, Randy Mascarenhas2, Simon Lee2 , Michael J. Salata4 and Shane J. Nho1, 3
(1)
Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, IL, USA
(2)
Department of Orthopaedic Surgery, Midwest Orthopaedics at Rush, Rush University Medical Center, Chicago, IL, USA
(3)
Midwest Orthopaedics at Rush, Hip Preservation Center, Rush University Medical Center, Chicago, IL, USA
(4)
Department of Orthopaedic Surgery, Joint Preservation and Cartilage Restoration Center, University Hospitals Case Medical Center, Cleveland, OH, USA
Abstract
Hip arthroscopy and hip preservation surgery have experienced a tremendous upsurge in the past two decades. As imaging modalities, diagnostic abilities, and surgical instrumentation/implants continue to improve, indications for arthroscopic hip surgery are expanding at a rapid rate. Understanding the complex anatomy of the hip joint and appreciating the pathology responsible for both intra-articular and extra-articular pathology are crucial to selecting the appropriate patients and procedures. This is of utmost importance in the athletic patient population. Depending on the activity or sport, young athletes with hip pain may present in different ways with a variety of complaints. This chapter will discuss specific populations of interest in hip arthroscopy and hip preservation surgery. Diagnoses pertinent to this patient population will be discussed, with an emphasis on the unique injury patterns encountered in these patients.
Introduction
Hip preservation surgery has undergone exponential growth over the past two decades. Advances in our understanding of hip pain in both the general patient population and also in multiple specific patient populations have revolutionized our ability to treat these patients. Further, substantial recent improvements in imaging modalities and surgical instrumentation have completely changed the surgical approach to these patients, from techniques that were previously open and invasive to techniques that are now more efficient and less invasive. One area of particular interest to surgeons performing hip arthroscopy and hip preservation surgery is the evaluation and treatment of the young, athletic patient population [1–5]. These patients can be challenging to diagnose and treat, as they are often high-demand, high-level patients who desire a quick return to athletic activity. Depending on the activity or sport, young athletes with hip pain may present in different ways with different complaints.
General Classifications of Hip Pain in Athletes
Hip pain in young athletes can be characterized in several different ways. Often, hip pain is classified by its location about the joint, including lateral hip pain, anterior hip pain, posterior pain, and medial hip, or groin, pain [6–8]. Common causes of lateral hip pain include greater trochanteric bursitis, gluteus medius dysfunction, iliotibial band syndrome, and meralgia paresthetica. Anterior hip pain is more variable and can result from osteoarthritis, hip flexor tendinopathy, iliopsoas bursitis, occult hip fracture or femoral neck stress fracture, acetabular labral pathology, and avascular necrosis of the femoral head. Femoroacetabular impingement (FAI) is a common source of anterior hip pain in this patient population, but FAI-related pain can be referred to other areas throughout the hip. Posterior hip pain, even in the athlete, is often referred from the lumbar spine and/or from the sacroiliac joint. Other sources of posterior hip pain include hip extensor or rotator muscle strains, proximal hamstring ruptures, and piriformis syndrome. In addition to geographic location, hip pain can also be classified as either intra-articular or extra-articular. Intra-articular sources of pain include labral tears, FAI, capsular laxity, cartilage damage, ligamentum teres pathology, and loose bodies. On the other hand, extra-articular sources of hip pain can include iliopsoas tendinitis, iliotibial band syndrome, gluteus medius and/or minimus tendinitis, greater trochanteric bursitis, femoral neck stress fracture, piriformis syndrome, and, as previously mentioned, referred pain from the lumbar spine or sacroiliac joint.
Femoroacetabular Impingement
Femoroacetabular impingement (FAI) is becoming increasingly recognized in both the general and athletic patient populations. FAI is a disorder characterized by abnormal contact between the femoral head and acetabulum, with associated labrum and articular cartilage damage. While some patients have isolated cam deformities and others that isolated pincer deformities (see Fig. 1), the majority of patients with FAI have a combination of both. Hips with impingement have been associated with limited range of motion, hyperlaxity, and athletic pubalgia, among other conditions. It is unclear as to whether FAI makes patients more susceptible to other injuries or if FAI simply develops concurrently in these patients. Regardless, athletes involved in a variety of activities, including contact athletes, pivoting athletes, overhead athletes, endurance athletes, and hypermobile athletes, are, depending on the sport, at high risk for certain hip disorders, with or without concomitant FAI. While FAI is becoming increasingly recognized in this patient population [9], it is critical to have a general appreciation for the different types of hip pain unique to this patient population in order to determine the correct diagnosis and ultimately the appropriate treatment plan.


