Arthroscopy of the Talocrural and Subtalar Joints
Armen S. Kelikian
The advent of arthroscopic surgery has opened a new window to in vivo anatomy. Correlations with topographic anatomy with regard to normal landmarks—relative to portal sites as well as joint access and structures at risk—are paramount to the arthroscopist’s visualization. Knowledge of normal intra-articular anatomy and its variations allow one to address pathologic conditions. Watanabe first introduced ankle arthroscopy in 1970 and subsequently published a series of 28 ankles.1 Guhl and, subsequently, Yates and Grana expanded visualization via invasive and noninvasive distraction apparatuses.2, 3 Ferkel published a classic text Arthroscopic Surgery, The Foot and Ankle in 1996.4 Recently van Dijk has expanded techniques to the posterior approaches of the ankle, subtalar, and retrocalcaneal bursa as well as endoscopy of the peroneal, posterior tibial, and flexor hallucis longus tendons.5
ANATOMIC LANDMARKS
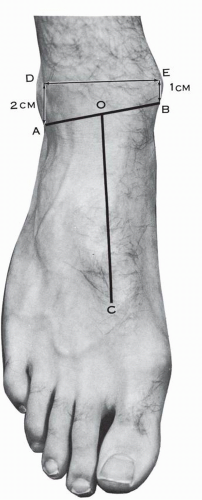
Osseous landmarks are the lateral and medial malleoli. The ankle joint is subtended by points 1 cm proximal to the medial malleolar tip and 2 cm proximal to the tip of the lateral malleolar (. 11.1). The cross-section of the ankle at 1 cm from the tip of the medial malleolus (Fig. 11.2) demonstrates the following relationships: anteriorly from medial to lateral the saphenous vein and nerve over the medial malleolus. The tibialis anterior tendon is at the junction of the medial malleolus with the tibial plafond. The extensor hallucis longus tendon is anterior to the medial aspect of the tibial plafond and the extensor digitorum longus tendons correspond to the lateral aspect of the tibial plafond and to the tibiofibular synovial fringe. The dorsalis pedal vessels (anterior tibial vessels) and the deep peroneal nerves are lateral and deep to the extensor hallucis longus tendon. These relationships are also well represented in the dissection of the ankle anteriorly (Fig. 11.3). The superficial peroneal nerve has already divided into its terminal branches—intermediate and medial dorsal cutaneous nerve at an average of 6.5 cm proximal to the tip of the lateral malleolus. The intermediate dorsal cutaneous nerve crosses over the tibiofibular syndesmosis, crosses obliquely the fifth and fourth extensor digitorum longus tendons, and courses over the third intermetatarsal space (Fig. 11.4). This nerve can be visualized and palpated with plantar flexion and inversion of the foot. The saphenous nerve crosses the medial malleolus anteriorly. Posteriorly on the cross-sectional study of the ankle, the tibialis posterior tendon is posterior to the medial malleolus and the peronei are posterior to the lateral malleolus. The posterior peroneal vessels are posterior to the tibiofibular syndesmosis. The Achilles tendon is central and medial; posterior to the tibial plafond are the flexor hallucis tendon and the posterior neurovascular bundle. The short saphenous vein and sural nerve are in the interval between the peronei tendons and the Achilles tendon (Figs. 11.2, 11.5, and 11.6).
