2.1 Barriers to disease and susceptibility
Chapter 2.1a Health and susceptibility: what makes us vulnerable to disease?
Susceptibility as vulnerability to disease
Chapter 1.1e introduced the basic causes of disease from the perspective of both conventional and more holistic approaches to medicine, and looked at their similarities and differences.
The conventional view of barriers to disease
Conventional medicine recognises mechanical and immune barriers to disease. Mechanical barriers are those that confer protection as a result of the physical structure of the barrier (e.g. the keratinised squamous epithelium of the skin). Immune barriers are those that protect by a complex interaction of the immune cells and proteins (including antibodies) that circulate in the body fluids and can move into tissues when required. Examples of these are summarised in Table 2.1a-I.
Table 2.1a-I Examples of the barriers to disease
| Depth | Name of barrier | Type |
|---|---|---|
| Superficial | Skin, and body hair | Mechanical |
| Oily secretion of skin (sebum) | Mechanical | |
| Antibodies in sweat | Immune | |
| The structures which protect the orifices (e.g. eyelids, nostrils, urethra) | Mechanical | |
| Mucous membranes | Mechanical | |
| Mucus secreted from mucous membranes | Mechanical | |
| Antibodies in mucus and tears | Immune | |
| The cushioning of subcutaneous tissues (fat) | Mechanical | |
| The bony skeleton | Mechanical | |
| The supportive and protective nature of other types of connective tissue in all parts of the body | Mechanical | |
| The ability of wounds to heal | Mechanical | |
| The ability of blood to clot | Mechanical | |
| Deep | Immune cells and antibodies in the blood and lymph | Immune |
Table 2.1a-I summarises those parts or functions of the body that have a protective role. Most of the mechanical barriers serve as a protective method for the body literally by providing physical protection against damage. Healing of wounds and the blood-clotting mechanism may be more difficult to picture as a mechanical barrier, as a chain of physiological responses has to be set in action for them to exert their protective effect. The role of the immune system in protection is even more complex. For this reason, wound healing, blood clotting and the immune system are each discussed in more detail in the following chapters in this section.
Health and susceptibility
Table 2.1a-I lists those body parts or functions that have a specific role in protection against disease. However, overarching the protection that these specific barriers provide is the general health of the body. In fact, health in any organ or body part will in itself provide a barrier against disease. For example, a perfectly structured heart organ will be less susceptible to heart disease than one with damaged heart valves or a weakness in the heart muscle (see Q2.1a-3) .
.
Congenital susceptibility
Congenital susceptibility means that one or more of the barriers to disease are not functioning well from birth (see Q2.1a-5) . Examples of congenital disease conferring susceptibility include albinism, haemophilia and congenital heart disease. In albinism an inability to produce the skin pigment melanin leads to vulnerability to sunburn and skin cancer. In haemophilia an inability to produce sufficient blood-clotting proteins leads to vulnerability to bleeding into joints and muscles. In congenital heart disease poorly formed heart valves and gaps in the internal muscle wall of the heart lead to a vulnerability to poor heart pumping action, breathlessness and, over time, lung damage. The important congenital diseases are described in detail in Chapter 5.4c.
. Examples of congenital disease conferring susceptibility include albinism, haemophilia and congenital heart disease. In albinism an inability to produce the skin pigment melanin leads to vulnerability to sunburn and skin cancer. In haemophilia an inability to produce sufficient blood-clotting proteins leads to vulnerability to bleeding into joints and muscles. In congenital heart disease poorly formed heart valves and gaps in the internal muscle wall of the heart lead to a vulnerability to poor heart pumping action, breathlessness and, over time, lung damage. The important congenital diseases are described in detail in Chapter 5.4c.
Acquired susceptibility
Acquired susceptibility is the consequence of a weakening of the barriers to disease after birth. Any one of the conventionally accepted causes of disease (Chapter 1.1e), such as poor diet, lack of exercise, obesity and smoking, is understood to contribute to increased susceptibility before disease is seen to occur.
Preventive medicine
Disease prevention may be directed at an individual patient, in the form of personalised health education advice to a patient, screening for early signs of preventable disease, or by prescribing medication to reduce the impact of risk factors such as high blood pressure. Alternatively, changes can be instituted at a national, or even international level to prevent disease. Such changes may require political reform. The advances in sanitation in the UK made in the 19th century are an example of this sort of wide-scale ‘public health’ measure. Other examples include legislation concerning the advertising of tobacco products, and supplementation of foods with nutrients, such as folic acid in breakfast cereals (see Q2.1a-7) . Table 2.1a-II lists some more examples of approaches to the prevention of disease.
. Table 2.1a-II lists some more examples of approaches to the prevention of disease.
Table 2.1a-II Examples of preventive measures against known risk factors for disease
| Risk factor | Preventive measure |
|---|---|
| Meningitis outbreak | |
| Unprotected sex | |
| High-fat diet | |
| Sedentary lifestyle | Encouragement to exercise by providing cheap access to leisure centres, cycle tracks, etc. |
| Tendency to accidents in childhood | |
| Smoking tobacco | |
| Alcohol | Restriction on the sale of alcohol to children |
 Self-test 2.1a Health and susceptibility: what makes us vulnerable to disease?
Self-test 2.1a Health and susceptibility: what makes us vulnerable to disease?
1. Define susceptibility from the perspectives of conventional and holistic medicine.
2. What is the more popular term for what is understood as an inherited susceptibility to disease?
3. Name three types of mechanical barrier to disease, and for each one:
4. Name two risk factors that predispose to skin cancer.
5. Name two factors that are protective in road safety.
6. List four possible conventional medical approaches to the prevention of heart disease. Include in your list at least one approach that is aimed at the individual patient and at least one public health approach.
Answers
1. Conventional medicine: vulnerability to disease.
Holistic medicine: vulnerability to imbalance.
2. Poor constitution (constitutional vulnerability) is the more popular term for an inherited susceptibility to disease.
3. Possible examples include (there are many):
| Barrier | Risk factor | Disease |
|---|---|---|
| Bony skeleton | Tendency to fracture (osteoporosis) | |
| Skin | Long-term sun exposure | |
| Wound healing | Diet low in vitamin C | Scurvy (poor wound healing) |
| Immune system | Unprotected sex | HIV infection |
6. Conventionally accepted risk factors for heart disease include smoking, a high-fat diet and physical inactivity. Preventive medicine would therefore attempt to reduce susceptibility to heart disease by focusing on smoking reduction, reducing fatty foods in the diet and increasing levels of activity.
There are many possible preventative approaches. These include:
Chapter 2.1b Barriers to disease: wound healing
Introduction
• the physiology of a particular topic or physiological system is described
• based on this understanding of how the healthy body should function, the pathology relevant to the topic or system (i.e. what happens when disease causes imbalance) is explored
• the conventional medicine approach to treatment of the diseases that have been described is discussed
• comparisons with the language of one holistic medical perspective, that of Chinese medicine, are brought in wherever possible. These ‘translations’ relate to physiology, pathology and the effects of medical treatments. To distinguish these from the main part of the text, this text is be presented in characteristic boxes. The rationale for these comparisons is explained in detail in the Note to the Reader in the preliminary pages of this book.
The role of wound healing and clotting
The processes of wound healing and clotting were introduced in Chapter 2.1a as two of the mechanical barriers to disease. It was pointed out that these are different from the purely structural barriers of skin, mucous membranes and bone. Instead, they are both dynamic processes that are set in motion after injury has occurred. They prevent the damage from worsening, and enable repair to take place. In this way, their role is similar to that of the immune system.
This chapter focuses on wound healing. The principles of blood clotting are studied in Chapter 2.1c.
The physiology of wound healing
A description of the mechanism of wound healing is fundamental to a full understanding of how the body responds to disease. There are many situations in disease when the healthy structure of the body tissues is damaged and has to be repaired by means of this delicate process. The formation of a blood clot is the first stage of wound healing, and this is described in more detail in Chapter 2.1c.
