20 Best Rehabilitation Practices
Overview
Hip fractures are potentially catastrophic events that occur frequently in the lives of elderly persons. These injuries are among the leading causes of disability and mortality in elderly patients and represent a major burden on the health care system.1–3 Investigators have also shown that these patients have a sustained decline in physical function, with fewer than 30% of patients regaining their prefracture level of functioning.4–6 Up to one third of the patients with hip fracture can become dependent and risk institutionalization.7,8 Long-term functional outcomes have significant direct and indirect effects on, and costs for, not only patients with hip fracture, but their family or caregivers as well.
In addition, the overall incidence of hip fracture has increased rapidly because of longer life expectancy and a higher age-specific incidence of this injury.9 This increase in numbers of hip fractures coupled with the long-term functional decline mentioned earlier has provided the impetus for examining the efficiency of treatment following hip fracture across the continuum of care. Programs that focus on continuity of care, adopt an interdisciplinary approach, and accelerate rehabilitation have reduced the cost of care after hip fracture.10
Integrated care pathways have been instrumental in improving the standard of care and outcomes for patients with hip fracture who have complex issues (e.g., concomitant medical problems, frailty), although this approach does require additional resources.11 This integrated care pathways approach was used to implement a model of care through the Total Joint Network (www.totaljointnetwork.org), which was a consortium of 35 health care organizations in the greater Toronto area that were working collaboratively to improve care of patients with hip fractures.12 As a result of improved outcomes demonstrated in this pilot project, the Ontario provincial government is now reviewing the funding model to see whether implementation and sustainability are feasible. Analysis of best practices in rehabilitation along with evaluation of existing services can provide the framework for instituting a care pathway in any setting. The key to success is collaboration among the various components of continuum of care within the health care system, with the goals of improving system efficiency and patient care. This chapter explores best practice guidelines for the management of medical issues in the postacute phase of hip fracture and the principles involved in organization of rehabilitation services.
Organizing Rehabilitation Services
Definition of Rehabilitation
Rehabilitation is a goal-oriented and time-limited process aimed at enabling an impaired person to reach an optimum mental, physical, or social functional level and thus providing that person with the tools to change her or his own life.13 Interprofessional care is a way of practice that is based on collaboration among health providers (HCPs) involved in the care of patients. This team usually consists of a rehabilitation physician, a rehabilitation nurse, a social worker (SW), an occupational therapist (OT), a physical therapist (PT), and a speech therapist. The team may also include a pharmacist, a psychologist, a recreational therapist, and OT or PT aides. To maximize rehabilitation potential, interprofessional care is essential to provide the various skills needed to manage complex issues associated with medical comorbidities, the risk of medical and surgical complications, and premorbid functional limitations.14 In today’s cost-cutting environment, caution must be taken to prevent short-term cost-saving measures from compromising long-term outcomes for elderly patients with hip fracture.15
Rehabilitation Setting
Rehabilitation can take place in different settings and usually begins postoperatively in the acute care setting. A systematic review by Chudyk et al16 of hip fracture rehabilitation in the acute care showed that management by a geriatrician, high-frequency physical therapy (1.5 hours a day, 5 days a week), and additional occupational therapy (1 hour a day, 5 days a week) were associated with increased ambulatory recovery. Inpatient rehabilitation typically takes place either in a free-standing rehabilitation hospital (FSRH), an acute care hospital (ACH) with an inpatient rehabilitation unit (ACHRU), or a skilled nursing facility (SNF), such as a long-term care (LTC) facility, a complex continuing care (CCC) facility, or a nursing home (NH). High-intensity therapy for 3 hours a day, 5 to 7 days a week is provided by an interprofessional team in the FSRH or ACHRU, whereas the SNFs usually have lower-intensity therapy for 1 hour a day, 3 days a week. Physician involvement and HCP expertise are often more limited in the less-intensive locations. Intensive rehabilitation in an inpatient rehabilitation setting results in superior functional outcomes and a shorter length of stay (LOS) as compared with a SNF17or a local hospital ward.18
Bridging the Health Care Continuum
Direct Home with Outpatient Care
Selected patients who are often younger and less frail are more likely to be discharged home after therapy in the ACH. In one study, the absence of postoperative complications and a regimen of more than one physical therapy treatment per day increased the odds of early independence in mobility.19 Exercise and gait training continue in the home setting, as provided by the PT in the community.
