CHAPTER 5 Bony Impingement of the Ankle and Subtalar Joints
Ankle sprains are one of the most common injuries seen in sports medicine, and most heal without persistent pain or chronic disability.1,2 However, some patients with ankle sprains continue to have persistent pain and dysfunction.2,3 Two common sources of chronic pain and disability—persistent ankle instability and impingement—may occur separately or concomitantly. Impingement, which is entrapment of an anatomic structure that leads to pain and decreased range of motion of the ankle, can be classified as soft tissue or osseous.4
Osseous or bony impingement most commonly results from spur formation along the anterior margin of the distal tibia and talus or from a prominent posterolateral talar process (i.e., os trigonum). Soft tissue impingement usually results from scarring and fibrosis associated with synovial, capsular, or ligamentous injury, and it most often occurs in the anterolateral gutter, medial ankle, or region of the syndesmosis.5
Of the first few ankle impingement syndromes reported in the English literature, all involved bone. They usually have occurred in athletes whose sports necessitated sudden acceleration, jumping, and extremes of dorsiflexion or plantar flexion. The so-called athlete’s ankle was first mentioned in the orthopedic literature by Morris6 and was subsequently reported by McMurray,7 who called it footballer’s ankle. McMurray stated that the footballer’s ankle was peculiar to the professional soccer player, especially those older than 25 years who have played for many years. In later studies, this entity was described in many other athletic activities, including rugby players, football players, ballet dancers, jumpers, and runners, and it can occur in any sport.
BONY IMPINGEMENT
Etiology
Osteophytes are protrusions of bone and cartilage around the joint space. Osteophytic formations occur with weight-bearing articular cartilage damage, such as osteoarthritis of the hip and knee, and occur without weight-bearing articular cartilage damage, such as bony impingement lesions.8
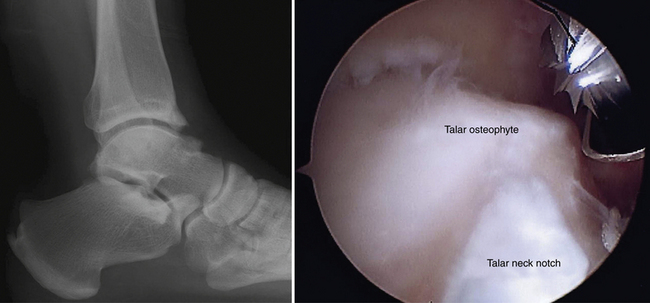
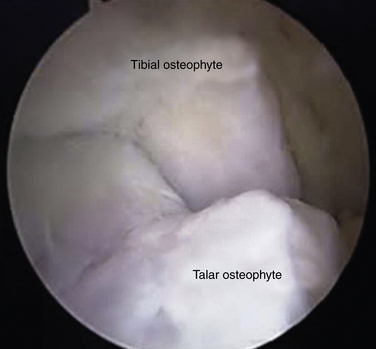
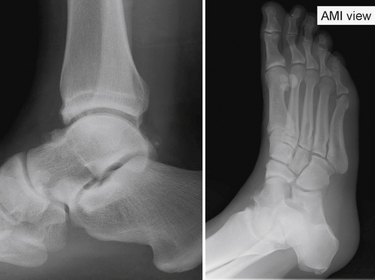
Controversy exists about the cause of bony osteophytes around the ankle with normal articular cartilage. Adjacent or articulating bones that are repetitively in contact can stimulate the cambium layer, the deep layer of periosteum that has osteogenic potential, to form osteophytes. The osteophytic prominence causes bony impingement, often increases in size, and eventually may break off, forming a loose body. After the spur is formed, it may alter normal mechanics or motion of the ankle. Morris6 and McMurray7 described osseous exostoses of the anterior rim of the tibia and the sulcus of the talus, and they believed these to result from a traction injury of the joint capsule of the anterior aspect of the ankle that occurred when the foot was in extreme plantar flexion (i.e., capsule-ligament traction). However, the capsule of the ankle attaches above the location of the tibial osteophytes and distal to the talar ones. In later studies, anatomic observations during arthroscopic surgery confirmed that tibial osteophytes were located at the joint level and talar osteophytes were found proximal to the talar neck notch, away from the capsular attachment sites (Fig. 5-1); the osteophytes were intra-articular.9,10 O’Donoghue11 attributed these exostoses to direct osseous impingement during forced dorsiflexion or to post-traumatic calcification. Van Dijk and colleagues12 attributed the osteophytes to medial impingement from inversion of the talus onto the medial tibia and thought they might be related to instability (Fig. 5-2). The osteophytes were related to direct trauma associated with the impingement of the anterior articular border of the tibia in the talar neck during forced dorsiflexion of the ankle joint.
