31
Arthroscopic Treatment of Latera Tibial Plateau Fractures
Arthroscopy has been shown to have a valuable role in the treatment of lateral tibial plateau fractures.1–5 In addition to assessment of joint surface restoration, disengagement of entrapped meniscal fragments, and facilitation of meniscal repair, arthroscopic-assisted techniques, often utilizing specialized instrumentation, can achieve fracture reduction and fixation with minimal incisions, avoiding the additional trauma of open surgery and maximizing rehabilitation potential.
Classification
Schatzker6 has constructed the most useful classification scheme (Fig. 31-1). Lateral tibial plateau fractures occur from axial and lateral bending moments applied through the lateral femoral condyle, dividing the lateral tibial plateau into one of four general types of fracture pattern: central articular depression, metaphyseal wedge fracture of the lateral plateau,combined wedge and articular depression, and complex injury of the lateral plateau associated with diaphyseal or medial plateau fractures.
Clinical Evaluation and Imaging
Clinical assessment is critical to diagnosing associated vascular and neurologic injuries, including compartment syndrome.7 Ligamentous examination of the knee is often difficult due to the patient’s pain. Anteroposterior laxity suggests associated eminence fracture, and mediolateral laxity in extension usually indicates significant joint surface depression or associated medial collateral ligament (MCL) rupture.
Routine radiographs include a lateral, standard anteroposterior, 45-degree oblique, and an anteroposterior view angled 10 degrees caudally.8
Depressed articular fragments are best visualized by computed tomography (CT) scanning. Confirmation of ligament injury may require magnetic resonance imaging (MRI).
Indications
Nondisplaced fractures and those with articular surface depression of less than 2 to 3 mm that are stable to mediolateral stress can be treated nonoperatively. These fractures are treated by non-weight bearing for at least 8 to 12 weeks using a hinged knee brace, which facilitates early joint motion.
Displaced wedge and articular depression fractures alone or in combination are generally amenable to arthroscopic-assisted fixation. Other patterns of lateral plateau fractures including complex shaft and plateau and combined medial and lateral plateau fractures are usually best treated by conventional open reduction and internal fixation.
Surgical Techniques
Setup
Because of the necessary use of a fluoroscopy C-arm and monitor in addition to the usual videoarthroscopy equipment, certain adjustments to the regular arthroscopy setup are necessary. These include use of a radiolucent table, a lateral post instead of a circumferential thigh holder, and a thigh tourniquet. In general, place the videocart (with monitor) on the opposite side near the midpoint of the table (patient’s waist), position the C-arm for entry from alongside the uninjured knee, and station the fluoroscopy monitor at the foot of the table.
Initial Arthroscopy
- Establish a standard superomedial portal for large-bore inflow and an anterolateral portal for diagnostic visualization. Prior to inserting the arthroscope in its sheath, perform repeated lavage and suction to remove debris and blood clots. Additional clots can be removed using a 5 mm motorized shaver inserted through an anteromedial portal.
- Identify any associated lateral meniscus tear. If the tear is peripheral, repair it only after fracture reduction to facilitate fracture visualization.
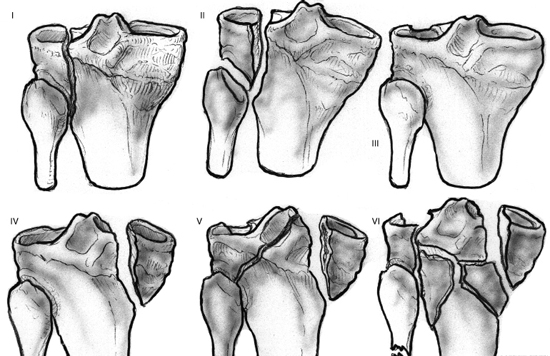
Figure 31-1 Shatzker classification of tibial plateau fractures.
Wedge Fracture Without Central Articular Depression
- If necessary, elevate any portion of the lateral meniscus that might be entrapped.
- Remove hematomas with the motorized shaver from the fracture surfaces (Fig. 31-2).
- Most of these fractures are simply widened and only minimally shifted in the vertical plane. Apply the large AO reduction forceps percutaneously to the wedge fragment anterior to the fibular head, engage the other tip against the cortex of the medial plateau, and reduce the fracture, confirming the restoration of the joint surface arthroscopically.
- Evaluate the bony reduction by fluoroscopy. Insert two parallel guidewires for 7.0 mm cannulated cancellous screws with washers to avoid screwhead migration (Fig. 31-3).
- For additional support in the vertical plane, insert an additional screw near the inferior extent of the wedge fracture.
- If the wedge fracture is significantly displaced in the vertical plane, offset the reduction forceps in an oblique orientation across the fracture (inferior-lateral) in an effort to translate the fragment vertically.
Fractures with Articular Depression (Articular Depression Alone or in Combination with a Wedge Fracture)
- Harvest iliac crest cancellous graft prior to arthroscopy; leave accessible to harvest additional graft later if needed.
- Perform arthroscopy as described above.
- Identify the level of the depressed fragments with fluoroscopy.
- Make a 1 to 2 cm skin incision anterior to the fibular head at the level of the depressed fragments (Fig. 31-4A).
- Bluntly dissect through the tibialis anterior to the tibial cortex, staying anterior to the interosseous membrane.
- Using fluoroscopy, insert a 4.5 mm drill through the lateral cortex, staying immediately below the depressed articular fragments (Fig. 31-4B).
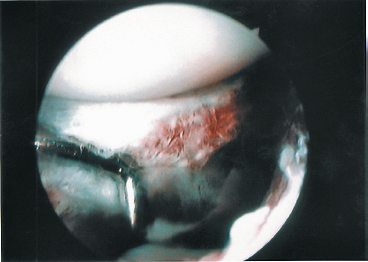
Figure 31-2 Arthroscopic view of hematoma-filled gap between articular margins in a wedge-type fracture of lateral tibial plateau.
- Through this aperture, disimpaction, reduction, and, if desired, addition of bone graft is performed.
- Specialized instruments (Special Devices Inc., Grass Valley, CA) are helpful. A straight-shafted, obliquely tipped tamp-like instrument can be used to initiate disimpaction of the fragments (Fig. 31-4C), and variously curved, blunt-tip instruments aid reduction by delivering the articular fragments upward to the joint surface (Fig. 31-4D).
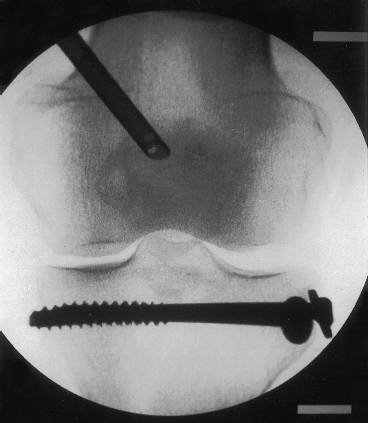
Figure 31-3 Image from fluoroscopic monitor demonstrating reduction of articular surface in wedge-type fracture of lateral tibial plateau. Arthroscopic inflow cannula is still present in the suprapatellar pouch.
- Apply counterpressure to the elevated fragment if necessary through the arthroscopy portals.
- Insert and elevate iliac crest cancellous graft as needed to support the reduction (Fig. 31-4E).
- 1Insert two parallel 7.0 mm cancellous screws with washers as described above for central depression fractures, and add a third inferior screw with washer for combined wedge and depression injuries.
- 1Perform meniscus repair once the fracture is reduced and stabilized.
Tips, Tricks, and Pitfalls
Avoid excessive application of force, and if reduction is inadequate or cannot be obtained, proceed to open reduction. Application of one tip of a reduction forceps into the anterinferior aspect of the wedge fragment can assist in elevating the fragment toward the joint surface, whereas a second pair of forceps is used to compress the fracture. Provisional Kirschner wire (K-wire) fixation can stabilize the reconstructed joint surface. Always use bone graft if there is central depression. Iliac crest graft is easily harvested through a trapdoor approach, which allows the superior aspect of the crest to be closed after harvesting the cancellous bone. This reduces bleeding and maintains the cosmetic appearance of the crest.
Postoperative Management
A compression dressing incorporating a cryotherapy cuff is applied in the operating room. In the recovery area, start continuous passive motion (CPM) with an initial range of 0 to 40 degrees. Deep venous thrombosis (DVT) prophylaxis is used on a case-by-case basis. Non-weightbearing ambulation is necessary for a minimum of 10 to 12 weeks. Thereafter, cycling and other resistance exercises are instituted. Return to full activity usually requires 6 months.
Complications
Complications are similar to those of open surgery and include DVT, infection, malreduction, loss of reduction, joint stiffness, and posttraumatic arthritis. The risks of failure to achieve adequate reduction and loss of reduction can be minimized by using arthroscopic techniques for amenable fractures only, as well as the judicious use of bone graft in cases with comminuted articular fragments.
Conclusion
The primary advantage of arthroscopic-assisted reduction is twofold: visual confirmation of articular surface restoration, and preservation of vascular supply to often comminuted fragments. It is anticipated that this approach will reduce the incidence of posttraumatic arthritis in fractures of the lateral tibial plateau.
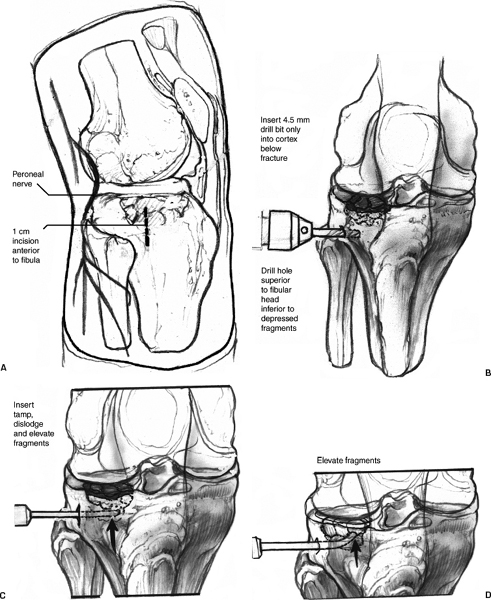
Figure 31-4 (A) Location of skin incision for insertion of beneath articular fragments. (C) Disimpaction of articular drill and instruments to elevate depressed articular fragments. (D) Elevation of articular fragments toward joint fragments. (B) Anteroposterior view of drill bit entering surface using curved disimpactor.
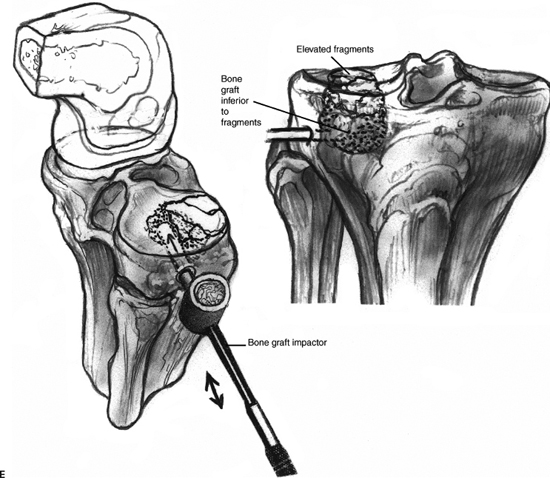
Figure 31-4 (Continued) (E) Insertion of bone graft and compaction with specialized impactor.
References
1 Caspari RB, Hutton PM, Whipple TL, et al. The role of arthroscopy in the management of tibial plateau fractures. Arthroscopy 1985;1:76–82
2 Ertl J, Marder R, Sterett W, et al. Arthroscopic assisted reduction with internal fixation of centrally depressed tibial plateau fractures. Arthroscopy 1998;14:14.
3 Ertl J, Marder R. Arthroscopy assisted fixation of fractures around the knee. In: Chow E ed. Advanced Arthroscopy. New York: Springer-Verlag; 2000: 559–571
4 Holzach P, Matter P, Minter J. Arthroscopically assisted treatment of lateral tibial plateau fractures in skiers: use of a cannulated reduction system. J Orthop Trauma 1994;8:273–281
5 Jennings JE. Arthroscopic management of tibial plateau fractures. Arthroscopy 1985;1:160–168
6 Schatzker J. Fractures of the tibial plateau. In: Chapman MW ed. Operative Orthopaedics, 2nd ed. Philadelphia: JB Lippincott; 1993: 671–684
7 Peek RD, Hayes DW. Compartment syndrome as a complication of arthroscopy. Am J Sports Med 1984;12:464–468
8 Moore TM, Harvey JP, Jr. Roentgenographic measurement of tibial plateau depression due to fracture. J Bone Joint Surg Am 1974;56:155–160
< div class='tao-gold-member'>









