36
Avulsions of the Flexor Digitorum Profundus
Donald M. Lewis and Randall W. Culp
History and Clinical Presentation
A 43-year-old right hand dominant air transportation specialist presented with pain in his left ring finger after an injury sustained at work. The patient reported pulling on the handle of a rototiller, which suddenly stopped, causing his finger to be forcibly hyperextended. He reported hearing a snap when this occurred and experienced immediate pain in his ring finger. He reports no prior injury to this area. This patient complained of pain at the level of the distal interphalangeal (DIP) joint of the ring finger.
Physical Examination
The patient had volar swelling and tenderness, and could not actively flex his finger at the level of the DIP joint. Upon making a fist, he had a noticeable lack of flexion compared with the other digits (Fig. 36–1). The flexor digitorum profundi (FDP) to the other digits were intact as demonstrated by blocking the digits in extension at the level of the middle phalanx, and asking him to flex at the level of the DIP joints. The flexor digitorum superficialis (FDS) was intact in all fingers, as demonstrated by blocking the adjacent digits in extension at the level of the proximal interphalangeal (PIP) and DIP joints and asking the patient to actively flex at the level of the PIP joint in the examined finger. Active extension was possible at the metacarpophalangeal (MP), PIP, and DIP levels of all fingers. He had no complaints of numbness or tingling. He also had no complaints of pain in the palm, wrist, or forearm.
PEARLS
- The physical examination should check for active flexion and extension of the DIP, PIP, and MP joints separately to ensure the FDP, FDS, and extensors are intact.
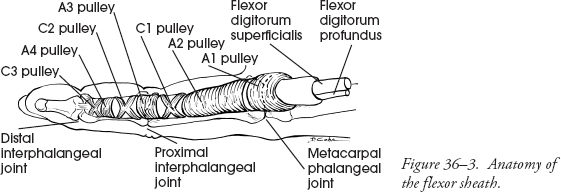
- The A2 and A4 pulleys should be preserved at all times to prevent bow-stringing.
- If the bony fragment is too small or comminuted, it can be excised and the tendon repaired directly to the distal phalanx as in a type 1 or 2 injury.
PITFALLS
- The tendon must be secured through or around the distal phalanx; fixation to the distal tendon remnant or periosteum is not secure.
- The proximal tendon end must not be debrided or advanced more than 1.5 cm, to prevent tethering of the FDP and the quadrigia effect.
- For type 1 and type 2 injuries, the PIP joint level must be explored before the palm, to prevent pulling the tendon proximally and converting a type 2 injury to a type 1 injury. This will rupture the long vinculum and its blood supply.
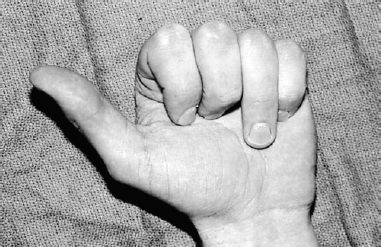
Figure 36–1. Presentation with ring finger unable to actively flex at the distal interphalangeal (DIP) joint.

Figure 36–2. Radiographs of the distal phalanx bony avulsion.
Diagnostic Studies
Individual radiographs of the left ring finger and hand were obtained. A small bony avulsion was seen at the volar proximal aspect of the distal phalanx of the affected finger (Fig. 36–2).
Differential Diagnosis
Bony flexor digitorum profundus (FDP) avulsion
Fracture/dislocation of the distal phalanx
Diagnosis
The patient was diagnosed with bony flexor digitorum profundus avulsion. This is a classic history and presentation of an acute “jersey finger.” Four types of FDP avulsions have been described, as modified from Leddy’s original description:
Type 1: Distal tendinous avulsion with proximal retraction into the palm
Type 2: Distal tendinous avulsion with retraction to the PIP joint level
Type 3: Distal bony avulsion with retraction to the A4 pulley
Type 4: Distal bony avulsion with FDP avulsion from the bony fragment
The ring finger is the most common profundus tendon avulsion. A typical presentation is in sports injuries when the participant grabs the opponent’s jersey in a tackle, undergoing forced extension of the fingertip while the profundus is under maximal contraction. Thus the name “jersey” or “rugby” finger was coined.
Type 1 and 2 injuries are defined by proximal retraction of the FDP tendon into the palm and finger respectively, with subsequent rupture of the short and possibly long vincula. Patients with a type 1 injury often have swelling, pain, and tenderness in the palm, and patients with a type 2 injury have swelling, pain, tenderness, and decreased motion at the level of the PIP joint. Sometimes a small fleck of bone is seen volarly at the level of the PIP joint on the lateral radiograph in type 2 injuries.
Surgical Management
A comfortable ulnar gutter splint was applied to the patient with the ring and small fingers in the intrinsic-plus position. He was scheduled urgently for outpatient surgery that week. Type 1 injuries should be repaired within 7 to 10 days, as the tendon blood supply is theoretically compromised, due to rupture of the long and short vincula when the tendon retracts into the palm. Type 2, 3, and 4 injuries have a longer safety zone for repair, with successful reports greater than 2 months after injury. Earlier repair is recommended to facilitate rehabilitation, decrease morbidity, and prevent a possible conversion to a type 1 injury, with later rupture of the long vinculum and retraction into the palm.
The next day, the patient was placed supine on the operating room table after obtaining general endotracheal anesthesia. Regional axillary block anesthesia is an acceptable alternative. The arm was placed on a hand table with a well-padded proximal arm tourniquet. After prep and drape, the limb was exsanguinated with an Esmarch bandage and the tourniquet inflated to 250 mm Hg. A volar zigzag incision was made at the level of the DIP joint on the ring finger, and exploration using loupe magnification was performed down to the flexor sheath. Hemostasis was meticulously maintained using bipolar electrocautery, and both neurovascular bundles were carefully protected throughout the procedure. The sheath was opened distal to the A4 pulley, taking care to preserve this pulley throughout the procedure to prevent bow-stringing of the tendon postoperatively (Fig. 36–3). A window between the C3 and A5 pulleys was opened to expose the distal bony avulsion fragment, and it was seen that the FDP tendon was still attached to this piece of the distal phalanx, indicating a type 3 injury. Hematoma and debris were curetted from the piece and from the avulsion site. The piece was reduced and held into position with a 0.035-inch Kirschner wire, and under fluoroscopy two 1.5-mm titanium self-tapping screws were placed with bicortical purchase (Fig. 36–4). The fragment was seen to be stable with a range of motion. The tourniquet was deflated, hemostasis obtained, and saline irrigation performed. The skin was closed with 4–0 nylon simple sutures, a bulky dressing applied, and a dorsal blocking splint applied with the wrist in 30 degrees of flexion. The fingers were splinted in the intrinsic-plus position to relax the FDP tendon and prevent postoperative stiffness.