Fig. 26.1
Anatomical relations of the distal biceps tendon with the radius and ulna in supination (a) and pronation (b) (School of Anatomical Drawing, University of Bologna, Rizzoli Orthopaedic Institute)
26.1.3 Clinical Presentation
Usually, the patients refer to the tendon rupturing during sudden extension of the flexed elbow. This movement produces an eccentric muscular contraction followed by pain in the antecubital fossa. Also, an audible pop is often felt before the pain sensation and the appearance of an ecchymosis. After the acute pain has decreased, a feeling of discomfort or pain of minor intensity is felt during elbow flexion and more severely during active supination. At the clinical observation the normal biceps contour disappears and an odd profile appears, called “Popeye deformity”. This type of deformity is more evident in patients with a well-developed muscular mass. At the acute stage patients do not complain about restrictions of flexion, extension, pronation and supination. An evaluation of strength proves difficult, as pain affects the clinical results. At the subacute stage the patient refers to easy fatigability during consecutive movements of supination together with elbow flexion. Although this is the typical clinical history, tendon rupture can also go unrecognised, especially when the lacertus fibrosus remains intact. If the lesion is misdiagnosed and not adequately treated, pain gradually decreases over time. About 21 days after trauma most of the patients feel no pain or functional limitation, which is revealed only when resuming working or the recreational activities formerly performed. A chronic lesion is more difficult to treat and the results are worse [6, 7]; therefore, early clinical diagnosis is important. Several authors have made the effort to define a clinical test with good sensitivity and specificity for distal biceps lesions. Ruland et al. [6] have suggested a test similar to the Thomson test for Achille’s tendon lesions, with “squeezing” of the biceps muscle belly while observing whether or not spontaneous forearm supination takes place. The test is positive when the movement is absent. Thomson [7] have described the “hook test”. The examiner tries to “hook” the tendon in the antecubital fossa with the elbow during 90° flexion. When this is not possible there is a high probability that the tendon is broken. The results of their study indicate sensitivity and specificity of about 100 %, compared with 92 % sensitivity and 85 % specificity for MRI in the same patients. The authors stress the importance of grasping the lateral part of the tendon to avoid the medially placed lacertus fibrosus provoking misdiagnosis of the lesion.
In our experience, the clinical examination has proved essential. The history of the traumatic event may be evident, while sometimes it suggests more subtle lesions with sequential two-stage ruptures, without any evident sprain and with a history of recurrent or chronic pain. An accurate evaluation looking for a popeye sign is important; however, a thick subcutaneous fat layer can hide it. Care also has to be taken in palpating the muscle mass of the retracted biceps. As time since the traumatic event passes, the deformity becomes more evident and the muscle tone improves. A less retracted but evidently flaccid muscle indicates an acute lesion. The hook test remains the best, to be performed several times, with the elbow during flexion, during different degrees of pronation and supination. In any case, only a comparison with the opposite limb allows clinical examination to indicate the diagnosis.
A differential diagnosis with other possible causes of pain in the antecubital fossa is always necessary; namely, biceps tendon tendinitis, a partial tendon lesion, bursitis, posterior interosseous nerve syndrome and entrapment of the lateral cutaneous nerve of the forearm.
26.1.4 Diagnostic Examinations
26.1.4.1 X-Ray
Plain radiograms have no diagnostic value in distal biceps tendon lesions, but they are useful for a general assessment and to rule out possible concomitant bone lesions. No cases have been reported with radiographically visible bony avulsions. When present, calcific degeneration of the biceps insertion may be demonstrated; however, this does not imply a tendon lesion.
26.1.4.2 MRI
Magnetic resonance imaging is the gold standard examination for identifying these lesions. Usually, it is performed with the arm in extension and in the axial plane, owing to the longitudinal course of the tendon in the antecubital fossa. This type of view allows easier diagnosis of partial tears that are otherwise difficult to identify [8, 9].