Fig. 1
AP pelvis radiographs in competitive hockey player illustrate bilateral acetabular crossover signs indicative of femoroacetabular impingement
The Role of Hip Arthroscopy and Hip Preservation Surgery
Given the wide variety of potential diagnoses in patients presenting with hip pain, the need for both an accurate diagnosis and an appropriate treatment algorithm has become apparent. Arthroscopy has become an extremely valuable diagnostic tool in the evaluation of these patients. Diagnostic hip arthroscopy allows the clinician to evaluate for both intra- and extra-articular sources of pain, and with recent advances in instrumentation and soft tissue management, the procedure has become much more tolerable for the patient. In addition to examining intra-articular structures, including the labrum, capsule, and articular cartilage, hip arthroscopy also allows for a full evaluation of the peri-trochanteric space. Finally, hip arthroscopy allows for a dynamic intraoperative assessment of mechanical pathology, which can be extremely problematic in athletes. Mechanical pain in athletes is often thought to be related to dynamic and/or static factors. Dynamic factors include femoral retroversion, femoral varus, cam lesions, and pincer lesions, while static factors include femoral anteversion, femoral valgus, lateral acetabular under-coverage, and anterior acetabular under-coverage [1, 2, 9].
Overall, arthroscopy is extremely helpful in both the diagnosis and treatment of athletes presenting with hip pain. Given the variety of stresses placed upon the hip joint during different athletic activities, patient presentations and underlying diagnoses are variable. Specifically, while athletes such as football players, hockey players, and runners, for example, may each present to the office complaining of hip pain, the underlying diagnoses are likely to be different in each situation. This chapter will focus on several specific athletic patient populations who commonly present with a need for hip arthroscopy and/or hip preservation surgery. Specific patient populations to be discussed include contact athletes, pivoting athletes, overhead athletes, endurance athletes, and hypermobile athletes.
The Contact Athlete
Athletes involved in contact sports are at risk for a variety of different hip disorders. Participation in athletic activities involving physical contact, such as football, rugby, and hockey, among others, places athletes at risk for both repetitive mechanical intra-articular pain and direct impact-based injuries. Common injuries in this patient population include traumatic instability, contusions and “hip pointers,” and fractures of the hip and pelvis.
Of all athletes, those participating in contact sports are perhaps at the highest risk for traumatic hip instability, including subluxation and/or dislocation (see Fig. 2). Specifically, athletes most likely to sustain an injury resulting in hip instability include those participating in football and hockey [10]. It remains unclear as to whether these athletes are predisposed to hip instability due to underlying FAI. In a report of three cases of posterior hip instability by Berkes and colleagues [11], all three patients were found to have evidence of acetabular retroversion, a cam lesion, an elevated alpha angle, a labral injury, and a posterior acetabular rim fracture. While the presence of the bony fracture and possibly the labral injury can likely be attributed to the initial instability event, the other associated findings are clearly unrelated to the injury, and the question remains: do such anatomical abnormalities predispose these athletes to hip instability? Philippon and colleagues [10] performed hip arthroscopy on 14 professional athletes at a mean time of 125 days following traumatic hip dislocation and found all patients to have labral tears. Nine of the 14 athletes had evidence of FAI with cam- and/or pincer-type pathology. Despite the mean time from dislocation to reduction being only 3.56 h, all patients were found to have chondral defects at the time of arthroscopy, again suggesting possible preexisting intra-articular pathology from underlying FAI.
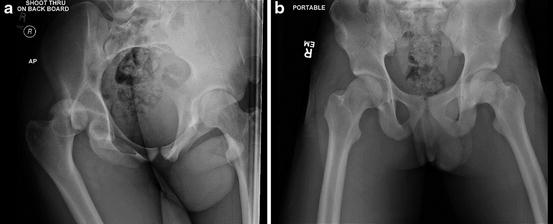
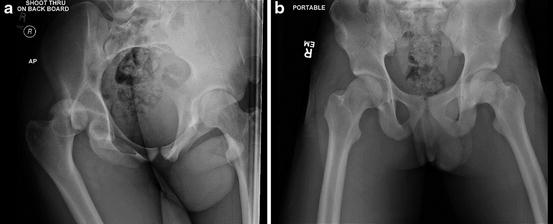
Fig. 2
(a) Portable AP pelvis radiographs show a posterior hip dislocation in a football player. (b) Postreduction films indicate a successful reduction of the dislocated hip
Hip pointer injuries are also common in contact athletes. The term “hip pointer” refers to an injury resulting from direct blunt trauma to the iliac crest. This type of injury is typically sustained only during contact sports after a direct blow to the hip and causes substantial pain and often an inability to continue participation [6, 12]. The trauma from the direct blow leads to subperiosteal edema with subsequent hematoma formation and a contusion of the iliac crest itself. In these situations, the history is usually diagnostic as patients are able to recall the specific inciting event and also point to where the pain is. Usually, plain radiographs are sufficient to rule out fracture and further diagnostic imaging is unnecessary. These patients will benefit from a course of activity modification, ice, and compression to the area. Occasionally, these patients may be managed temporarily with injections of local anesthetic to allow them quicker return to play [13]. While treatment for hip pointers is almost exclusively nonoperative, patients with persistent pain may be evaluated with hip arthroscopy in order to assess for possible concomitant intra-articular injuries.
Avulsion fractures near the hip represent another diagnosis commonly seen in the contact athlete, though noncontact athletes can sustain these injuries as well. Avulsion fractures are more common in the adolescent patient population and are typically the result of a sudden forceful contraction of a muscle attached to the apophysis. These injuries can be sustained with both forceful concentric and eccentric contractions. Common sites of injury include the anterior superior iliac spine (sartorius, tensor fascia lata), ischial tuberosity (hamstrings), anterior inferior iliac spine (direct head of rectus femoris), lesser trochanter (iliopsoas), greater trochanter (abductors), and iliac crest (from external and abdominal obliques) [14, 15]. While these injuries can usually be managed without surgery, nonunion or malunion can become problematic. For example, Matsuda reported on a case of a traumatic anterior iliac spine apophyseal avulsion fracture leading to secondary symptomatic FAI that ultimately required arthroscopic surgery with anterior iliac spinoplasty [16]. In this case, the patient was also noted to have acetabular retroversion and a cam deformity, which highlights the importance of evaluating for concomitant impingement-related symptoms in this patient population. Traumatic avulsion fractures/injuries of the ligamentum teres have also become increasingly recognized, and arthroscopic surgery is sometimes warranted. In a series including 23 patients with traumatic ligamentum teres ruptures undergoing hip arthroscopy, Byrd and Jones noted an average improvement in modified Harris Hip Score from 47 to 90 [17]. Interestingly, despite advanced imaging, the diagnosis of ligamentum teres rupture was made preoperatively in only 2 of the 23 cases, and thus arthroscopy proved to be both diagnostic and therapeutic for these patients.
The Pivoting Athlete
Athletes participating in sports that involve a substantial amount of pivoting are at increased risk for several specific hip injuries. Some of the more common sports involving pivoting include soccer, lacrosse, wrestling, Australian rules football, and field hockey. The amount of strain placed on the hip and pelvis during a forceful pivot motion can be significant, leading to multiple painful conditions, including FAI, athletic pubalgia, osteitis pubis, and muscle sprains secondary to overuse. The pivoting action itself is thought to translate force down the kinetic chain, causing a compensatory overload from the hip to the knee, ankle, and foot, potentially leading to injury in these areas as well. Athletes engaged in pivoting sports often develop hip pain localized to the groin. Given the complex anatomy in this region, the differential diagnosis in these patients is extremely broad. Common diagnoses include FAI, adductor muscle strains, and osteitis pubis. Other causes of groin pain in these athletes are summarized in Table 1.