Free-standing Rehabilitation Hospital or Acute Care Hospital with an Inpatient Rehabilitation Unit Inpatient Rehabilitation Transfers
Rehabilitation provides the crucial services needed for enabling functional independence in these patients. Post-ACH rehabilitation services can occur in different settings, as mentioned previously. Skilled assessment using set specific criteria can help in deciding which types of patients are best suited for which setting, so that optimal outcomes are achieved at reasonable cost. The ideal goal is to provide the right amount of rehabilitation to each patient at the right time in the right setting.20 Two concepts important in this transition are as follows:
Inpatient Rehabilitation Services: Guidelines for Common Medical Issues Encountered During Rehabilitation
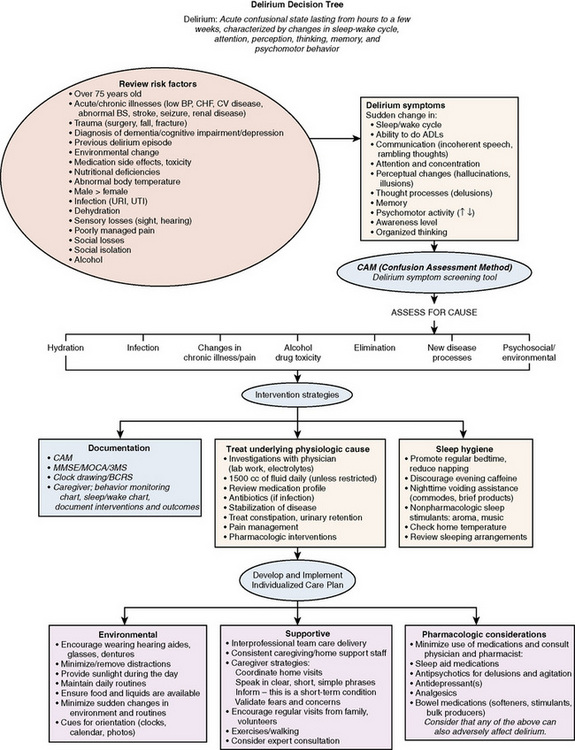
Delirium
Delirium (or acute confusional state) (Fig. 20-1) affects 13% to 61% of patients after hip fracture and is an independent predictor of poor functional outcome.21,22 In one study, delirium on admission was associated with poorer functioning in physical, cognitive, and affective domains at 6 months after fracture.22 Early identification and management of delirium are essential for enabling participation in therapy. The confusion assessment method (CAM) is an easy and quick instrument to detect delirium with high specificity and sensitivity.23 The CAM uses the following features for diagnosis: (1) acute and fluctuating changes in mental status, (2) inattention, (3) disorganized or incoherent thinking, and (4) altered level of consciousness. A CAM score is considered positive if the patient has any of the following combinations: 1, 2, and 3; 1, 2, or 4; or 1, 2, 3, and 4. Agitation is often associated with delirium; however, the clinical team also needs to be aware of hypodelirium states (withdrawn behavior, low energy), which are also manifestations of delirium.
Both nursing and medical interventions can reduce postoperative delirium and improve outcome following hip fracture.24 Medical interventions commonly include the following:
Nursing interventions are based on a consistent structured care and rehabilitation schedule in an appropriately designed system to improve functioning.24 These interventions include the following:
Medical Comorbidities
Medical assessment needs to be continued in the rehabilita- tion setting because the aggravation of any comorbidities can prolong the LOS and can cause further deconditioning in the already frail individual that may lead to adverse functional outcomes. Bernardini et al26 reported that patients who were more than 65 years old who were admitted to a geriatric rehabilitation unit after proximal hip fracture had complex, multiple, interacting disorders, and 78% of these patients had significant comorbidities. Chest infection and heart failure were the most common postoperative complications requiring specialist assessment because these conditions were potentially fatal.27
The reported postoperative incidence of pressure sores ranges from 10% to 40%. Foam and alternating-pressure mattresses reduce the incidence of pressure sore development compared with usual care, which includes manual repositioning of patients.28
Cognitive Impairment and Dementia
Patients with underlying dementia are more likely to have delirium,21 with a higher risk for long-term institutionalization and mortality after hip fractures.8 Patients with dementia were previously denied access to intensive rehabilitation programs in some countries,29 because of the potential risk of poor outcomes. Grade A, level 1 evidence indicates that patients with mild or moderate dementia will benefit from a multidisciplinary rehabilitation team to regain function.30,31 Outcomes comparable to those reported in patients without cognitive impairment (CI) can be achieved in patients with CI in the setting of a dedicated hip fracture service.32,33 Heruti et al34 showed that the absolute motor gains made were independent of patients’ cognitive status. Intensive postfracture rehabilitation in the early phase of recovery promotes functional independence and return to the community for older patients at risk of NH placement.12,35
Diagnosis of Dementia
Dementia is diagnosed when acquired deficits are sufficient to interfere with social or occupational functioning in a person without depression or clouding of consciousness.36 When the patient has objective evidence of memory loss or a decline in other areas of cognition on mental status testing, function in terms of daily activities should be assessed. Collateral history from a caregiver should be used to corroborate this assessment. Investigations are done to look for reversible conditions such as infections and metabolic abnormalities that may aggravate or even cause cognitive decline. Substance abuse, adverse drug effects, and depression need to be excluded.