Giuffre and Moss [9] described a technique for optimal patient positioning, allowing examination of the whole length of the tendon from the musculotendinous junction to the insertion on the radial tuberosity in at least one if not two sections. The patient is placed inside the scanner in prone position with the arm to be examined elevated overhead (shoulder in 180° abduction with the arm beside the head, the elbow in 90° flexion, the forearm in supination and the thumb pointing upwards). This position is known under the acronym FABS (flexion, abduction, supination). The optimal equipment includes a shoulder coil to be placed around the elbow, so that it lies in the middle of the magnets. The FABS sequence is added to the conventional positions of the biceps.
26.1.4.3 Echography
Ultrasound imaging has been extensively used for the diagnosis of distal biceps rupture, as it has a lower cost and greater availability than MRI. This technique allows the continuity of the distal tendon or changes in its size to be assessed [9]. Dynamic ultrasound examination can help in distinguishing between partial and complete rupture. Unfortunately, this is an operator-dependent diagnostic technique, less reproducible than MRI, and it loses both sensitivity and specificity in obese patients, or those with highly developed muscular masses, or those with previous surgical procedures in the same area. Echography, therefore, requires an operator with very good musculoskeletal pathology training. Bird [10] developed the use of the pronator teres acoustic window, which can provide better visualisation of the bicipital insertion.
26.1.5 Treatment
26.1.5.1 Conservative
The first studies on these lesions suggested that conservative treatment might be the best therapeutic option, allowing excellent functional recovery as early as 4 weeks after the event [10–12]. In 1985, Baker and Bierwagen [13] were the first to examine the changes in strength in conservatively treated patients compared with those who had received surgical treatment. The results reported in their study show a 40 % loss of strength during supination, a 79 % loss in supination cycles, and a 30 % loss of strength during flexion, both absolute and cyclic, for non-surgical patients compared with those undergoing surgery. Morrey et al. [14] reported similar conclusions, with a 40 % loss during supination and a 30 % loss during flexion. These studies have stressed how the bicipital action occurs primarily during supination and only secondarily during elbow flexion. More recently, two studies conducted by Chillemi et al. and by Hetsroni et al. [15, 16] have shown that even from the view point of clinical scoring systems (European Society for Surgery of the Shoulder and Elbow Score) and of subjective and objective perceptions (isokinetic tests) the results are superior after surgical treatment to those after conservative treatment. The most recent trial, with the wider pool of patients and the longest follow-up, has been conducted by Freeman’s group [17]. They showed after conservative treatment supination strength equal to 74 % and flexion strength equal to 88 % compared with the contralateral healthy side, and the results were better when the lesion had occurred in the non-dominant arm (83 % vs 60 % for supination strength). In the same study, it was once again demonstrated that the main loss of strength after conservative treatment concerned supination—74 % vs 101 % of surgical patients—and it was confirmed that the gap increased in the case of lesions of the dominant arm. Disabilities of the arm, shoulder and hand (DASH) scores, however, were inferior (lower impairment) in conservatively treated patients than in those who had received surgery. The authors’ conclusion is that the results in subjective outcomes should be attributed to the absence of surgery and to the post-operative protocol.
Nowadays, we therefore restrict conservative treatment to sedentary patients who have no need for full absolute strength and who do not perform repetitive movements, mainly during pronosupination, patients who cannot be scheduled for surgery and those who voluntarily elect to accept loss of muscular strength and endurance rather than facing the risks of surgery and the long recovery time. Conservative treatment includes temporary immobilisation, the use of drugs for pain control and then rehabilitation cycles. Resuming previous manual activities is allowed as soon as the patient feels ready, usually no longer than 1 month after the tendon rupture. Even though cases are reported in which there is persistent discomfort or pain in the antecubital fossa, the results are generally satisfactory.