Classification
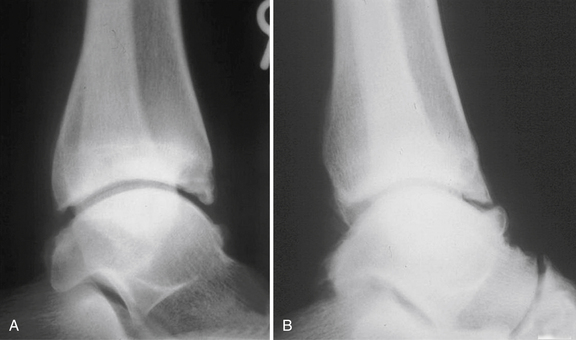
In 1992, Scranton and McDermott8 classified four types of anterior ankle impingement by the radiographic appearance of bony spurs (Table 5-1). The classification system grades the degree of spur formation and assists in predicting the length of recovery time. Van Dijk’s 1997 radiographic classification (Table 5-2) was based on osteoarthrosis of the ankle on plain radiographs (Fig. 5-3).10 The degree of osteoarthritic change is a better prognostic indicator for the outcome of arthroscopic surgery for anterior ankle impingement than size and location of spurs.
TABLE 5-1 Classification of Anterior Ankle Impingement
From Scranton PE Jr, McDermott JE. Anterior tibiotalar spurs: a comparison of open versus arthroscopic débridement. Foot Ankle. 1992;13:125-139.
TABLE 5-2 Classification of Osteoarthritic Changes of the Ankle Joint
| Grade | Characteristics |
|---|---|
| 0 | Normal joint or subchondral sclerosis |
| I | Osteophytes without joint space narrowing |
| II | Joint space narrowing with or without osteophytes |
| III | Total disappearance or deformation of the joint space |
From van Dijk CN, Tol JL, Verheyen CC. A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med. 1997;25:737-745.
THE ANKLE JOINT
The Anterior Ankle
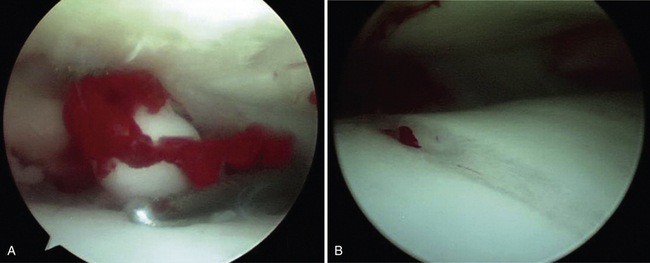
Anterior impingement syndrome of the ankle is the most common cause of anterior ankle pain in many sports participants. Repetitive forced dorsiflexion also can result in impaction-related microtrauma of the anterior chondral margin of the tibiotalar joint. Over time, attempted repair with resultant fibrosis and fibrocartilage proliferation leads to the formation of osteophytes.7 When osteophytes form, they limit dorsiflexion, facilitate further impingement, and result in more periosteal stimulation, creating a repetitive cycle. Careful inspection of the pathologic anatomy shows that osteophytes do not form in the capsular insertion but instead where bones come together.11 Osteophytes can break off and become loose bodies (Fig. 5-4).