Table 1
Common causes of groin pain in athletes
FAI |
|---|
Adductor strains |
Osteitis pubis |
Athletic pubalgia |
Ilioinguinal neuralgia |
Avulsion fractures |
Bursitis |
Rectus femoris strain |
Obturator nerve entrapment |
AVN of the femoral head |
SCFE |
Snapping hip |
Adductor muscle strains are common in the pivoting athlete patient population [18–22]. These injuries are typically referred to as groin strains and are most often encountered by athletes participating in ice hockey, soccer [23], and Australian football. Adductor strains are more likely to occur in athletes with decreased adductor strength relative to abductor strength, as noted by Tyler and colleagues [24]. Specifically, Tyler et al. examined 47 professional hockey players and noted that athletes were 17 times more likely to sustain an adductor strain if their adductor strength was less than 80 % that of the ipsilateral abductor [24]. In another study, decreased adductor strength as well as flexibility have been shown to be risk factors in athletes [19], though the study by Tyler did not find adductor flexibility (or lack thereof) to be a risk factor [24]. Osteitis pubis is another diagnosis commonly encountered in the pivoting athlete, with pain most often localized to the groin. Thought to be a chronic, overuse injury caused by overloading of the pubic symphysis and adjacent parasymphyseal bone, patients with osteitis pubis will eventually develop a bony stress reaction affecting the pubic symphysis and/or the parasymphyseal bone [25]. Arriving at this diagnosis can be challenging, as patients will often complain of vague groin pain with adduction-, rotation-, and flexion-type activities, but occasionally, patients will have pain directly over the pubic symphysis.
Athletic pubalgia, or sports hernia, has become an increasingly recognized diagnosis in the pivoting athlete. Occurring predominantly in men, athletic pubalgia is an occult hernia caused by weakness (or a tear) in the posterior inguinal wall. A variety of anatomical structures may be involved, including attenuation of the transversalis fascia, partial avulsion of the internal oblique muscle fibers at the pubic tubercle, and disruption of the body of the internal oblique muscle itself. The etiology is poorly understood but is thought to be related to repetitive twisting and turning at high speed, which places substantial stress on the inguinal wall musculature. Typical exacerbating motions in these athletes include trunk hyperextension and thigh hyperabduction [26, 27]. Patients with this injury often have pain relief with rest and symptoms only become apparent during exacerbating movements. Unlike other more classic hernia presentations, there is no palpable bulge or other clinically appreciable signs of hernia in these patients, making the diagnosis challenging. Patients will often have tenderness over the pubic tubercle, especially with resisted hip adduction and resisted sit-up motions.
Many of these athletes can have concomitant athletic pubalgia and FAI. It is unclear as to whether anatomical features of FAI predispose these patients to the development of a sports hernia. Certainly there is a relationship between limited hip range of motion, in particular flexion and internal rotation, and the development of symptomatic groin pain [28]. In these cases, it is imperative for the surgeon to appreciate the potential for underlying FAI, as both nonoperative and operative treatments aimed only at athletic pubalgia are unlikely to be beneficial [29, 30]. Hammoud and colleagues [31] reported on a series of 38 professional athletes with athletic pubalgia undergoing arthroscopic surgery for FAI. The authors noted 32 % of these athletes had previously undergone isolated surgical treatment for athletic pubalgia, with none of these patients returning to their previous level of competition after the index procedure. Following the arthroscopic procedure for FAI, 36 of 38 patients were able to return to their previous level of play at an average of 5.9 months postoperatively [31].
The Overhead Athlete
Overhead athletes are subject to the same subset of hip disorders commonly encountered in other athletic patient populations, including FAI. These athletes, however, may experience unique sequelae from FAI not typically found in other athletes, as alterations in their biomechanics often occur in a compensatory fashion up the kinetic chain, from the hip to the sacroiliac joint, spine, elbow, and shoulder. Thus, while many overhead athletes, including pitchers, quarterbacks, and volleyball players, present with elbow and/or shoulder injuries, some authors will argue that baseline hip pathology is ultimately responsible [32, 33]. The act of overhead throwing places a tremendous force on the hip at all stages in the pitching cycle. The biomechanics of the pitching cycle are complex, and while much attention is given to the force placed on both the shoulder and elbow, hip motion and stability also play a key role in stabilizing the shoulder/elbow and even generating ball velocity. In 2010, Robb and colleagues [34] examined 19 professional baseball pictures throughout the cycle with a focus on hip range of motion. The authors found a significantly decreased passive range of motion in the nondominant hip when compared to the dominant hip for all ranges. Further, the authors found that the total arc of rotation of the nondominant hand was correlated with ball velocity. They concluded that the motion disparity between the dominant and nondominant hips was correlated with various pitching biomechanical parameters [34]. Laudner et al. [35] found that pitchers have significantly smaller amounts of hip internal rotation compared to positional players and, as a result, rely more on energy created in the core and upper extremity to throw. This data suggests a correlation between upper extremity injuries in pitchers and abnormal hip kinematics (less range of motion).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