26.1.5.2 Anatomical or Non-anatomical Repair
When the advantages of the surgical treatment as the best therapeutic option for the lesions of the distal biceps were understood, the question arose of whether an anatomical or a non-anatomical repair might be better. The first option involves the reinsertion of the tendon at the radial tuberosity, whereas the second one is aimed at suturing the tendon to the brachialis muscle. The literature review by Ratanen and Orava about 147 patients [18] describes a higher level of clinical satisfaction in the patients operated on using an anatomical procedure than in those subjected to non-anatomical surgery (60 %) or conservative treatment (14 %). More recently, Klonz et al. [19] evaluated using an isokinetic test the real functional recovery of patients operated on using both techniques, detecting similar values in flexion strength recovery, but a definitely lower supination strength in patients with a non-anatomical reconstruction. On the other hand, patients subjected to an anatomical repair had a higher rate of heterotopic ossifications.
Nowadays, when the indication for surgery is selected, the anatomical reinsertion of the tendon is preferred. Suturing the tendon to the brachialis muscle is a salvage option for the few cases in which taking the biceps tendon back to the radial tuberosity proves impossible at surgery.
26.1.5.3 Partial Ruptures
Partial rupture of the biceps tendon is a rare occurrence and few cases are described in the literature. The diagnosis in these cases is more difficult, as patients complain about vague symptoms and also clinical signs are less clear. Patients often describe a clinical history of vague pain in the antecubital fossa and when a loss of strength during supination and flexion is present, it is less evident than in patients with a total lesion. In these cases, performing an MRI is more useful, as it allows the extension of the lesion to be defined and in many cases the collateral aspects of tendonitis, or tenosynovitis, or bursitis to be shown.
The first treatment in these cases is the control of pain using anti-inflammatory drugs, which can be associated with a physiotherapy protocol aimed at stretching the anterior structures of the elbow. In the case of persistent pain and functional limitations, surgical treatment is warranted. The authors who described this type of lesion suggest transforming the partial lesion into a complete lesion and to reinsert the tendon at its anatomical site [19–23].
26.1.5.4 Chronic Ruptures
When the lesion dates back to 6–8 weeks or more, then it should be defined as chronic. These lesions are the most difficult to treat, mainly because of the muscular retraction. An intact lacertus fibrosus provides the conditions for the possibility of reinserting the biceps tendon into the radius, because if it breaks, proximal tendon retraction, soft-tissue adhesions, tendon shortening and resorption preclude reconstruction with the native tendon. The first suggested options were conservative treatment [11–24] and suture to the brachialis muscle [25–29], with results similar to those formerly described; namely, a partial loss of flexion strength and a more consistent loss of supination strength. Sotereanos et al. [30] tried to repair chronic lesions in one surgical step, separating the tendon from soft-tissue adhesions as the first step, then sectioning the lacertus fibrosus and lengthening the tendon by making radial micro-incisions when traction alone was ineffective. Unfortunately, it was not possible to take the tendon back to the radial tuberosity in a number of cases and in these patients a graft was employed. This extensively studied technique can include the use of fascia lata, or the ligament advanced reinforcement system (LARS), or semitendinosus, or homologous tendons, and none of the types of graft proved mechanically superior to the others.
26.1.5.5 Surgical Technique
The choice of the surgical approach for a lesion of the distal tendon of the biceps brachii is still a source of controversy among surgeons, because there is no scientific evidence of the superiority of one technique over the other. The single incision with anterior approach is historically associated with a higher chance of neurological lesions, probably the consequence of a larger dissection and the need for wider retractors to visualise the tendon and to reinsert it on its anatomical footprint. With the aim of avoiding these complications, Boyd and Anderson developed the two-incision technique, limiting the anterior tissue dissection. However, its safety was initially impaired by an increased chance of radio-ulnar synostoses and injuries of the posterior interosseous nerve.
Over the years these two techniques have been improved. Morrey et al. [31] refined the two-incision approach, improving the posterior muscle splitting to avoid elevating the ulnar periosteum and therefore the risk of radio-ulnar synostoses. The improvements in the one-incision approach have been related to the introduction of fixation systems (anchors, endobutton, interference screws), which allowed the anterior exposure to be limited.
Regional anaesthesia is generally preferred, unless the anaesthesiologist or the patient prefers otherwise. The patient is placed supine on the surgical table with the upper limb in about 90° abduction over a hand surgery stand in supination. The surgeon and the assistant are on the opposite sides of the limb, while the scrub nurse is in front of the stand on the same side of the body as the surgeons. A tourniquet is placed at the upper arm (it is advisable to exsanguinate the limb only after identifying and isolating the biceps tendon). After preparing the skin the surgical field is set up.
Tendon Identification and Evaluation of the Lesion
The first incision described was shaped like an italic S centered on the cubital crease, with isolation of the main vascular and nervous trunks and anatomical dissection down to the radial tuberosity where the biceps tendon had to be reinserted. Over the years, the need for more limited surgical aggressiveness has led to the development of less invasive techniques.
The anterior incision only needs to be a few centimetres long (Fig. 26.2) The anterior cubital aspect has several transverse skin folds that become evident with elbow flexion. If a transverse incision is selected, following one of these folds will allow a better cosmetic result. This corresponds to the central part of the italic S incision. The choice of the level of the incision is important. If it is more proximal it allows better exposure of the biceps at the myotendinous junction, but it impairs exposure of the radial tuberosity. It is therefore preferable to make a more distal incision, about 2 cm from the main cubital crease. The biceps tendon can be identified by elbow flexion and subcutaneous tissue dissection; at the same time, by elbow extension, it is possible to expose the proximal radius without excessive soft tissue traction by the retractors. It is always possible, if needed, to enlarge the approach with a proximal or distal longitudinal extension of the incision.
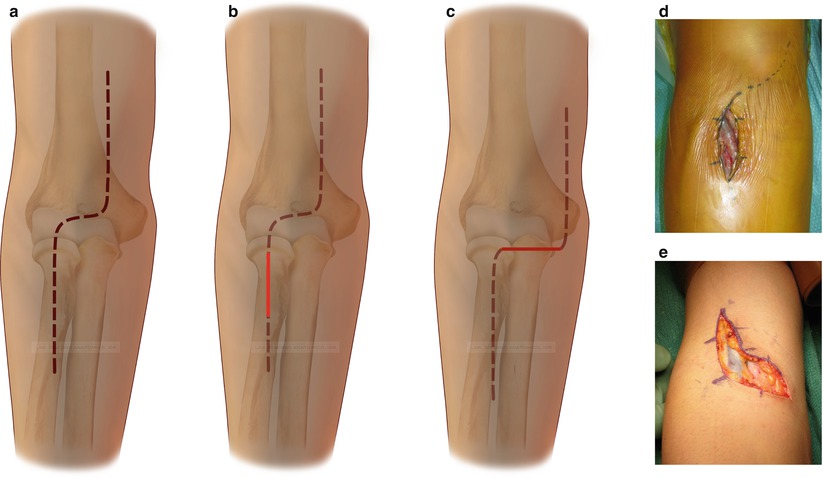
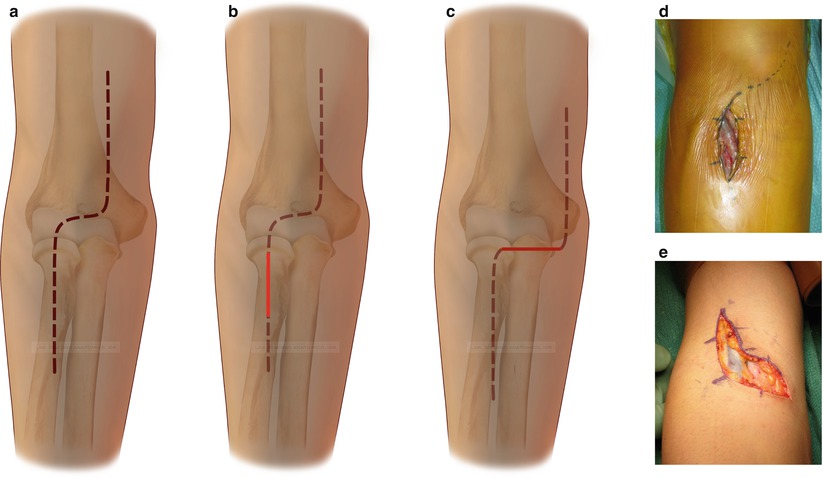
Fig. 26.2
Surgical approaches. Extended italic S incision (a) and less invasive incisions, longitudinal (b) and transverse (c). If needed, both of these incisions can be extended proximally or distally (d, e) (School of anatomic drawing, University of Bologna, Rizzoli Orthopaedic Institute)
In our experience we have changed the line of incision, from the formerly described transverse line to a 3- to 4-cm longitudinal incision centred over the radial head. Elbow flexion and the use of retractors allows the same view as permitted by the transverse incision for tendon identification, while the anatomical dissection for exposure of the radial tuberosity proves more simple and safe, although it is more difficult in muscular and tall patients. It is possible, in any case, to enlarge the exposure by a proximal extension of the incision following the line of the italic S (Fig. 26.2).