Primary wound healing
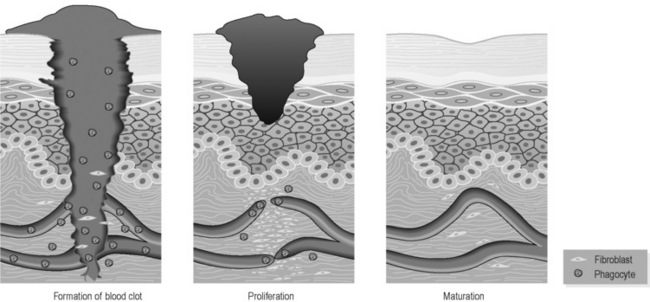
Primary wound healing can take place when the edges of a cut or puncture are in close opposition. Figure 2.1b-I illustrates the three stages of primary wound healing. The edges of the wound ooze blood from the broken capillaries, and the blood rapidly forms into a clot in the confined space. The blood clot releases chemicals that stimulate the process of ‘chemotaxis’, i.e. the attraction of the cells of the immune system (the leukocytes) and the fibroblasts (the connective tissue repair cells) into the region of the clot. The phagocytic (‘engulfing’) leukocytes move into the clot and absorb and remove cell debris, dirt and bacteria. Fibroblasts lay down a delicate network of fibrous strands that begin to bridge the gap formed by the wound. Into this meshwork the broken ends of the capillaries start to re-grow a new network of tiny vessels so that this developing scar tissue has a rich blood supply. At the same time, the deepest layer of the epithelium of the broken skin grows through the upper regions of the blood clot to close the breach formed by the injury. This stage is one of proliferation, and when the fibrous and capillary network is sufficiently strong it causes the scab, the dried blood clot overlying the wound, to drop away, leaving the pink and delicate scar tissue protected by a layer of new epithelium beneath. The proliferative stage takes 5–30 days. Over the next few days to weeks the maturation phase involves the delicate scar tissue becoming strengthened and more organised due to increasing amounts of fibrous tissue. The initially complex network of tiny capillaries is simplified in this phase. At the end of this phase what remains is a stronger, more densely structured and paler tissue than the newly formed scar.
Secondary wound healing
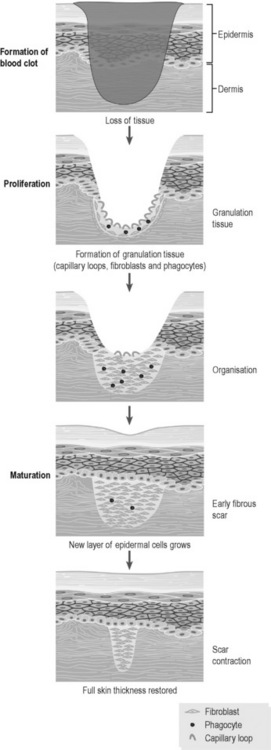
Secondary wound healing is the process that takes place when the wound leaves a gap in both the skin and the underlying connective tissue. Figure 2.1b-II illustrates the three stages of secondary wound healing. As is the case with primary wound healing, the first stage is the lining of this breach with a blood clot originating from blood that has oozed from the remaining damaged tissue. The clot encourages the ingrowth of new fibrous tissue and capillaries and the appearance of phagocytic cells to remove debris and bacteria. This delicate new tissue is known as ‘granulation tissue’. This proliferative stage takes longer than the corresponding stage in primary wound healing, the time to healing being dependent on the size of the breach in the tissue, and the health and quality of blood supply to the underlying tissue. If foreign bodies (dirt) and bacteria are present they can be the focus for ongoing damage, and will further slow this stage of the healing process. The initially shallow layer of proliferating new tissue cannot yet be lined by epithelium and, once the scab drops away, it is instead covered by a moist yellowing layer of dead cells called ‘slough’. Like the old blood clot, slough continues to be a stimulus for the chemotaxis of fibroblasts, leukocytes and new capillaries. Once the new scar tissue reaches the level of the edges of the broken skin epithelium, the new epithelium can grow inwards, closing the breach by degrees. Any breach in an epithelium is called an ‘ulcer’, which means that secondary wound healing always involves the formation of an ulcer. Ideally, the ulcer is gradually reduced in size until it is has been closed over entirely by new epithelium. Following the closure of the ulcer the maturation phase continues to strengthen and organise the new fibrous tissue until the healed wound eventually appears as a pale, shiny patch of tough new scar (see Q2.1b-1 and Q2.1b-2) .
.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 .
. .
. .
. .
.