ANKLE ARTHROSCOPIC PORTALS
Arthroscopic portals in the foot and ankle rely on access, visualization, structures at risk, and cross-sectional anatomy. They provide a window to normal and abnormal anatomy. These portals are: anteromedial, anterolateral, accessory anterolateral, accessory anteromedial, and posterolateral. The anterior medial portal is at the joint line, 1 cm proximal to the tip of the medial malleolus, and just medial to the anterior tibial tendon with the ankle dorsiflexed and distracted. The mean distension volume of the ankle joint is 20 mL (range 16-30 mL).6 The anterior capsule insertion on the tibia is between 6 to 8 mm from the joint line proximally and about 8 to 10 mm distally from the talar articular surface according to Testut.7 The anterolateral portal is at the same level and just lateral to the peroneus tertius tendon. The lateral portal can be determined by transilluminating the skin to visualize and avoid the superficial peroneal nerve. An accessory anterior portal can be used between the extensor hallucis longus and tibialis anticus tendons8 (Fig. 11.7). The accessory anteromedial portal is 1 cm below the anterior edge of the anterior colliculus whereas the accessory anterolateral portal is 1 cm anterior to the lateral malleolus4 (Fig. 11.7).The posterior lateral portal is just lateral to the lateral border of the Achilles tendon and between 12 to 25 mm proximal to the tip of the fibula4 (Fig. 11.7). The posteromedial portal is medial to the Achilles tendon and directed toward the posterolateral canola away from the posterior neurovascular structures. This technique has been popularized by van Dijk.5, 9 Another utility
portal also used for subtalar arthroscopy is the anterolateral, which is 2 cm anterior and 1 cm distal to the fibular tip.4
portal also used for subtalar arthroscopy is the anterolateral, which is 2 cm anterior and 1 cm distal to the fibular tip.4
Anterior Arthroscopy Portals
Numerous anatomic studies have shown the incisional hazards relative to the neurovascular structures that envelop the region of the ankle and subtalar joints. A Feiwell and Frey study found a 10% incidence of injury to the superficial peroneal nerve via the anterolateral portal whereas the anterocentral portal (which has since then been abandoned) approached a 30% rate.10, 11, 12 Anatomic variations such as a laterally situated anterior tibial artery in 5.5% of specimens according to Huber (see Chapter 7) and its transmalleolar branches further illustrates the value of regional anatomy for the arthroscopists13 (Fig. 11.8). The medial and lateral transmalleolar arteries’ distances from the joint line vary with ankle flexion and extension. The lateral transmalleolar branch distance from the joint line increases from 2.47 to 6.41 mm whereas the medial branch distance goes from 1.58 to 4.73 mm with plantar flexion in 18 cadaveric dissection.14
Intra-articular Anatomy
The anteromedial portal affords excellent visualization in the anteroposterior direction because of the medially situated groove in the tibial plafond or notch of Harty.15 It is the first portal established after saline insufflation. Again it is made at the level of the ankle joint line 1 cm above the medial malleolar tip in the soft spot just medial to the anterior tibial tendon. The saphenous nerve and vein have a safe zone 10 mm and 7.4 mm away or medial to this portal.10 The cross-sectional anatomy illustrates these structures (see Fig. 11.2).
The eight-point anterior and six-point central exams are shown in Figure 11.9.4 The anterolateral portal gives additional viewing when portals are changed. Once the anteromedial portal is employed a spinal needle lateral to the peroneus tertius and intermediate branch of the superficial peroneal nerve is introduced. The lateral gutter can be well visualized with a 30-degree arthroscope. The posterolateral exam is made by introducing the spinal needle in the soft spot with triangular borders consisting of the superior calcaneal border inferiorly, the Achilles tendon posteriorly, and the peronei anteriorly (Fig. 11.7). The soft portion of the capsule or cul-de-sac just medial and below the transverse ligament (but lateral to the FHL) is penetrated. The deep deltoid, medial gutter, the articular surfaces, and posterolateral corner are inspected to complete the 21-point exam (Fig. 11.9).
When viewing the articular surface of the talus the central depression just medial to this on the articular surface of the tibia is the notch of Harty (Fig. 11.10). There are three fascicles whose most distal component can be implicated as a cause of dorsiflexion impingement as described by Basset et al.16, 17 (Fig. 11.11A). A distal fascicle has been identified in 21% of cases by Ray et al.18 Nikolopoulos visualized the fascicle in up to 90% of impingement cases.19 The anterior capsule and anterior talar dome is seen first when viewed from the anteromedial portal (see Fig. 11.11B). Laterally one then encounters the anterior inferior tibiofibular ligament (see Fig. 11.11C,D). The lateral malleolar articular surface is visualized next in the eight-point exam as described by Ferkel and Scranton.20 The interosseous ligament forms the proximal roof of the tibiofibular syndesmosis and is recessed 6 mm (see Fig. 11.11E). This can be probed but not visualized. The synovial fringe from this articulation is seen. With dorsiflexion of the ankle the examiner will see the space or culde-sac between the transverse ligament and the distal ligaments increase; also, the synovial fringe will retract. Looking in the
posterolateral corner, the posterior tibiofibular ligaments’ deep component or transverse ligament is encountered. By virtue of its attachment from the malleolar fossa of the fibula to the posterior cartilaginous rim of the tibia, it is analogous to the labrum of the shoulder. The superficial component of this ligament cannot be seen from the anterior portal according to Golano et al.21 There is discussion that an inferior slip of the deep ligament is a separate fascicle and referred to as the posterior intermalleolar ligament by Paturet.21, 22, 23



posterolateral corner, the posterior tibiofibular ligaments’ deep component or transverse ligament is encountered. By virtue of its attachment from the malleolar fossa of the fibula to the posterior cartilaginous rim of the tibia, it is analogous to the labrum of the shoulder. The superficial component of this ligament cannot be seen from the anterior portal according to Golano et al.21 There is discussion that an inferior slip of the deep ligament is a separate fascicle and referred to as the posterior intermalleolar ligament by Paturet.21, 22, 23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree