12 Articular Cartilage Paste Grafting
Articular cartilage lesions left alone fail to heal. Although many may be asymptomatic, those lesions that cause pain are a significant source of disability for patients. Treatment with debridement, drilling, and microfracturing have produced variable results though generally in the 50% to 65% pain relief success range.1–5 Resurfacing efforts using perichondrium, periosteum, fascia, carbon fibers, and collagen matrices have produced hyaline-like articular cartilage in various animal studies.6–9 However, long-term studies generally have noted breakdown of the newly formed articular cartilage caps at the peripheral edges. In general, the interface between new and old cartilage has not fused, leading to poor force transduction and eventually tissue degeneration.9,10 Mesenchymal cells and growth factors have been added to various matrices to improve the fusion between old and new cartilage, again with limited clinical experience. Combinations of articular cartilage cells and perichondrium have had variable results.3 These procedures require an open arthrotomy, sewing of a perichondral flap, and then injection of cultured chondrocytes beneath the flap. Coring out of cartilage lesions followed by the placement of single or multiple intact cartilage and bone plugs has the advantage that a surface of intact hyaline articular cartilage is immediately available for weight bearing.11,12 The disadvantages include morbidity produced from the harvest sites, which are usually along the medial or lateral femoral condylar ridges. These areas are weight-bearing surfaces that are not likely to give up their cartilage without long-term consequences. Additionally, few articular cartilage lesions are truly round. Therefore, further damage must be created to round out these irregular lesions. Lastly, if the plug techniques fail, a large hole has been created in the joint surface at the defect. Paste grafting of articular cartilage and bone into morselized arthritic and traumatic lesions has produced effective repair tissue for large irregular lesions.
84% of patients followed in a 2- to 12-year follow-up study reported improvement in pain of at least one grade on a 1 to 4 pain grading scale.13,14 The paste graft technique can be performed as a single outpatient arthroscopic procedure. The technique and indications are as follows:
Indications
Full-thickness articular cartilage loss in isolated areas of the knee and ankle joints due to direct traumatic lesion or chronic arthritic changes
Contraindications
- Inflammatory arthritis
- Severe tricompartmental osteoarthritis
- Patient’s inability to comply with a non-weight-bearing postoperative program.
Physical Examination
Variable presentation with or without pain, crepitus, or swelling at the joint line
Diagnostic Tests
- Standing x-rays of the knee with posteroanterior (PA) flexion, anteroposterior (AP), skyline, lateral, and full-length (hip to ankle) views
- Magnetic resonance imaging (MRI) with cartilage-enhancing techniques
Special Considerations
Cartilage lesions can sometimes be extensive but the pain often comes only from the central area of exposed bone. Even partial coverage with new repair tissue provides relief. The patella is refractory to cartilage growth; however, the opposing trochlea is ideal. In patellar femoral pain, when there is both a patellar and trochlea lesion, coverage of the trochlea lesion frequently provides pain relief.
Preoperative Planning and Timing of Surgery
- Optimize alignment and gait with heel wedges and physical therapy.
- Initiate muscle strengthening and range of motion exercises.
- If the meniscus is absent or deficient, plan for simultaneous meniscus allograft replacement.
- If the alignment is in significant varus or valgus, plan for simultaneous corrective osteotomy.
- Operate after nonoperative methods have failed.
- Be sure that the patient understands that any effort at cartilage transplantation can make the knee worse.
Special Instruments
- Chonstruct Instrument Set from Mitek Inc. (Norwood, Massachusetts)
- If Chonstruct set not available, then Instrument Makar grafters (Okemos, Michigan) can be used.
- Chondroplasty awls from Mitek, Inc. or Richards, Inc. (Bartlett, Tennessee)
Anesthesia
Local anesthesia with IV sedation, general anesthesia, or epidural
Patient and Equipment Positions
- Supine with circumferential leg holder (Instrument Makar)
- A tourniquet should not be used to improve bleeding at the lesion.
Surgical Procedure
- Complete arthroscopic joint evaluation
- Debridement of loose flaps of articular cartilage
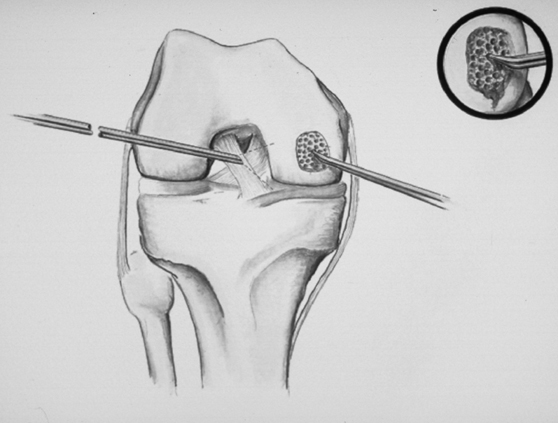
- Morselization of the arthritic area with chondroplasty awls (Fig. 12–1)
- Harvest of articular cartilage and underlying bone from the intercondylar notch using trephines from the Chonstruct Set. (Fig. 12–2)
- Paste formation in a graft impactor from the Chonstruct Set. (Fig. 12–3)
- Loading the paste into the trephines
- Impaction of the paste into the prepared arthritic defects through the anterior medial or lateral arthroscopic portals (Fig. 12–4)
- Placement of 50 cc of 1/4% Marcaine with epineph-rine mixed with 2 mg morphine in the knee
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








