10
Bites to the Hand
Kevin D. Plancher
History and Clinical Presentation
A 17-year-old college student presented to the emergency room with an open wound to the dorsum and a piece of human tooth in the wound. The patient reported he had been in a bar brawl last evening. Closed fist injuries are encountered almost exclusively in young males, usually occurring during adolescence through the fourth decade of life. Although toddlers are notorious for biting each other, these injuries tend to be superficial and low risk.
PEARLS
- Open lavage with adequate debridement to avoid complications.
- Early intervention to avoid collar button abscess
- Appropriate immediate antibiotic coverage
- Must evaluate the wound in the same position as the injury occurred to appreciate the depth
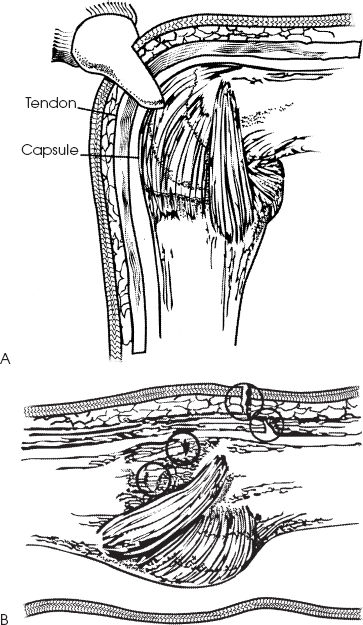
Figure 10–1. (A) Tooth from bite severing skin and entering metacarpophalangeal (MP) joint of the hand. (B) Although the wound looks small and innocuous, when the digit is in extension the penetration is much deeper. Adequate debridement and opening of the wound are essential.
PITFALLS
- Undertreatment with closure of wound seen after 8 hours from injury
- Underestimation of full depth of penetration to wound and joint
Physical Examination
If the bite results in a puncture wound that is swollen, red, and painful, the wound is likely to be infected. Patients with infection may have an elevated temperature, swollen glands, or a history of fever. Any loss of motion or sensation in the fingers suggests that a tendon or nerve has been severed. If a flexor tendon has been severed, the patient will be unable to extend or flex some portion of the finger. When a nerve has been lacerated, there is a loss of sensation over the tip of the finger.
Closed fist injuries often result in injury to the extensor tendon and its sheath. When a closed fist injury occurs to someone with a clenched fist, the bacterial load is often carried back into the hand as the tendon slides back to its relaxed state (Fig. 10–1). This means that the problem of contamination cannot be easily resolved using normal methods of irrigating and cleaning a wound.
Patients who present with dog or cat bites have a wounded area that is painful, red, and swollen. Abscess formation may develop.
Diagnostic Studies
Wound cultures are used to diagnose the infecting organisms. Aerobic and anaerobic cultures should be included. For human bites, the most common infecting organisms include Staphylococcus aureus, streptococci, and Eikenella corrodens. For cat bites, cultures should be examined for Pasteurella multocida. For dog bites, Straphlococcus aureus, Streptococcus viridans, Bacteroides spp., and P. multocida may be cultured. All patients with lacerations over the metacarpophalangeal joint should be x-rayed for retained teeth fragments, regardless of patient-reported history.
Radiographs are used to exclude fractures or foreign bodies (e.g., teeth). Radiographs can be used to determine if osteomyelitis is present, which has been frequently reported in cat bites.
Differential Diagnosis
Puncture wound
Insect bite
Other animal bite
Marine animal bite
Diagnosis
Human Bite to the Hand
There are two major mechanisms of human bites to the hand. An example of penetrating trauma is a closed fist injury, in which one person strikes another in the mouth, causing a fight bite to the hand. If the hand is clenched in a fist, laceration of the skin over the knuckle may damage a tendon sheath or tendon, as well as surrounding tissue or underlying bones of the joint. Wounds over the fingers or other surfaces of the hand are the result of a direct and deliberate (“chomping”) human bite (Fig. 10–2). The most common site of injury is the third and fourth digits at the metacarpophalangeal joint. Osteochondral fractures are common.