The term cognitive impaired, not demented is used when deficits do not meet the criteria for dementia.37 Follow-up for this group is essential because 5% to 6% of these patients will progress to dementia. Caution should be used when diagnosing dementia in this postacute period. Allowing for the potential delirium to settle and medical issues to stabilize when the individual is back in his or her own preinjury environment or in a more stable nonhospital environment will provide a more realistic picture of the elderly patient.
Management of Dementia
Staff members in the rehabilitation setting should have skills, attitudes, and knowledge to encourage therapy and functional activities in patients with dementia. Communication difficulties with understanding and following instructions can be compounded by deficits in areas of hearing and vision. Problems with short-term memory make it difficult to remember exercises and instructions with regard to functional activities and use of walking aids. Repetition and cueing are essential. Patients and family members need to be educated about the disease and how to cope with its manifestations. This education includes appropriate modifications to the home environment and learning to communicate and interact with the patient. Caregiver coping strategies should be encouraged, to reduce stress.38
When the patient experiences anxiety or agitation during the rehabilitation stay and is unable to articulate the cause, careful assessments are required to determine the rationale behind the behaviors. More than likely, the patient is responding to an unmet need (i.e., pain, hunger, fear, constipation). Disruptive behaviors are observable actions that have the potential for or are perceived as endangering the patient or staff, causing stress or fear, or being socially unacceptable.39 Consequences of behavior should be recorded, and the act of documenting these can itself reduce the number of incidents because the patient learns to recognize and anticipate the consequences and thus avoids provocation.39
Nonpharmacologic interventions are recommended and involve interventions to fulfill the unmet needs of the patient. Such interventions may involve environmental modifications, relational approaches, and specific behavioral techniques. If the patient continues to be agitated, pharmacologic interventions may be tried. Newer atypical neuroleptics such as risperidone, olanzapine, and quetiapine are preferred over the traditional neuroleptics because of the high incidence of extrapy-ramidal side effects. A trial may be given with cognitive-enhancing drugs such as donepezil and rivastigmine if a picture of dementia appears likely with corroborating prefracture evidence. Follow-up should be arranged once in 3 months to assess the patient’s response.38
Pain Management
Inadequate postoperative pain control is associated with longer hospital LOS, missed or shortened physical therapy sessions, delayed ambulation following surgery, and impaired locomotion at 6 months following fracture.40 Postoperative pain and pain management strategies are both independently associated with the development of postoperative delirium.41 In one study, patients who received oral opioid analgesics as their primary method of postoperative pain management were at decreased risk for developing delirium compared with those receiving patient-controlled analgesia (PCA). Opioid analgesics administered orally may result in a lower blood level of the drug because of the first-pass effect compared with intravenously administered narcotics, which may directly cross the blood-brain barrier.41
Arinzon et al42 showed that pain perception on admission to geriatric rehabilitation inversely correlated with family support, function before fracture, and cognitive status on admission and correlated positively with depressed mood. The average visual analog scale (VAS) score on admission to the rehabilitation setting in this study was 7.38 ± 1.20 and on discharge was 3.67 ± 1.18. Pain has been shown to be an independent predictor of FIM on discharge. With every increase in one point of VAS, the LOS increased by 4.76 days, and the FIM on discharge decreased by 6.73.42
Undertreatment of elderly patients is exemplified by a 1998 article by Bernabei et al,43 who demonstrated that even in patients with cancer who had CI, physicians tended to undertreat chronic pain. In this study, one fourth of the patients received no analgesics, and almost half of these patients were not given any opioids, compared with individuals with no CI who received medications for pain.43
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree