that represents the sub-chondral bone of the capitellum and the bone of the lateral trochlear ridge.20 The double-arc sign distinguishes these injuries from simple capitellar fractures. Previous reports of capitellum fractures with less medial extension, however, have exhibited a similar “double arc” on x-ray.25
Capitellum Fractures
Anatomy
Osseous
Blood Supply
Ligaments
Biomechanics
Epidemiology and Mechanism of Injury
Classification
| Type | Eponym | Characteristics |
| I | Hahn-Steinthal | Large fragment containing substantial subchondral bone |
| II | Kocher-Lorenz | Sleeve fracture with minimal bone |
| III | Comminuted | |
| IV | Fracture includes a major portion of the trochlea |
Variations
Capitellum fractures have been reported in children. A small series of children was compiled from a major pediatric trauma center.14 A type I fracture pattern was present in six of the seven patients. The average age of the patients was almost 15 years, indicative of the onset of physeal closure. The clinical presentation was similar to adults, although the diagnosis can be more difficult and the fracture fragment size underestimated because of the abundance of cartilage.
A pediatric version of a type IV capitellum fracture has also been reported.15,20 The fracture pattern separated the anterior capitellum and trochlea from the intact posterior humerus. The metaphyseal component (Thurston-Holland sign) is the anterolateral portion of the distal humeral metaphysis. A “double-arc” sign formed by the subchondral bone of the capitellum and the lateral trochlear ridge was present. This growth plate fracture represented a Salter-Harris type IV fracture with interruption of the metaphysis and the epiphyseal plate.33 Similar to adults, a shear mechanism was postulated as the mechanism of injury.15
Assessment and Diagnosis on Presentation
Capitellum fractures are usually the result of a fall.14,20,27 Pain, swelling along the lateral aspect of the elbow, and a joint effusion are prominent findings. The pain is increased during forearm rotation, although pronation and supination are usually not limited. The bony alignment between the posterior olecranon and epicondyles should be normal. Disruption of this configuration implies elbow subluxation or dislocation. Prior to considerable swelling, a large type I fragment may be palpable within the antecubital space.2 This large fragment often creates a bony block to elbow flexion secondary to impingement within the radial fossa. In contrast, a type II osteochondral fracture fragment usually displaces in a posterior direction. The fracture fragment limits flexion as the fragment is forced against the capsule and acts as a mechanical block to extension.3
Marked pain on forearm rotation is suggestive of a combined radial head and capitellum fracture.19,25 Tenderness and swelling along the medial joint line are indicative of a concomitant medial collateral ligament injury.25,26
FIGURE 3-7. Classification of capitellum fractures into four types, according to the size of the fracture fragment and the extent of the fracture line.
FIGURE 3-8. Lateral x-ray of a type I (Hahn-Steinthal) fracture with a large fragment containing substantial subchondral bone.
Imaging
Standard anteroposterior (AP) and lateral x-rays are required after elbow trauma fracture. The AP view can be misleading, as the distal humerus often obscures the capitellum fracture fragment. The lateral projection often reveals a fat-pad sign and disruption of the distal humerus contour with displacement of the semicircular-shaped capitellum (see Figure 3-8). A type I fracture of the capitellum is displaced into the radial fossa with a variable amount of rotation.21,25 An inadvertent oblique x-ray rotates the distal humerus and may prevent visualization of the fracture fragment.17,34
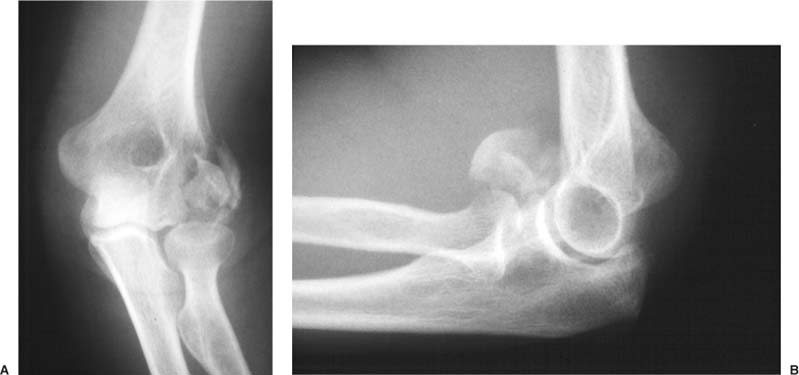
FIGURE 3-9. Anteroposterior (A) and lateral (B) x-rays of a comminuted type III fracture secondary to considerable axial load.
Type II fractures are more difficult to diagnose, and accessory views may be necessary. A radial head-capitellum view can facilitate definition of the fracture fragment.34 This x-ray is a modified lateral view of the elbow joint with the radiographic beam angled 45 degrees toward the radial head. This projection eliminates the overlap between the humeroradial and humeroulnar joints (Figure 3-11). The radial head-capitellum view provides better delineation of small fracture fragments and nondisplaced capitellum fractures than conventional x-rays.
Advanced imaging modalities are often useful to further define the fracture pattern. CT provides high resolution of capitellum fractures. Sagittal reconstructions of the CT scans can help define the fracture line.20
Treatment
A variety of treatment methods have been recommended, including nonoperative management, excision of the fracture fragment(s), and open reduction and internal fixation. Untreated displaced capitellum fracture uniformly leads to a poor functional outcome.2,3 The neglected fracture fragment will block motion or form a loose body. In addition, the bony fragment can proliferate and further diminish elbow motion.3 Eventually, progressive arthritic changes develop over time. The natural history is worse with concomitant disruption of the medial collateral ligament or a type IV fracture. Both instances result in elbow instability and joint degeneration.20,26

FIGURE 3-10. Anteroposterior (A) and lateral (B) x-rays of a type IV coronal shear fracture that involves a substantial portion of the trochlea.

FIGURE 3-11. A radial head-capitellum view eliminates the overlap between the humeroradial and humeroulnar joints (normal elbow).
Nonoperative Treatment
Nondisplaced fractures can be treated by cast immobilization, although careful monitoring is necessary to ensure maintenance of reduction. Initially, displaced fractures were treated by fragment excision and early range of motion. The results were variable when the elbow was stable and dismal when there was concomitant elbow instability. Elbow instability can be related to resection of a fragment that includes the lateral trochlear ridge or release of the lateral collateral ligament during the surgical approach.20,35
Initial attempts at internal fixation were also problematic. Inadequate fixation, iatrogenic avascular necrosis, and repeated displacement were common. The development of small fracture fixation devices and improved surgical techniques has made open reduction and internal fixation more successful.18,20,21,36
Closed Reduction
Closed reduction is another option for treatment of a displaced fracture.10,13,27 The reduction requires anesthesia, and the recommended maneuver is variable. A spontaneous reduction may be obtainable in acute fracture management.27 The procedure is performed under anesthesia, and the arm is gently positioned into extension with the forearm in supination. A lateral x-ray confirms spontaneous reduction of the capitellum fragment. The fragment is locked into place using joint distraction and gradual elbow flexion. The radial head captures the capitellum against the distal humerus within 30 to 40 degrees of elbow flexion.
Another method involves direct manipulation of the fracture fragment. Initial traction is applied to the extended arm with the forearm positioned in supination.10,11,13,37 A varus stress applied to the elbow facilitates reduction. Subsequently, the elbow is flexed, and direct posterior pressure is applied to the fracture fragment.10 The fracture fragment is held in place by the radial head. Forearm pronation positions the radial head against the capitellum for maintenance of fracture reduction.
In general, closed reduction is difficult and repeat displacement is common because the fragment is devoid of soft tissue attachments.3,10,21,25 In addition, the accuracy of reduction is difficult to interpret without advanced imaging studies. Furthermore, 3 weeks of immobilization is required prior to any elbow movement, which results in secondary stiffness.13 These problems have shifted the pendulum toward open reduction and internal fixation as the preferred approach to displaced capitellum fractures, especially in type I fractures.3,20,25 A stable anatomic reduction, however, is mandatory, as insecure fixation requires extended immobilization and slight displacement disrupts joint congruity. Small or comminuted fragments that cannot be effectively secured are often better excised.
Operative Treatment
Surgical intervention is warranted for displaced fractures of the capitellum with or without elbow instability. A type I fracture can be treated by fragment excision or internal fixation, although fixation is preferred to restore lateral column anatomy and stability. A type II or type III fracture is often unfixable and requires fragment excision.3,21 A type IV fracture requires open reduction and internal fixation to restore elbow congruity.
Approach
General or regional anesthesia is appropriate for surgical treatment of capitellum fractures. The patient is placed supine on the operating room table. All bony prominences are padded. A pneumatic tourniquet is applied to the proximal arm. Preoperative antibiotics are administered.
The operative approach to capitellum fractures can be divided into two components. The initial part is fracture exposure, and the second segment is fracture management. The preoperative decision making must consider both elements. The standard exposure is a lateral Kocher approach, which provides wide exposure and ample options for fracture fixation but detaches the lateral collateral ligament complex. The modified lateral approach (or lateral collateral preserving approach) preserves the lateral collateral ligament complex but creates more difficulty with fracture fixation.38,39 This approach is preferred for excision of comminuted capitellum fractures and is quickly becoming the preferential approach for all problems about the lateral column. Fracture fixation may require an anterior or posterior window about the capitellum to obtain access for placement of an internal fixation device.
Standard Lateral Approach
The lateral Kocher approach is between the anconeous and extensor carpi ulnaris (Kocher interval).39 The incision begins along the supracondylar ridge about 2 cm above the radiocapitellar joint and extends 2 to 3 cm distal to the radial head to the subcutaneous border of the ulna. The interval between the extensor carpi ulnaris and anconeous is exposed. The triceps and anconeous are reflected in a posterior direction. The common extensor origin, lateral collateral ligament complex, and anterior capsule are mobilized in an anterior subperiosteal direction (Figure 3-12). The entire lateral muscle mass is elevated, which detaches the lateral collateral ligament. Elevation of the entire tendon and ligament complex as a single unit facilitates repair after fracture management. The anterior sleeve of tendon and ligament must be repaired back to the bone after fracture fixation. Suture anchors may be used to obtain a secure repair of the capsuloligamentous complex. The extensor origin should not be dissected, as a separate layer as the collateral ligament originates from the coalescence of septa between the extensor compartments.38,39
< div class='tao-gold-member'>