Fig. 11.1
A videocapillaroscope that is used in detecting the microcirculation at the level of the nailfold bed
Capillaroscopic Detection of the Early Microvascular Alterations That Are Markers of Secondary Raynaud’s Phenomenon
The morphologic changes that characterize the microvasculature in the scleroderma-spectrum diseases at the level of the nailfold have been extensively described – giant capillaries, microhemorrhages, loss of capillaries, neovascularization, and avascular areas (Fig. 11.2) [2].
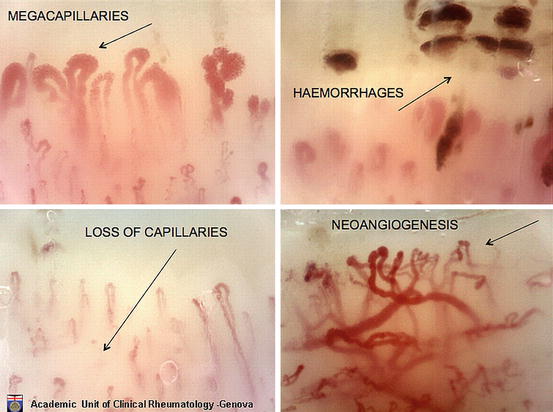
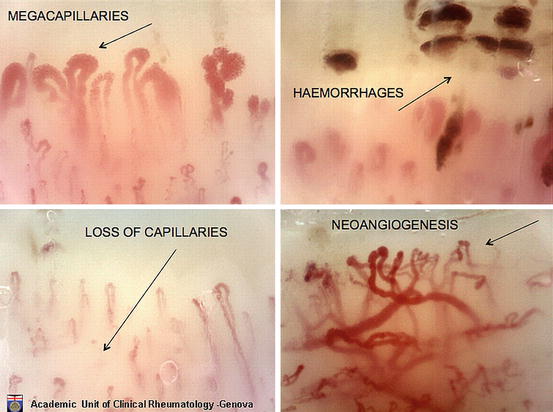
Fig. 11.2
Different microvascular alterations (i.e., giant capillaries, microhemorrhages, loss of capillaries, and neovascularization) that characterize the secondary Raynaud’s phenomenon
The microvascular alterations have been recently reclassified in systemic sclerosis (SSc) into three defined and different NVC patterns:
1.
An “early pattern” (few giant capillaries, few capillary microhemorrhages, no evident loss of capillaries, and relatively well-preserved capillary distribution)
2.
An “active pattern” (frequent giant capillaries, frequent capillary microhemorrhages, moderate loss of capillaries, absence or mild ramified capillaries with mild disorganization of the capillary architecture)
3.
A “late pattern” (almost absent giant capillaries and microhemorrhages, severe loss of capillaries with extensive avascular areas, ramified/bushy capillaries, and intense disorganization of the normal capillary array) [3] (Fig. 11.3)


Fig. 11.3
The three scleroderma patters (early, active, late) compared to the microvasculature in a normal health control subject
The marked increase in capillary size is the most characteristic feature of the nailfold capillary bed (giant capillary) in early secondary RP. In particular, the detection of enlarged and giant capillaries, together with microextravasation (hemorrhage) of the red blood cells in the nailfold, most likely represents the first morphologic sign of the altered microcirculation in systemic sclerosis.
The shape of the widened capillaries is largely heterogeneous, but giant capillaries with a homogeneous enlargement (diameter over 50 μm) are an absolute marker of the scleroderma capillaroscopic pattern. This picture characterizes the “early” (initial) SSc capillaroscopic pattern (Fig. 11.3) [4]. As the pathophysiological process of SSc progresses into fibrosis, the capillaroscopic analysis most likely reflects the effects of tissue hypoxia/massive capillary destruction, then increased loss of capillaries and avascular areas are observed, together with bushy capillaries indicating neoangiogenesis. This advanced stage of the systemic sclerosis is characterized by the “late” capillaroscopic pattern (Fig. 11.3). We know that patients with the “early” capillaroscopic pattern may have had RP for many years, and a transition from primary to secondary RP may be expected in almost 15 % of subjects in an average time of 29 months [5].
Learning to Use Capillaroscopy
Recent preliminary experience indicates that technical and operative skills in capillaroscopy, using a videomicroscopy system, can be achieved in approximately five nonconsecutive hours by an untrained specialist, in the context of a self-teaching program under expert supervision [8]. The beginner’s performances show that self-efficacy increases with practical experience, and image quality is reached in up to 70 % of learners by the third session [8].
Scleroderma Capillaroscopic Patterns and Serum Autoantibodies in Systemic Sclerosis
Regarding the anti-endothelial cell antibodies (AECA), these have been detected significantly more frequent in SSc patients with the “late” capillaroscopic pattern compared to the “early” and “active” patterns (p < 0.05) [9]. Concerning the anti-topoisomerase I (anti-Scl70) and anticentromere (ACA) antibodies, anti-Scl70 were found more frequent again in SSc patients showing the “active” and “late” patterns, whereas ACA especially in patients with the “early” pattern [10].
In a large prospective study, enlarged/giant capillaries, capillary loss, and more SSc-specific autoantibodies independently predicted definite SSc [11]. The authors reported associations between certain patterns of capillary abnormality and different specific autoantibodies. Anti-CENP-B and anti-Th/To antibodies predicted enlarged/giant capillaries; these autoantibodies and anti-RNAP III predicted capillary loss. Interestingly, each autoantibody was associated with a distinct time course of microvascular damage, as gauged by capillary enlargement or capillary loss. At follow-up, 79.5 % of patients with one of these autoantibodies and abnormal findings on nailfold capillary microscopy at baseline had developed definite SSc. Patients with both baseline predictors (abnormal capillaroscopy and an SSc-specific autoantibody) were 60 times more likely to develop definite SSc.
Finally, the association of specific antinuclear antibodies positivity and the presence of the NVC scleroderma pattern have been proposed as biomarkers for the very early diagnosis of SSc together with clinical symptoms (i.e., Raynaud’s phenomenon and/or puffy fingers) [12].
Possible Predictive Value of Capillaroscopy for Clinical Outcome in Systemic Sclerosis Patients
Systemic sclerosis microangiopathy correlates with disease subsets and the severity of peripheral vascular, skin, and lung involvement; in particular, patients with the “late” pattern showed an increased risk to have active disease and have moderate/severe skin or visceral involvement compared to patients with “early” and “active” capillaroscopic patterns [13].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