In supination injury, damage to the anterior non–weight-bearing cartilage rim occurs.12 The cartilage proliferation, scar tissue formation, and calcification that may result from attempted repair depend on the degree of initial damage and on chondral and bone cell stimulation. Recurrent forced dorsiflexion of the ankle is the main factor in the development of spurs.13,14 Another factor is recurrent microtrauma, and it has been demonstrated that spur formation is related to recurrent ball impacts in soccer players.15 The entire process of spur formation and hypertrophied synovium or fibrosis is exacerbated by recurrent ankle sprains and persistent ankle instability. Synovial changes may result from chronic inflammation of the soft tissue (e.g., synovial fold, subsynovial fat, collagen tissue) that was crushed during forced dorsiflexion movements between spurs.16
The common history of patients with anterior ankle impingement is recurrent inversion sprain. The typical patient is a young athlete presenting with chronic anterior ankle pain.17 Pain likely results from entrapment of hypertrophied synovial tissue between the talus and the anterior tibia, which is exacerbated by the presence of anterior spurs. Patient usually present with swelling after activity and with limited ankle dorsiflexion movement.
Standard lateral radiographs of the ankle usually show spurs. The weight-bearing lateral view with the ankle in maximal dorsiflexion (i.e., plié view) demonstrates anterior impingement, and this view commonly is used in evaluating dancers. Conventional magnetic resonance imaging (MRI) accurately detects and localizes anterior tibiotalar spurs, adjacent reactive synovitis and fibrosis, subchondral bone edema, and other coexisting lesions, such as collateral ligament complex injury, osteochondral lesions of the talus, or intra-articular bodies. There is little or no additional information gained through indirect magnetic resonance (MR) arthrography for evaluating anteromedial impingement compared with conventional MRI.18
Several conditions can mimic the anterior impingement syndrome, including osteochondritis dissecans of the talus, a “high” ankle sprain involving the anterior tibiofibular ligament,19 impingement by Bassett’s ligament,1 an aberrant distal insertion of the anterior tibiofibular ligament that can cause persistent symptoms, Ferkel’s disease,16 an accumulation of debris and synovitis in the anterolateral gutter, degenerative joint disease of the tibiotalar or talonavicular joints (especially in the early phases when the radiographic findings are subtle), and a stress fracture or an osteoid osteoma in the tarsal navicular.
Conservative treatment with rest, physical therapy, shoe modification, or local injection constitutes first-line therapy for most cases of anterior ankle impingement. If all modalities of conservative treatment are unsuccessful, operative treatment may be indicated. The goal of surgery is removal the osteophytes to restore the anterior space and to reduce the chance of symptoms recurring. Numerous investigators have reported good results with open arthrotomy, but it can be complicated by cutaneous nerve entrapment, wound dehiscence, damage of the long extensor tendons, and formation of hypertrophic scar tissue.7,11,17 In recent years, the arthroscopic treatment of anterior ankle impingement has had a high success rate. The first series reported by Biedert3 had a success rate of approximately 67%. Ferkel and colleagues16 reported a success rate of approximately 84% for 31 patients with soft tissue impingement of the ankle. Ogilvie-Harris and colleagues20 described an average of 39 months’ follow-up for patients who were treated for anterior ankle impingement by arthroscopic removal of bony spurs. The good and excellent results were obtained for 88% of 17 patients.20 In a prospective study, Amendola and coworkers21 treated 79 cases of ankle impingement by arthroscopic débridement. Fifteen cases of soft tissue impingement and 14 cases of anterior bony impingement were included in the study. There were statistically significant decreases in subjective analog scores. Eighty percent of the soft tissue impingement lesions and 86% of the bony impingement lesions benefited from the procedure. Eighteen percent of patients had neurologic complications, including partial deep peroneal nerve neurapraxia and superficial peroneal nerve irritation.21
Scranton and colleagues8 reported the comparative open and arthroscopic treatment of ankle impingement. The recovery time of the arthroscopic treatment patients was approximately one half of the time of open treatment patients. The patients treated arthroscopically returned to full athletic training 1 month faster than the other group.8