In the subcutaneous layer the superficial cubital veins are situated. Whenever possible, these veins are isolated and respected; however, if they are an obstacle for surgical exposure they have to be ligated, as their size does not allow simple cauterisation. The cephalic vein usually lies over the lateral cutaneous nerve of the forearm. It is advisable to identify this nerve, isolating it using a vessel loop (Fig. 26.3) and placing it in the lateral part of the surgical field. It is now possible to safely pay attention to the search for and exploration of the biceps tendon.
Fig. 26.3
Exposure of the proximal radius. The cephalic vein is moved laterally; the superficial branch of the radial nerve is identified, protected and moved laterally. The recurrent vessels have to be isolated and ligated before approaching the radial tuberosity in the depth of the field (School of Anatomical Drawing, University of Bologna, Rizzoli Orthopaedic Institute)
Multiple conditions may occur. The tendon may only be partially detached from the tuberosity. In this case the medial lacertus fibrosus is intact and the tendon lies in its anatomical site inside its sheath, although it has lost its tension. It is easy to follow it distally and to test its resistance to traction using a hook. In most cases a mild traction makes the lesion complete and the tendon comes out. If on the contrary it resists traction, the option to abort surgery can be considered (after careful examination of the myotendinous junction to rule out a proximal rupture). However, if the tendon is loose, it is better to expose the tuberosity and transform the partial lesion into a total lesion by detaching the few residual fibres.
When the lesion is complete, the sheath is empty, and inside there is serous haematic fluid, which is more abundant if the injury is recent. The tendon stump can usually be found proximally, underneath the biceps muscle belly. When the lacertus fibrosus is also broken, the tendon can be found folded in itself and migrated proximally by several centimetres. In these cases, especially if surgery is performed 15–20 days after the injury, it is wise to extend the incision proximally and perform a very careful dissection of the tendon from the surrounding scar tissue, which can show the same colour and consistency as the tendon. Once the tendon is isolated, its distal portion is taken out of the surgical wound and the degenerated fibres at the extremity are removed.
Tendon Repair at the Radial Tuberosity
The surgical techniques can be separated into two main groups, the single anterior approach and the double anterior and posterior approach.
Single Anterior Approach Technique
The radial tuberosity should be carefully exposed. The literature reports bony anchors, or endobutton, or interference screws as fixation devices alternative to the transosseous suture. A transosseous repair with a bony trough, as described for the double incision technique, is not easy to perform with an anterior single approach and is less strong in cadaver tests. The mechanically stronger methods are the endobutton, which unfortunately is associated with a risk of damage to the posterior interosseous nerve, and fixation by an interference screw, which carries the risk of late bony resorption of the proximal radius. Apart from evaluation of which is the mechanically stronger method, none of the techniques has shown clinical superiority over the others. We therefore selected the anterior single approach technique to use bony anchors, as we believe that they represent the best compromise among mechanical strength, surgical reproducibility and risk of complications.
After the lateral cutaneous nerve of the forearm has been identified and moved laterally, the deep dissection is carried out. The superficial veins are ligated or cauterised and the brachioradialis and round pronator muscle bellies are retracted laterally and medially. The recurrent vessels are so exposed that they correspond to the level of the radial tuberosity and have to be carefully dissected and ligated to gain access to the bone (Fig. 26.3).
Forceful forearm supination allows access to the tuberosity, from which the tendon fibre remnants and scar tissue need to be cleaned. The working field is deep; a lever can be used on the medial side, while attention should be paid to the lateral side, where the posterior interosseous nerve lies inside the supinator muscle close to the bone. It is therefore prudent to only place a retractor on this side, which applies less pressure than a lever (Fig. 26.4).
Fig. 26.4
Exposure of the proximal radius, axial section (School of Anatomical Drawing, University of Bologna, Rizzoli Orthopaedic Institute)
The bony surface is roughened to promote tendon-to-bone healing. The holes for the anchors have to be carefully prepared so that they are inserted correctly and they are guaranteed to hold. It is our practice to drill both cortices using a 1.5-mm drill; the proximal hole is then enlarged by a 2.5-mm drill to insert a 5-mm anchor (Fig. 26.5). To reduce the risk of cortical fracture, a 10 cm gap is left between the first and the second anchor. Our preference is to use threaded anchors, as they can be easily removed if needed. Careful lavage is performed after each step to remove as much of the bony debris as possible, and with the same intent we advise using drill bits rather than smooth bits.
Fig. 26.5
Surgical technique of anchor introduction. Drilling both cortices is useful to allow the correct introduction of the tip of the anchor. The proximal hole should be enlarged to prevent cortical fractures, which may compromise the pull-out strength of the anchors (School of Anatomical Drawing, University of Bologna, Rizzoli Orthopaedic Institute)
The tendon is grasped by the sutures of the anchors (Fig. 26.6). The proximal anchor is connected to the medial part and the distal anchor to the lateral part of the tendon. Each anchor bears two sutures. By one head, a Krackow-type suture is placed over a 4-cm length of the tendon, while both heads of the second suture are passed in a mattress configuration into the distal head of the tendon. With this method the first suture allows a stronger hold on the tendon, while the second suture increases the contact surface between the tendon and the bony surface.
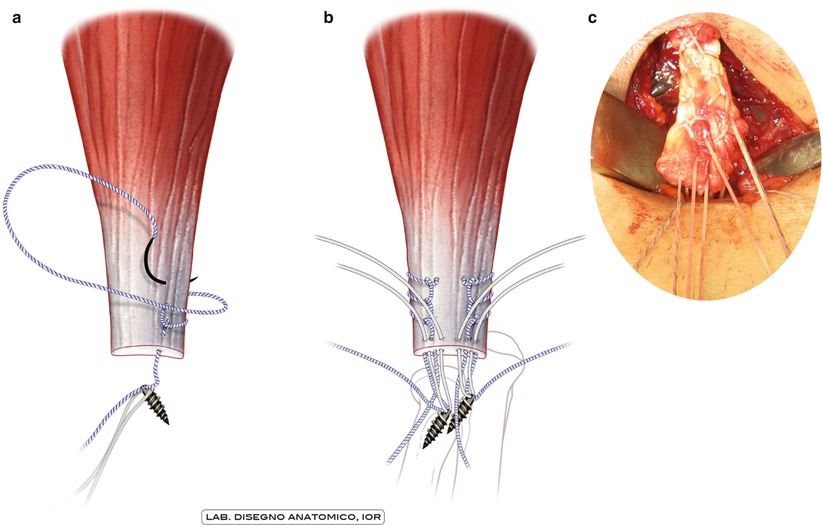
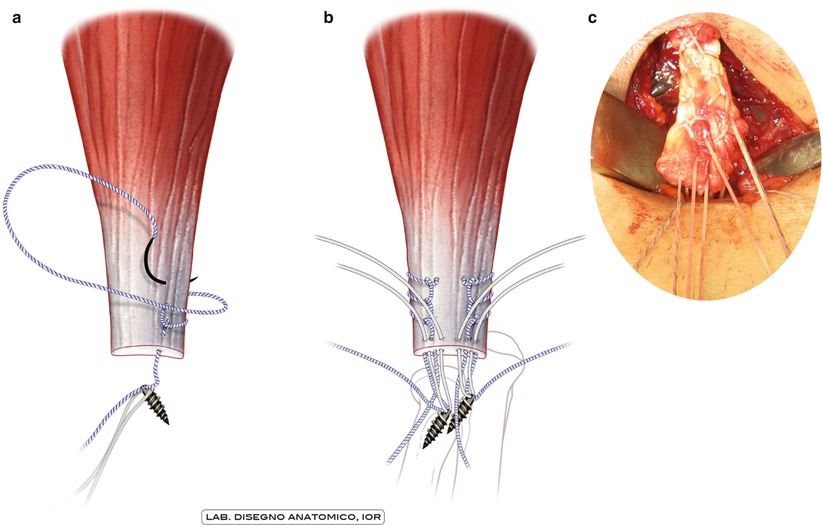
Fig. 26.6
Drawings (a, b) and surgical detail (c) of the passage of the anchor sutures inside the tendon (School of Anatomical Drawing, University of Bologna, Rizzoli Orthopaedic Institute)
We have no experience of repair using the endobutton (Fig. 26.7), except on cadavers. This technique has proved to be biomechanically stronger, but in surgical practice it has been reported to be more difficult and dangerous for the posterior interosseous nerve.
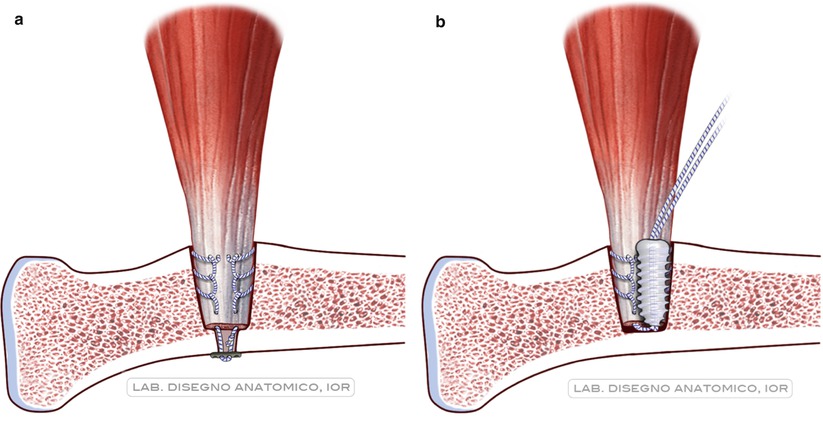
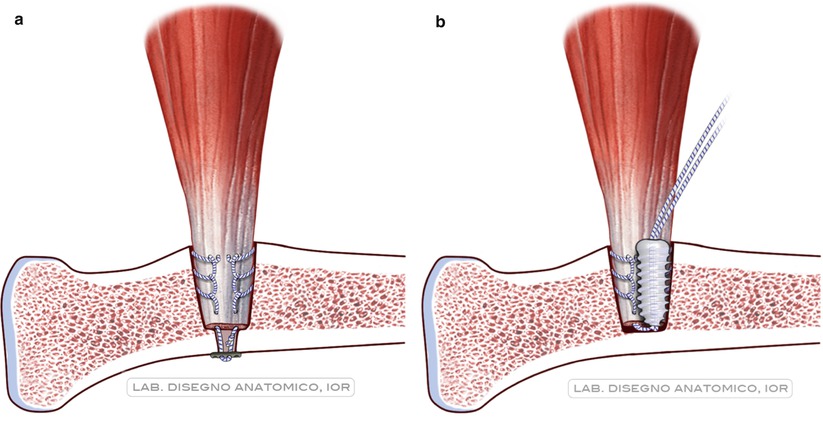
Fig. 26.7
Tendon repair using the endobutton system (a) and by the interference screw (b) (School of Anatomical Drawing, University of Bologna, Rizzoli Orthopaedic Institute)
We used interference screws (Fig. 26.7) in only a few cases. The literature reports cases of osteolysis around resorbable screws and for this reason we chose polyetheretherketone (PEEK) screws. Even in this case the surgical technique must be meticulous. The hole for the screw has to be large enough, but if the grip is loosened, it becomes difficult to switch to another fixation technique.
Double Anterior and Posterior Approach Technique
This is a reliable and low-cost technique that has not been modified since its original description by the Sotereanos et al. [30].
The suggested anterior incision is transverse and proximal. Once the tendon is retrieved as formerly described, it has to be cleaned and then grasped by two high-resistance sutures with Krackow-type stitches over a 4-cm length. An extensive anterior dissection is not necessary; the peritoneum should be smoothly followed until the radial tuberosity. A curved haemostat should be passed very closely to the radius while the forearm is placed in flexion and complete pronation. The haemostat is advanced until it reaches the subcutaneous layer posteriorly (Fig. 26.8). The author draws attention to the tool direction, which should follow the posterior radial cortex to limit the possible muscular injury, predisposing to heterotopic ossifications.
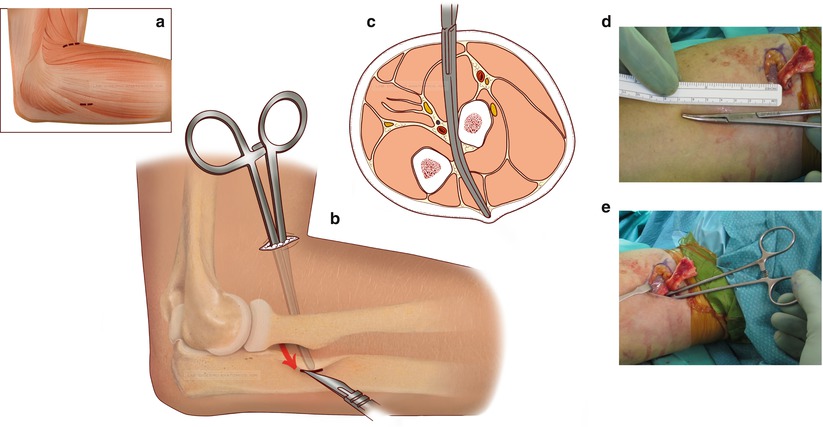
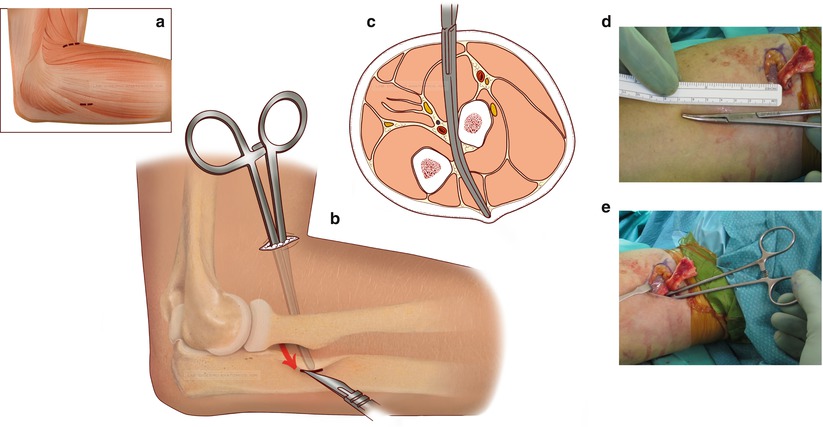
Fig. 26.8




Drawings (a–c) and surgical details (d, e) of the blind passage of the curved haemostat (The drawings reproduce the author’s [30]) original pictures, by the School of Anatomical Drawing, University of Bologna, Rizzoli Orthopaedic Institute)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






