Chapter 50 Arthroscopy of the Foot and Ankle
Ankle Arthroscopy
Arthroscopic Examination and Débridement of the Ankle Joint
 For routine ankle arthroscopy, place the patient supine, with the operative extremity in a leg holder such that the hip and knee are flexed, with the foot hanging free, resulting in gravity-assisted distraction. This also allows free ankle range of motion, which can assist in access to different parts of the ankle (Fig. 50-1).
For routine ankle arthroscopy, place the patient supine, with the operative extremity in a leg holder such that the hip and knee are flexed, with the foot hanging free, resulting in gravity-assisted distraction. This also allows free ankle range of motion, which can assist in access to different parts of the ankle (Fig. 50-1).
 Mark portal placement after establishing the path of the superficial peroneal nerve, which can be seen subcutaneously after plantar flexion and inversion of the foot (Fig. 50-2).
Mark portal placement after establishing the path of the superficial peroneal nerve, which can be seen subcutaneously after plantar flexion and inversion of the foot (Fig. 50-2).
 Mark anterolateral and anteromedial portals at the joint line, which can be palpated, staying away from the peroneal nerve (Fig. 50-3).
Mark anterolateral and anteromedial portals at the joint line, which can be palpated, staying away from the peroneal nerve (Fig. 50-3).
 After Esmarch exsanguination of the extremity and inflation of the thigh tourniquet, establish the anteromedial portal by inserting an 18-gauge spinal needle at the marked site and insufflating the joint with saline to ensure intraarticular placement and to provide more space for introduction of the blunt trocar (Fig. 50-4). Successful insufflation occurs when there is minimal resistance to the introduction of saline, when the foot dorsiflexes as the joint capsule becomes tight, and when there is backflow of the saline into the syringe after the joint is maximally distended. The anteromedial portal is established first, because there are fewer structures at risk than with the anterolateral portal.
After Esmarch exsanguination of the extremity and inflation of the thigh tourniquet, establish the anteromedial portal by inserting an 18-gauge spinal needle at the marked site and insufflating the joint with saline to ensure intraarticular placement and to provide more space for introduction of the blunt trocar (Fig. 50-4). Successful insufflation occurs when there is minimal resistance to the introduction of saline, when the foot dorsiflexes as the joint capsule becomes tight, and when there is backflow of the saline into the syringe after the joint is maximally distended. The anteromedial portal is established first, because there are fewer structures at risk than with the anterolateral portal.
 After localization of the anteromedial portal with the spinal needle, make a skin incision just large enough to insert the cannula. A large incision allows more extravasation of fluid into the surrounding soft tissues and can make the procedure more difficult.
After localization of the anteromedial portal with the spinal needle, make a skin incision just large enough to insert the cannula. A large incision allows more extravasation of fluid into the surrounding soft tissues and can make the procedure more difficult.
 Further penetrate the joint with a blunt straight hemostat to avoid damage to the saphenous nerve, which is at risk in this area.
Further penetrate the joint with a blunt straight hemostat to avoid damage to the saphenous nerve, which is at risk in this area.
 Place a 2.7-mm 30-degree arthroscope into the anteromedial portal, and establish the anterolateral portal by direct visualization of a spinal needle introduced at the site of the anticipated portal placement.
Place a 2.7-mm 30-degree arthroscope into the anteromedial portal, and establish the anterolateral portal by direct visualization of a spinal needle introduced at the site of the anticipated portal placement.
 When appropriate needle placement is seen, make the skin incision for the anterolateral portal and penetrate the joint with a blunt instrument (Fig. 50-5); then introduce the arthroscopic shaver in this portal.
When appropriate needle placement is seen, make the skin incision for the anterolateral portal and penetrate the joint with a blunt instrument (Fig. 50-5); then introduce the arthroscopic shaver in this portal.
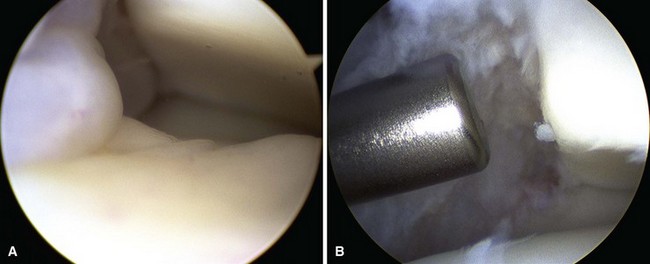
 Inspect the lateral aspect of the joint with use of instruments in the anterolateral portal as needed for débridement (Fig. 50-6), and then switch portals (arthroscope in the anterolateral portal and instruments in the anteromedial portal) for treatment of the medial side of the joint (Fig. 50-7).
Inspect the lateral aspect of the joint with use of instruments in the anterolateral portal as needed for débridement (Fig. 50-6), and then switch portals (arthroscope in the anterolateral portal and instruments in the anteromedial portal) for treatment of the medial side of the joint (Fig. 50-7).
 Noninvasive distraction can be used if needed to access the deeper aspects of the joint (Fig. 50-8). Occasionally, a posterolateral portal is needed to treat pathological processes in the posterior aspect of the ankle that cannot be reached even after distraction is applied.
Noninvasive distraction can be used if needed to access the deeper aspects of the joint (Fig. 50-8). Occasionally, a posterolateral portal is needed to treat pathological processes in the posterior aspect of the ankle that cannot be reached even after distraction is applied.
 After the procedure is completed, close the portals with suture to avoid the development of a fistula, which is a reported complication of ankle arthroscopy.
After the procedure is completed, close the portals with suture to avoid the development of a fistula, which is a reported complication of ankle arthroscopy.
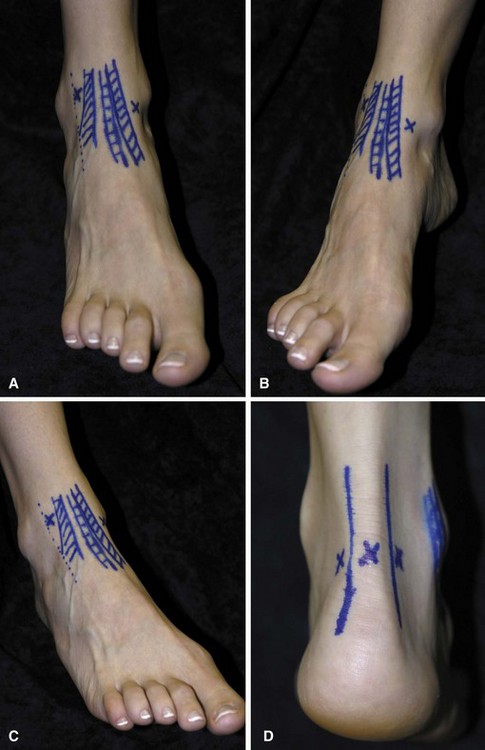
FIGURE 50-3 A, Two anterior portals for ankle arthroscopy are marked in relation to anterior tibial and other extensor tendons where they cross anterior aspect of ankle. B, Anteromedial portal site. C, Anterolateral portal site. D, Posterior portals. SEE TECHNIQUE 50-1.

FIGURE 50-5 Anterolateral portal is made with blunt instrument, followed by insertion of arthroscopic shaver. SEE TECHNIQUE 50-1.
Ankle Impingement Syndromes
Posterior Ankle Impingement
Patients with posterior ankle impingement point to the back of the ankle as the area of pain and have tenderness in the deep posterior aspect of the ankle and pain with a forced plantar flexion test (Fig. 50-9). Studies may show an os trigonum or hypertrophic posterior process of the talus, and patients obtain relief with a fluoroscopic-guided injection in the area.
Posterior Débridement for Ankle Impingement
 Place the patient prone with the foot at the end of the bed and a support under the lower leg so that the foot hangs freely (Fig. 50-10A). Keeping the foot in neutral with respect to dorsiflexion/plantar flexion and varus/valgus is the safest position in which to avoid neurovascular damage.
Place the patient prone with the foot at the end of the bed and a support under the lower leg so that the foot hangs freely (Fig. 50-10A). Keeping the foot in neutral with respect to dorsiflexion/plantar flexion and varus/valgus is the safest position in which to avoid neurovascular damage.
 Make the posterolateral portal just superior to a line from the tip of the lateral malleolus to the Achilles tendon, just lateral to the tendon (Fig. 50-10B). Insert a hemostat through a small skin incision, aiming along a line directed to the first web space of the forefoot, until it hits bone (Fig. 50-10C).
Make the posterolateral portal just superior to a line from the tip of the lateral malleolus to the Achilles tendon, just lateral to the tendon (Fig. 50-10B). Insert a hemostat through a small skin incision, aiming along a line directed to the first web space of the forefoot, until it hits bone (Fig. 50-10C).
 Make the posteromedial portal at the same level, just medial to the Achilles tendon, and insert a hemostat through the skin incision, directing it to contact the arthroscope at a 90-degree angle (Fig. 50-10D). Once the hemostat contacts the arthroscope, move it down the shaft until it hits bone and can be seen through the scope. If desired, use fluoroscopy to confirm appropriate placement.
Make the posteromedial portal at the same level, just medial to the Achilles tendon, and insert a hemostat through the skin incision, directing it to contact the arthroscope at a 90-degree angle (Fig. 50-10D). Once the hemostat contacts the arthroscope, move it down the shaft until it hits bone and can be seen through the scope. If desired, use fluoroscopy to confirm appropriate placement.
 Place a shaver in this portal and remove the posterior subtalar capsule (Fig. 5-10E). Take care to stay lateral to the flexor hallucis longus tendon to avoid damage to the neurovascular bundle (Fig. 5-10F).
Place a shaver in this portal and remove the posterior subtalar capsule (Fig. 5-10E). Take care to stay lateral to the flexor hallucis longus tendon to avoid damage to the neurovascular bundle (Fig. 5-10F).
 To remove the os trigonum, partially detach the posterior talofibular ligament and posterior talocalcaneal ligament and release the flexor retinaculum to expose the bone to be removed (Fig. 50-10G).
To remove the os trigonum, partially detach the posterior talofibular ligament and posterior talocalcaneal ligament and release the flexor retinaculum to expose the bone to be removed (Fig. 50-10G).
 If distraction is needed, a transcalcaneal traction pin can be hooked to a traction device.
If distraction is needed, a transcalcaneal traction pin can be hooked to a traction device.


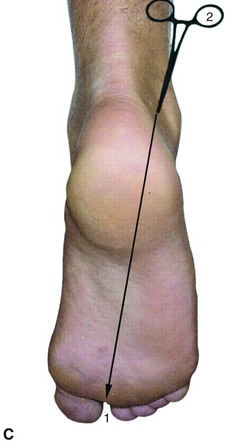
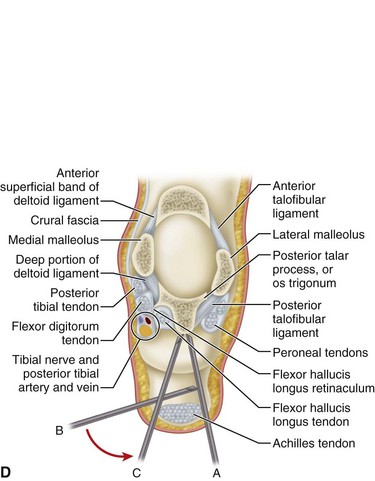

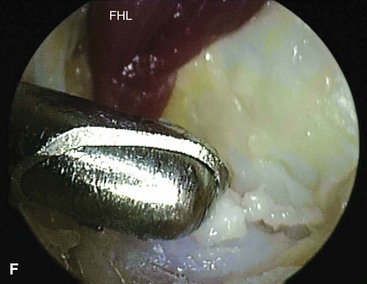
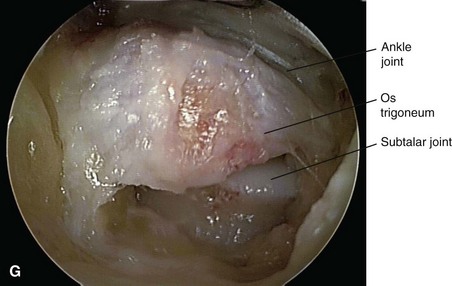
FIGURE 50-10 Posterior débridement for ankle impingement. A, Patient positioning. B, Posterolateral portal. C, Insertion of hemostat aimed along line directed to first web space. D, Insertion of arthroscope through posteromedial portal. E, Insertion of arthroscopic shaver. F, Identification of flexor hallucis longus. G, Exposure of os trigonum. SEE TECHNIQUE 50-2.
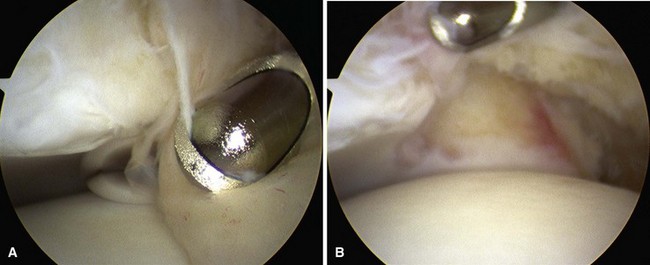
Osteochondral Lesions of the Talus
Osteochondral lesions of the talus can be treated arthroscopically and the current grade of recommendation is grade B (fair evidence), according to the literature that is currently available. Ankle arthroscopy is performed as described earlier; noninvasive distraction often is necessary to allow room for the instruments for subchondral penetration. A more thorough discussion of osteochondral lesions of the talus is given in Chapter 89.