Tol and associates9 described the results for 5 to 8 years of follow-up for the arthroscopic treatment of anterior impingement in the ankle. Excellent or good results were obtained for 100% of patients without osteoarthritis, 77% of patients with grade I disease, and 53% of patients with grade II diseases according to the classification for osteoarthritis of the ankle (see Table 5-2).22 Osteophytes recurred in two thirds of the ankles with grade I osteoarthritis, but the recurrence of osteophytes did not correlate statistically with the return of symptoms. Narrowing of the joint space increased in 47% of patients with grade II osteoarthritis.9
Anteromedial Ankle Impingement
Anteromedial ankle pain is caused by impingement of the anterior portion of the medial malleolus on a spur on the medial shoulder of the talus. Spurs often occur on both sides of the joint. They result from injury to the deltoid ligament complex, leading to scar formation and synovitis along the anteromedial joint line. Patients complain of pain along the anteromedial joint line that is aggravated by walking or sporting activities. Patients often report a clicking sensation and painful limited dorsiflexion of the ankle. On physical examination, the anteromedial aspect of the ankle appears swollen and is tender to palpation over the anterior tibiotalar fascicle of the deltoid ligament. The anteromedial spur often can be palpated on physical examination but usually cannot be visualized on standard anteroposterior and lateral radiographs of the ankle. In a cadaver study, Tol and colleagues15 described medially located talar osteophytes and anteromedial tibial osteophytes that were up to 7.3 mm in diameter, originated from the anteromedial border, and could remain undetected due to overprojection or superposition of the lateral part of the talar neck and body and the prominent anterolateral border of the distal tibia, respectively.15
These osteophytes are easy to miss (i.e., “hidden spurs”). A special oblique anteromedial impingement view (Fig. 5-5) has been developed to aid in the detection of anteromedial spurs, and it is obtained with the beam tilted in a 45-degree craniocaudal direction with the leg in 30 degrees of external rotation and the foot in plantar flexion in relation to the standard lateral radiograph position.23 The sensitivity of lateral radiographs for detecting anterior tibial and talar osteophytes is 40% and 32%, and their specificity is 70% and 82%, respectively. The combination of lateral and oblique anteromedial impingement radiographs of the ankle increase the sensitivity to 85% for tibial osteophytes and 73% for talar osteophytes.24
Conventional MRI has not been useful in detecting anteromedial impingement syndrome. Robinson and associates25 demonstrated that the cross-sectional MR arthrography could confirm anteromedial ankle impingement. Their findings included capsular and synovial soft tissue thickening anterior to the tibiotalar ligaments and associated osseous abnormalities such as anteromedial osteophytes.25 The impingement is thought to be soft tissue entrapment associated with previous injury to the anterior tibiotalar fascicle of the deltoid ligament complex. A thickened anterior tibiotalar ligament can impinge on the anteromedial corner of the talus, often resulting in adjacent fibrosis or a meniscoid lesion and synovitis that may lead to adjacent spur formation.
Anterocentral Ankle Impingement
Anterolateral Ankle Impingement
Bassett’s Ligament.
Bassett’s ligament impingement is caused the distal fascicle of the anteroinferior tibiofibular ligament.1 It is a thickened distal fascicle of the anteroinferior tibiofibular ligament (AITFL) that extends far distally on the lateral malleolus. Nikolopoulos and coworkers26 considered this fascicle to be an independent accessory ligament. This anatomic structure represents a separate ligament rather than a distal component of the AITFL. A fibrofatty septum separated the AITFL from the accessory fascicle, similar to the one that covered the intermediate space between the interosseous and the anterior tibiofibular ligament.26 The lateral shoulder of the talus impinges against the distal fascicle of the AITFL when the ankle is plantar flexed. Patients had a history an inversion sprain of the ankle followed by chronic pain in the anterior aspect of the ankle, but they had no gross ligamentous instability. The post-traumatic anterolateral hyperlaxity due to an injured ATFL resulted in anterior extrusion of the talar dome with dorsiflexion, which contacted the distal fascicle of the AITFL with more pressure and friction.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree