Chapter 64 Basic Surgical Technique and Postoperative Care
Preoperative Planning and Preparation
Arrangement and Routine in the Operating Room
Because surgical results depend considerably on the skill, judgment, and precise work of the surgeon, it is important to keep intraoperative distractions to a minimum. Disorganization, fatigue, and uncertainty diminish the efficiency of the operating team. It is important for the surgeon to establish a standard routine that is followed regularly (Fig. 64-1). Each assistant can then depend on this routine. The activities of the assistants in following this routine should not be disrupted by the surgeon with irregular, unexpected, or inconsistent demands. A standard routine makes it possible for assistants to know what is expected of them at each step in the operation and allows them to perform without hesitation, delay, or wasted motion.
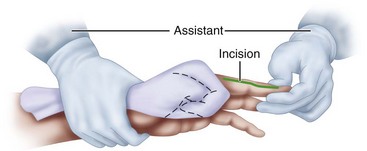
Seated opposite the surgeon, the assistant should view the operative field from 8 to 10 cm higher than the surgeon to allow a clear line of vision without having to bend forward and obstruct the surgeon’s view. Although mechanical hand holders are available, they are not as good as a motivated and well-trained assistant. It is especially helpful for the assistant to be familiar with each procedure. Usually, the primary duty of the assistant is to hold the patient’s hand stable, secure, and motionless, retracting the fingers to provide the surgeon with the best access to the operative field (Figs. 64-2 and 64-3).
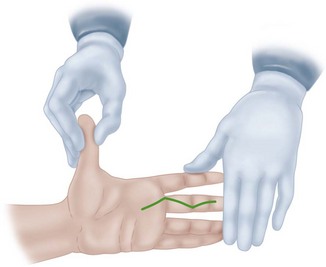
FIGURE 64-3 Ideal position for assistant to stabilize patient’s hand as surgeon makes zigzag incision.
The tray holding the basic instruments often is placed on a shelf extending from the operating table, level with the working surface. The instruments always should be arranged in the same order (Fig. 64-4). This arrangement allows the surgeon to save time by routinely reaching for instruments from the basic tray. With practice, this can be done without the surgeon looking at the instruments.
Choice of Anesthesia
Drugs used for local and regional anesthesia should become effective within a few minutes after injection, should cause minimal local irritation, and should have low systemic toxicity. Lidocaine seems to fulfill these requirements. Mepivacaine (Carbocaine) is longer acting but may be slower in onset. Many surgeons prefer bupivacaine (Marcaine) because it is effective for 8 hours or longer. It can be used for axillary brachial block to avoid the use of a general anesthetic. Each of these agents has a toxicity level based on milligrams per kilogram of body weight, and this should be calculated before administration (Table 64-1).
TABLE 64-1 Maximal Doses of Local Anesthetics for Brachial Plexus Blocks*
| ANESTHETIC | MAXIMAL RECOMMENDED DOSE |
|---|---|
| Bupivacaine | 2.5 mg/kg |
| Bupivacaine with epinephrine | 3.0 mg/kg |
| Levobupivacaine | 2.0 mg/kg |
| Levobupivacaine with epinephrine | 3.0 mg/kg |
| Ropivacaine | 2.0 mg/kg |
| Ropivacaine with epinephrine | 3.0 mg/kg |
*These amounts should be used as a guideline only; practitioners should use their clinical judgment when administering local anesthetics.
Modified from Bruce BG, Green A, Blaine TA, Wesner LV: Brachial plexus blocks for upper extremity orthopaedic surgery, J AAOS 20:38, 2012.
