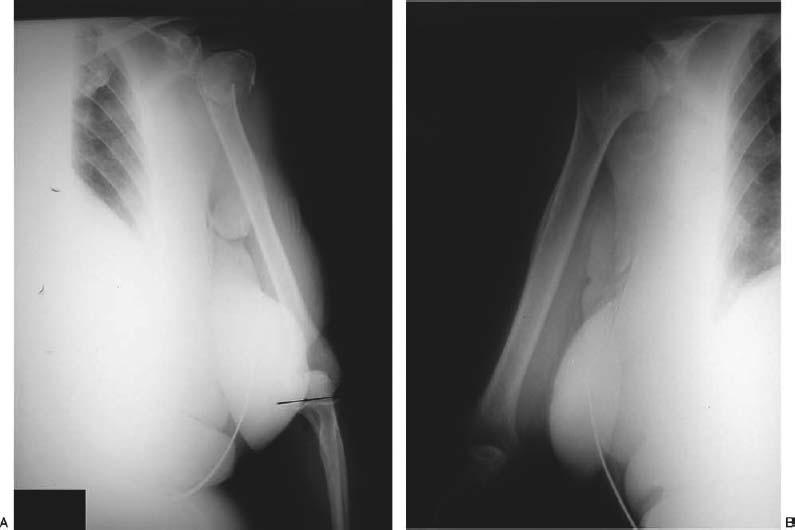
9 Arthroplasty for Proximal Humeral Fractures Complex fractures of the proximal humerus include three-and four-part fractures and fracture dislocations, intraarticular head splitting fractures, and chronic impression fractures. These injuries, which are historically quite rare, have become more common as the population ages and remains physiologically active. These injuries are generally the sequelae of low impact falls in elderly patients or high velocity trauma in younger patients, and are particularly disabling when they involve the dominant arm.1–3 Severe complications in these fractures are the result of associated vascular compromise, which occurs because of interruption of the ascending branch of the anterior humeral circumflex artery as it courses around the proximal humerus and enters at the tuberosities around the bicipital groove.4 These endosteal vessels are at risk in fractures that involve one or both tuberosities. Disruption of this major blood supply leaves the proximal humerus susceptible to avascular necrosis (AVN). Four-part fractures are particularly susceptible because they include disruption of both tuberosities and are associated with a high incidence of AVN ranging from 34 to 85%.5–8 In addition to vascular compromise, these fractures are often associated with significant comminution, which makes stable open reduction/internal fixation extremely difficult. Because of these factors, many surgeons have opted for a “wait-and-see” approach to treatment in some patients. The other treatment options have included closed reduction, open reduction with fixation, and hemiarthroplasty.2,6,7,9–12 Schai et al,6 in comparing the results of these treatments in a group of patients who had sustained four-part proximal humeral fractures, noted that hemiarthroplasty gave statistically significant better results than both open reductions and internal fixation or conservative care. In other series, conservative treatment had only a 5% successful outcome.7 Some authors have noted that four-part fractures treated acutely by hemiarthroplasty had significantly better results than those chronic four-part malunions treated later by arthroplasty.13–15 With all these factors considered, hemiarthroplasty is, in the acute setting, the procedure of choice for most displaced proximal humeral fractures at risk for malunion or vascular compromise.3,8,16–19 Hemiarthroplasty is indicated in many patients who are medically suitable for such extensive surgery and are able to carry out the long rehabilitation process that is mandatory for a successful outcome. In rare cases of very young patients with displaced proximal humeral fractures and in a small subset of patients who have impacted four-part valgus fractures, attempts at open reduction/internal fixation with minimal hardware are indicated.5,7,19,20 Minimal hardware is recommended so that if arthroplasty is necessary later the remaining soft tissue sleeve and vascularity to the humeral head will be preserved.5,14,21 Hemiarthroplasty is contraindicated in patients with medical frailty precluding surgery and those patients whose physical or mental condition makes them unable to comply with the required postoperative rehabilitation program. In the older patient group, indications for arthroplasty are not based on chronological age, but are based on the patient’s physiologic age, hand dominance, and activity requirements. In the younger patients an attempted open reduction/internal fixation is warranted to avoid prosthetic replacement and its associated complications. In these cases if AVN does occur, the tuberosities will be in a better anatomic position to facilitate conversion to a prosthesis. As with all traumatic injuries, a careful history and physical exam and appropriate radiologic studies are mandatory. A careful history and physical exam is performed to determine any comorbid factors that might affect the surgical procedure and/or the postoperative rehabilitation process. Figure 9–1 (A) Scaled x-ray of fractured proximal humerus. (B) Scaled x-ray of contralateral normal humerus. A thorough clinical examination of the shoulder is performed to determine the obvious deformity and neurovascular function. Special attention to the axillary nerve function and vascular compromise is important because many patients with complex proximal humeral fractures will have such injuries. Many patients with vascular injuries may have intact pulses distally due to the extensive collateral circulation around the proximal humerus. Deltoid contraction and sensory distribution may be tested and any vascular deficiency should be aggressively evaluated. Standard x-rays should include a trauma series, which includes a true antereroposterior view of the scapula, a transcapular “Y” view, and an axillary view. In most cases, these views will supply the necessary information about the fracture complex to determine configuration; however, in some cases where displacement remains uncertain, computed tomography (CT) scans can be helpful, especially in distinguishing three- and four-part fractures. CT scans may also be helpful in detecting any head splitting or articular component of the fracture. In an effort to reestablish proper height and length of the proximal humerus after hemiarthroplasty, we now routinely utilize full-length x-rays of both humeri to determine humeral length and properly use this measurement to help us later in recreating normal anatomy (Fig. 9–1). We utilize interscalene block anesthesia with supplemental general anesthesia when necessary. This allows for decreased use of anesthetic agents, especially in the older population. It also allows for significant pain relief postoperatively so that the patient may begin early physical therapy routines. A general anesthesia component is necessary for proximal muscle relaxation and eliminates discomfort of the patient lying in one position for extensive periods. The patients are placed in a modified beach-chair position with the back elevated between 30 and 40 degrees. The head is well supported in a headrest or in a commercially available shoulder table. The patient is placed at the lateral edge of the table to allow free mobility of the operative arm, allowing unrestricted humeral extension, adduction, and rotation to facilitate the intramedullary reaming and allow for proper prosthetic component placement. The arm is appropriately prepped and draped free. We utilize a long deltopectoral incision, which is performed from the anterior portion of the acromioclavicular (AC) joint along the coracoid process and following the anterior deltoid distally. The surgeon develops a deltopectoral interval preserving the cephalic vein. Appropriate deltoid retractors are utilized between the deltoid and the conjoined tendon. Care should be taken to avoid injury to the musculocutaneous nerve, which crosses inferior to the coracoid. This can be done by partially tenotomizing the conjoint tendon. The subacromial space is then cleared bluntly with gentle use of digital pressure or periosteal elevators. Proximal and distal deltoid insertion and origin are left intact and the pectoralis muscle tendon is retracted medially. The sternal head insertion may be partially released to decrease medial pull on the proximal shaft of the humerus and allow for better exposure. The fracture figuration is now exposed after hemorrhagic bursa and fracture hematoma is carefully excised. The biceps tendon is isolated and identified. This is a key surgical landmark that helps locate the tuberosity fragments because the fracture configuration is medial or deep to the exposure. The fracture line is found between the tuberosities slightly posterior to the bicipital groove. The intertubercular fracture line is followed proximally to the rotator interval, which is opened to allow better access to the tuberosities that can then be identified. The lesser tuberosity will be displaced medially and the greater tuberosity will be displaced posterior superiorly. In many cases, there are soft tissue attachments that must be gently freed utilizing periosteal elevators or osteotomes; however, care should be taken to avoid injury to the periosteal attachments. The cancellous portion of the isolated tuberosity fragments are often oversized and may need to be trimmed for reduction and repair later. The bone that is removed can be saved and used later as bone graft during tuberosity reconstruction. At this point three #5 nonabsorbable or fiber-wire sutures are placed at the bone tendon interface between the cuff and the bony surface of the greater tuberosity from proximally to distally. One traction suture is also placed at the bone tendon interface of the lesser tuberosity as well. Once control of the tuberosities has been achieved the humeral head is teased out of the glenohumeral joint. Sometimes this requires the use of osteotomes or periosteal elevators to release it from its soft tissue or bony attachments. The head fragment will then be measured using calipers or sizing guides to select the proper head size for later reconstruction. At this point with adequate exposure, the glenoid is evaluated for concomitant fracture or damage. In cases of severe damage, bone loss or even concomitant arthritis glenoid replacement might be considered. The long head of the biceps insertion into the glenoid is resected and the remaining stump removed. The remaining tendon will later be tenodesed to the soft tissue reconstruction. With the tuberosities retracted and the humeral head removed, the intramedullary canal is now exposed. The first critical step in prosthetic replacement is placement of the humeral component at the appropriate height (length) and version. This is a critical step in the operative process, which actually begins preoperatively. In some cases the humeral head will fracture at the articular surface making replacement at the appropriate height relatively easy. In other cases where there is significant proximal comminution, the surgeon must recognize the bone loss based on the findings of the preoperative x-rays, the intraoperative findings, and the evaluation of full-length scaled x-rays of the injured and contralateral humerus with a ruler of defined length. This information utilized in conjunction with either an external or intramedullary fracture sizing guide will ensure proper humeral length reconstruction. Many commercially available fracture arthroplasty systems will have associated extramedullary or intramedullary fracture placement guides, which will ensure proper height and fixation. Preoperative assessment of the proximal humeral comminution is also critical to allow the surgeon to place the humeral component at the proper height. Comminution of the medial humeral neck should be assessed and pieces measured to help identify the position in which the humeral component must be placed. The arm is extended and adducted to deliver the shaft anteriorly. The canal is now prepared with progressive hand-held sequential reamers.
Epidemiology and Mechanism of Injury
Treatment
Surgical Treatment
Indications for Surgery
Patient Assessment
Radiologic Assessment
Treatment
Surgical Treatment
Techniques
Anesthesia
Patient Positioning
Surgical Exposure
Identification and Mobilization of Fracture Fragments
Prosthetic Insertion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree