70 Bone grafts have been used in orthopedic surgery since the 1800s. Early techniques were only modestly successful and were applied primarily toward the treatment of fractures. Many of the current bone grafting methodologies began to be developed in the 1940s by the U.S. military. Over the next few decades, techniques like freeze-drying, fresh freezing, and irradiation continued to develop, and their use became more widespread. Still, it was not until the last few decades that advanced techniques, such as bone marrow aspirate, bone morphogenic protein (BMP), and autologous platelet concentrate, came into wide use. The use of bone grafts and bone graft substitutes in spine surgery has been steadily increasing for several reasons. Successful fusion of separate spine segments requires the formation of bridging bone as well as maintenance of correct alignment. While good results have been obtained with the current gold standard (iliac crest autograft), there has been a general trend in the spine community to decrease its use because of significant long-term graft harvest site pain. Furthermore, advances in medical care have permitted older patients as well as patients with significant comorbidities to undergo more complex spinal surgical procedures. These factors have led to increased use of the more advanced bone grafting techniques, occasionally without good data to support their use. Selection of appropriate bone graft options is based on several factors. The osteogenicity of a bone graft is its ability to directly contribute bone-forming cells and directly induce new bone formation. Osteoconductive bone grafts provide a scaffold for new bone formation. Osteoinductive bone grafts induce differentiation of osteoprogenitor cells into osteoblasts. Structural bone grafts and extenders provide a rigid support to the construct. Tricortical iliac crest autograft is widely considered to be the gold standard, as it is osteogenic, osteoconductive, and osteoinductive, and provides structural support. However, its use is limited by its finite supply, and there is significant morbidity associated with the harvesting procedure, including the potential for infection, nerve injury and donor site pain. These problems have led to the development of various bone grafting options. Cadaver bone is available as both structural and nonstructural allografts. The cadaver bone is processed after harvesting to decrease its antigenicity as well as the risk of disease transmission. This causes the allograft to lose its osteogenic, and most of its osteoinductive, properties. While some studies have demonstrated the superiority of structural autograft over allograft with regard to fusion rates, overall success rates, and maintenance of interspace height in anterior cervical fusions, there is also good evidence suggesting the noninferiority of allograft structural bone in single-level instrumented and uninstrumented anterior cervical fusions. The evidence is less ambiguous in posterior lumbar spine fusions; autografts result in higher fusion rates and higher density of fusion mass than allografts. Demineralized bone matrix (DBM) is obtained by demineralization of bone allograft, leaving behind collagen and other noncollagenous proteins and growth factors. This process results in loss of structural support but retains the osteo-conductive and weakly osteoinductive properties of autograft. It is available in several forms, including sheets, putties, and injectable gels. There is minimal oversight by the U.S. Food and Drug Administration (FDA) regarding the minimum quality and testing requirements, leading to wide variability in osteoinductive qualities of products produced by different vendors and even between individual lots of the same product. The lack of any structural strength in DBM limits its use in anterior lumbar and cervical interbody fusions. DBM use in anterior cervical discectomy and fusion procedures with structural allografts has been associated with a greater rate of pseudarthrosis and collapse than autograft. Still, results of DBM used in conjunction with a cage or structural bone graft and internal fixation have shown high fusion rates and good clinical outcomes. The evidence for DBM use in posterior lumbar fusion surgeries is much stronger. Several studies have demonstrated that DBM use in conjunction with autograft leads to fusion rates similar to when larger amounts of autograft without DBM are used. Prior to use of any DBM product it is advisable to investigate the individual DBM product’s testing data to make sure that it has effective osteoinductive properties. Several growth factors, such as transforming growth factor-beta (TGF-beta) and platelet-derived growth factor (PDGF), have been noted to promote bone and tendon healing following injury via promotion of mesenchymal cell differentiation and proliferation. Improved outcomes have been noted with local injection of autologous growth factor concentrate in some sports injuries, such as lateral epicondylitis and Achilles tendon injuries. Applications of these techniques in spine surgery, though, have not been as successful. Several studies demonstrated faster time to fusion with such autologous growth factor concentrates, but there was no effect on overall fusion rates. At this time, convincing evidence for use of autologous platelet products in spine fusion surgery is lacking. Ceramics, such as calcium carbonate and beta-tricalcium phosphate, provide an osteoconductive scaffold for new bone formation but lack osteoinductive and structural support qualities. Some ceramic bone graft substitutes may be coated with hydroxyapatite, which may improve bone ingrowth. While ceramics can be manufactured in different shapes and sizes, they are brittle and require internal fixation when used as a structural bone graft substitute. Ceramics require large surface areas of decorticated bone for optimal fusion in the lumbar spine. This limits their use in intertransverse posterolateral fusions, even in conjunction with bone marrow aspirate or local bone graft. However, some data show that good fusion rates can be achieved when ceramics are combined with autograft and large, bleeding bone surface areas are available. Good results have also been obtained when ceramics were combined with BMP. The use of ceramics in anterior spine surgery appears to have better results than in posterior spine procedures. Good fusion rates have been obtained when ceramics are used in anterior cervical interbody fusions in conjunction with rigid plating. While there is little evidence to support the use of ceramics in stand-alone anterior lumbar interbody fusions (ALIFs), good results have been obtained when they have been used as part of circumferential instrumented fusions. Mesenchymal stem cells have a significant osteogenic potential owing to their ability to differentiate into an osteoprogenitor cell lineage. Bone marrow aspiration can provide a large number of mesenchymal stem cells without the morbidity associated with iliac crest harvest. Stem cells can be obtained via both iliac crest aspirations and transpedicular vertebral body aspiration, with some data demonstrating higher numbers of progenitor cells obtained using the latter. Bone marrow aspirate needs to be combined with an osteoconductive carrier for optimal fusion mass formation. Equivalent clinical outcomes and radiographic fusion rates have been achieved when bone marrow aspirate with a collagen/hydroxyapatite matrix was compared with iliac crest autograft in posterolateral fusions. Similarly, bone marrow aspirate with a collagen carrier and allograft may be a good and cost-effective alternative to BMP with a collagen carrier in revision single-level posterior spine fusions. On the other hand, bone marrow aspirate appears to be less effective than autograft in anterior lumbar procedures. Still, at this time there are limited data available on the efficacy of bone marrow aspirate in spine fusion procedures. Although BMP was identified in 1965, it became widely commercially available since about 2000. This protein has significant osteogenic potential, but it lacks structural and osteoconductive properties. The two currently commercially available BMP products are rhBMP-2 and rhBMP-7. Both BMPs must be used with a carrier matrix to prevent rapid dissolution from the operative site. BMP-2 is currently FDA approved for use in ALIF procedures. Level 1 evidence suggests that BMP-2 produces better clinical results and fusion rates than allograft alone, and the clinical and radiographic results are equivalent to autograft. Cost analysis studies have also demonstrated that while the initial cost of BMP-2 use is higher than that of iliac crest autograft, long-term costs may be similar because of avoidance of the morbidity associated with autograft harvest. Excellent results have also been noted with BMP-2 use in posterior lumbar spine fusions. Several studies have demonstrated equivalent or better clinical outcomes and fusion rates with use of BMP compared with iliac crest autograft, both with and without pedicle screw instrumentation. BMP-2 use in posterior lumbar spine fusions is currently physician-directed, as it is not FDA-approved for these procedures. Similarly, BMP-2 use in the anterior cervical spine has been reported to result in improved fusion rates. This may be particularly important in multilevel procedures, where it may obviate the need for posterior supplemental fixation. Still, significant complications such as dysphagia and increased prevertebral swelling due to local inflammation have been associated with BMP-2 use. Although these appear to be dose-dependent, the FDA put out a public health notification in June 2008 regarding possible life-threatening complications associated with rhBMP use in the anterior cervical spine. Several other complications have also been noted with BMP-2 use. A small percentage of patients have had aggressive early resorption of bone graft as well as surrounding host bone following BMP use. Ectopic bone formation around nearby neural structures has also been reported. The use of BMP-2 for posterior and transforaminal interbody fusions has been associated with increased rates of postoperative radiculitis. Accordingly, while BMP is a very strong bone-forming adjuvant, its potential side effects and significant cost should be considered prior to its use. Despite the multiple bone graft and bone graft substitute options currently available, good evidence as to which option is better or may be more appropriate for a given indication is lacking. In general, anterior lumbar procedures require structural support, and good results have been obtained with both structural allograft as well as a cage with demineralized bone matrix. Concomitant use of bone morphogenic protein has led to increased fusion rates in these procedures. Similarly, anterior cervical procedures require structural support, and good fusion rates have been achieved with structural allograft or cages with demineralized bone matrix when used with anterior plate fixation. Multiple graft options are reasonable for posterior lumbar and cervical procedures. DBM with local autograft, as well as bone marrow aspirate with a collagen sponge, typically result in good fusion rates. When a large decorticated area is available for fusion, ceramics with local autograft have also led to good clinical and radiographic results. Still, further research is necessary to clearly delineate appropriate indications for each bone grafting option. Bishop RC, Moore KA, Hadley MN. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate: a prospective comparative analysis. J Neurosurg 1996;85(2): 206–210 PubMed This excellent study compares the outcomes of allograft versus autograft in anterior cervical interbody fusions. This study also noted the detrimental effect of smoking, particularly in the allograft group. Cammisa FP Jr, Lowery G, Garfin SR, et al. Two-year fusion rate equivalency between Grafton DBM gel and autograft in posterolateral spine fusion: a prospective controlled trial employing a side-by-side comparison in the same patient. Spine 2004;29(6):660–666 PubMed This study compared iliac crest autograft and DBM with a smaller amount of autograft side by side in the same patients. Authors noted that the use of DBM can produce equivalent fusion results while decreasing the amount of autograft needed, thus possibly reducing the risk and severity of donor site morbidity. Chen WJ, Tsai TT, Chen LH, et al. The fusion rate of calcium sulfate with local autograft bone compared with autologous iliac bone graft for instrumented short-segment spinal fusion. Spine 2005;30(20):2293–2297 PubMed Iliac crest bone graft on one side was compared with local autograft with calcium sulfate on the other side in the same patient undergoing instrumented one- or two-level lumbar spine fusion. The authors noted that the fusion rates were equivalent among the two groups. Dimar JR, Glassman SD, Burkus KJ, Carreon LY. Clinical outcomes and fusion success at 2 years of single-level instrumented posterolateral fusions with recombinant human bone morphogenetic protein-2/compression resistant matrix versus iliac crest bone graft. Spine 2006;31(22):2534–2539, discussion 2540 PubMed This is a prospective, randomized study comparing autograft to BMP with compression-resistant matrix in posterolateral spine fusions. The authors noted higher fusion rates and lower operative time and blood loss in the BMP group. Lewandrowski KU, Nanson C, Calderon R. Vertebral osteolysis after posterior interbody lumbar fusion with recombinant human bone morphogenetic protein 2: a report of five cases. Spine J 2007;7(5):609–614 PubMed This report of five cases draws attention to the possible complication of vertebral osteolysis following transforaminal lumbar interbody fusion with BMP. Although all cases resolved with nonoperative care, the possibility of this complication should be considered. Neen D, Noyes D, Shaw M, Gwilym S, Fairlie N, Birch N. Healos and bone marrow aspirate used for lumbar spine fusion: a case controlled study comparing Healos with autograft. Spine 2006;31(18):E636–E640 PubMed The authors compare the fusion rates of bone marrow aspirate with a collagen sponge versus iliac crest autograft in both anterior and posterior lumbar spine fusions. They note equivalent fusion rates in the posterior procedures among the two options. The fusion rates of the iliac crest autograft were noted to be superior to those of the bone marrow aspirate/collagen sponge group in the ALIFs. Samartzis D, Shen FH, Goldberg EJ, An HS. Is autograft the gold standard in achieving radiographic fusion in one-level anterior cervical discectomy and fusion with rigid anterior plate fixation? Spine 2005;30(15):1756–1761 PubMed This very good study demonstrates equivalent and excellent results of one-level anterior cervical interbody fusion with rigid plate fixation comparing autograft and allograft. Smoking was not noted to affect fusion rates significantly. This study demonstrates the advantage of rigid plate fixation when compared to the Bishop et al. 1996 study noted previously. Taghavi CE, Lee KB, Keorochana G, Tzeng ST, Yoo JH, Wang JC. Bone morphogenetic protein-2 and bone marrow aspirate with allograft as alternatives to autograft in instrumented revision posterolateral lumbar spinal fusion: a minimum two-year follow-up study. Spine 2010; 35(11):1144–1150 PubMed This retrospective cohort study compares autograft, BMP, and bone marrow aspirate in revision instrumented posterolateral lumbar fusions. The authors noted that BMP may be a reasonable alternative to autograft in both single and multilevel revision surgeries, while bone marrow aspirate may produce equivalent results at a lower cost and morbidity than either of the other options in single-level procedures. Vaidya R, Carp J, Sethi A, Bartol S, Craig J, Les CM. Complications of anterior cervical discectomy and fusion using recombinant human bone morphogenetic protein-2. Eur Spine J 2007;16(8):1257–1265 PubMed This retrospective study evaluates the safety and cost of BMP use in anterior cervical discectomy and fusion. The authors noted that the use of BMP resulted in significantly higher rates of prevertebral swelling and dysphagia than in the allograft/DBM group, while the cost of the allograft/DBM group was much lower. Wang JC, Alanay A, Mark D, et al. A comparison of commercially available demineralized bone matrix for spinal fusion. Eur Spine J 2007;16(8):1233–1240 PubMed This study demonstrates that there are significant differences between different commercially available DBM products. Prior to the use of a DBM product, its data should be thoroughly examined, as the osteogenic potential may vary significantly.
Bone Graft Substitutes/Biologics
![]() Bone Graft Substitute Options
Bone Graft Substitute Options
Allografts
Demineralized Bone Matrix
Autologous Growth Factor Concentrate
Ceramics
Bone Marrow Aspirate
Bone Morphogenic Protein
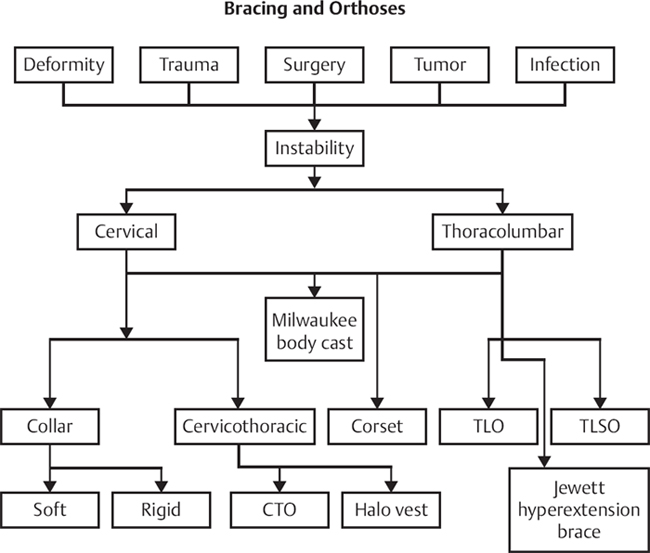
![]() Decision Making
Decision Making
Suggested Readings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