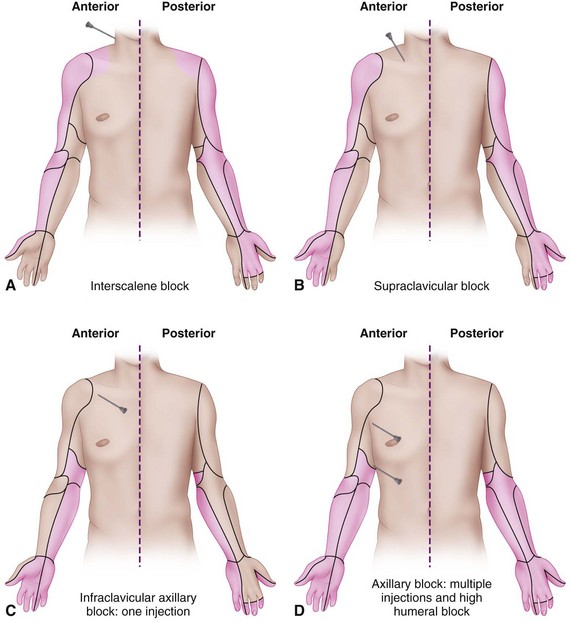
Brachial Plexus Blocks
The traditional approaches for administering anesthesia to the major components of the brachial plexus include the axillary, interscalene, and supraclavicular and infraclavicular routes (Fig. 64-5). The axillary and interscalene approaches we use most commonly probably are safer than the supraclavicular route, which carries the risk of a low incidence (1% to 5%) of pneumothorax. Infraclavicular and supraclavicular blocks are more commonly done now with ultrasound guidance. The interscalene block covers the supraclavicular nerves emanating from the third and fourth cervical roots and is ideal for shoulder surgery. Interscalene blocks can also be used for elbow surgery. Supraclavicular blocks are useful for surgery in the upper arm distal to the shoulder, whereas infraclavicular blocks can provide regional anesthesia for surgery of the elbow, forearm, wrist, and hand. An axillary block provides anesthesia similar to that of an infraclavicular block. Access to the axillary space requires the patient to abduct the arm 90 degrees, which may be difficult for those with trauma or contractures. Needle placement for brachial plexus blocks was traditionally based on anatomic landmarks and nerve localization with a nerve stimulator, but more recent approaches use an ultrasound approach. A meta-analysis of 13 studies comparing neurostimulation with ultrasound-guided blocks found that ultrasound-guided blocks were more likely to be successful, took less time, had a faster onset, and decreased the risk of vascular puncture. A study of the multiple-injection technique for axillary block showed that ultrasound guidance resulted in fewer needle passes, a shorter time to onset of anesthesia, and less procedure-related pain than nerve stimulation techniques. Limitations of ultrasound include availability, a limited plane of view, and highly operator-dependent image quality.
Short- and long-acting local anesthetic agents can be used for brachial plexus blocks. The dose depends on the agent used, the technique used, and the preference of the administering physician. Although the amount of anesthetic used is not standardized, maximal amounts have been recommended (see Table 64-1).
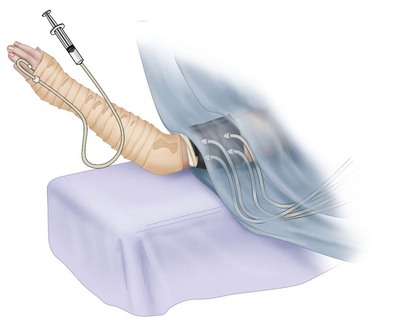
Intravenous Regional Anesthesia
The intravenous regional anesthesia technique using a double tourniquet (Bier) is useful, especially for procedures of relatively short duration (60 to 90 minutes). A specially designed double tourniquet is used. The patient should be satisfactorily premedicated, and intravenous infusion should be in place in the contralateral arm. The usual anesthetic agent is lidocaine. In most situations, 30 to 60 mL of 0.5% lidocaine provides sufficient and safe anesthesia. The dosage used should take the patient’s age and body weight into consideration. Satisfactory anesthesia can be obtained in a short time. The tourniquet is left inflated for a minimum of 30 minutes after injection of the anesthetic agent into the extremity. In the usual situation, the limb is exsanguinated; the proximal tourniquet is inflated to a level 100 mm Hg greater than the systolic pressure (usually 250 to 300 mm Hg); and, using sterile technique, the anesthesiologist intravenously introduces the previously determined volume of anesthetic agent (Fig. 64-6). As the more proximal tourniquet becomes uncomfortable, the distal tourniquet is inflated and the proximal tourniquet is deflated. Reported reactions during intravenous regional anesthesia include cardiac arrhythmias (bradycardia and cardiac arrest), unconsciousness, vertigo, and nystagmus.
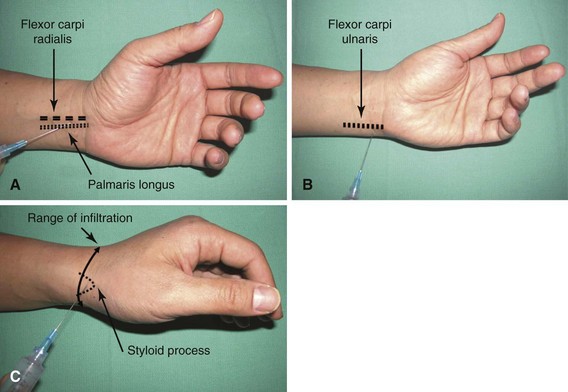
Peripheral Nerve Blocks
The median, radial, and ulnar nerves can be blocked at the elbow and wrist, and these blocks are extremely helpful for brief procedures (Fig. 64-7). A tourniquet may not be required or may be used only for a short period (usually ≤ 30 minutes). It is essential to know the location of the respective nerves before attempting regional blocks. Blocks at the wrist can be especially useful for procedures such as tenolyses and capsulotomies because motion of the fingers can be observed during surgery. The patient can be kept comfortable, and a tourniquet can be used longer than 30 minutes if the patient is adequately sedated.
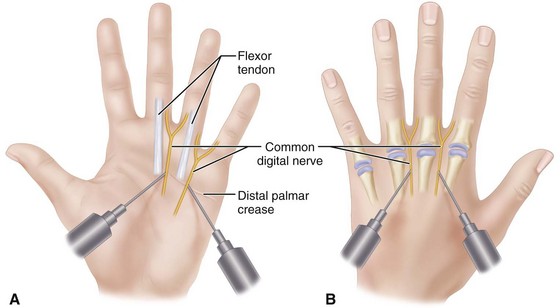
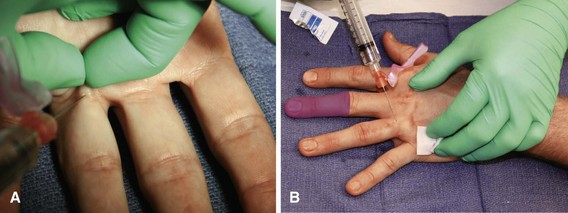
Digital Nerve Blocks
Digital nerve blocks provide excellent anesthesia for procedures on the fingers (Fig. 64-8). Usually, perineural injection around the digital nerves proximal to the finger web spaces is a safer technique than injection of the nerves at the base of the fingers. Because ischemia may develop after injection of an anesthetic agent in a circle around the base of the finger, this technique should be avoided. Digital blocks using a transthecal (flexor sheath) approach have shown no advantage compared with the traditional digital block technique (Fig. 64-9). We rarely use epinephrine in the local anesthetic agent in the digits, although it can be used safely.
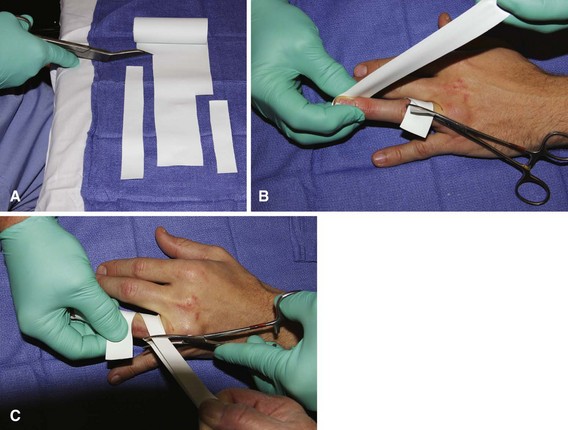
If hemostasis is required, traditionally a Penrose drain or a French rubber catheter applied around the finger has provided satisfactory and safe ischemia. Commercially available finger tourniquets and the finger of a rubber glove cut to allow it to be rolled onto the finger as a tourniquet also are effective tools. Pressures achieved beneath these tourniquets cannot be determined accurately; caution is advised. At times, especially in the elderly and patients with vascular disorders in the fingers (e.g., Raynaud disease, atherosclerosis, diabetes), vascular insufficiency may develop in the digit, and care should be taken when using digital tourniquets in these patients (Fig. 64-10).
Preparation and Draping for Elective Surgery
Regardless of the procedure, the method of preparing and draping the upper extremity and hand should be the same. This helps to standardize the routine and allows movement about the operative field while minimizing the risk of bacterial contamination. The preparation of other areas for graft donor sites varies depending on the requirements of the procedure. If skin, tendon, bone, nerve, or other grafts are required, the patient should be positioned to allow easy access to the specific areas. Care should be taken to pad and protect neurovascular structures. The electrocautery grounding pads should be attached in a safe and secure manner. Usually, the hand and forearm are scrubbed before the time of the surgery. The hair is removed with electric clippers from the areas where skin incisions will be made on the hand, forearm, and elsewhere as needed; this often is done before the patient is transported to the operating room. A well-padded tourniquet is applied to the arm or the forearm, depending on the surgeon’s preference; however, it is not inflated until all preparations have been completed (unless a Bier block is being used). After the patient has been satisfactorily anesthetized, the hand and forearm are scrubbed by an assistant while the surgeon scrubs his or her own hands. The surgeon puts on gloves and prepares the skin with an antiseptic solution of choice. Iodophor soaps and skin preparation solutions and combinations of chlorhexidine and alcohol have been found to be effective (Table 64-2). Wetting the padding beneath the tourniquet with these solutions should be avoided to minimize skin reactions. A waterproof sheet is placed on the well-padded hand surgery table, followed by a sterile drape-sheet. Combinations of sterile towels and sheets are applied, leaving exposed the upper extremity and hand and other areas that may require access during the operation. The gloves used in preparation of the surgical field are removed, and the surgeon dons a gown and gloves and sits down, usually on the axillary side of the forearm. The operating lights are adjusted, and the skin incisions are outlined.
TABLE 64-2 Antiseptic Solutions
| Alcohol | Good immediate skin disinfectant, but dries quickly and has less long-term effect |
| 95% alcohol better than 75% because of dilution by moist skin | |
| Hexachlorophene (pHisoHex) | Forms a film that retains bacteriostatic properties |
| Easily washed off | |
| Requires multiple applications to be effective | |
| May be toxic in infants | |
| Effective against gram-positive organisms; less effective against gram-negative organisms | |
| Iodine | Side effects |
| Alcoholic (tincture) | Frequent skin irritation (can be lessened by adding iodine) |
| Aqueous (Lugol’s solution) | True allergic reactions |
| Iodophors (povidone-iodine [Betadine]) | Advantages over iodine |
| Iodine and polyvinyl pyrrolidine or povidone | Slower release of iodine |
| Fewer skin reactions | |
| Effective against gram-negative and gram-positive organisms | |
| Chlorhexidine (Hibiclens) 70% alcoholic solution | Some studies have shown it superior to Betadine and pHisoHex |
| Repeated washings may have a cumulative effect |
Adapted from Green DP: General principles. In Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, editors: Green’s operative hand surgery, ed 6. Philadelphia, 2011, Elsevier.