Arthrodesis and Resection Arthroplasty of the Hip
Michael J. Taunton and Robert T. Trousdale
Arthrodesis
Introduction
Operative arthrodesis of the hip is defined by any method that effectively fuses the ilium and the proximal femur, eliminating the hip joint and its motion. Thus, arthrosis of the hip joint and accompanying pain are eliminated.
Hip arthrodesis was a commonly performed procedure in the United States up until other forms of motion-sparing, pain-relieving reconstruction became available. However, with the advent of hip arthroplasty, each decade the number of hip arthrodeses decreases. Unfortunately for the young patient, the durability of current components of total hip arthroplasty cannot compete with patients’ lifestyle, and this often leads to revision. The success of total hip arthroplasty has improved in recent decades with quoted success of modern components in patients younger than 50 years of age to be 87% at 10 years for uncemented Harris Galante acetabular components,1 95% at 7 years for Exeter cemented femoral components, and 90% for an uncemented grit-blasted straight tapered titanium femoral stem at 20 years.2 Even with exceedingly favorable results, many patients younger than 50 will need at least one revision of total hip arthroplasty in their lifetime.
Preoperative discussion in patients with end-stage arthrosis of the hip younger than 40 years of age must include discussions of the pros and cons of salvage procedures such as arthrodesis. Although surgeons’ enthusiasm for the procedure and patients’ acceptance of fusion may be low, hip arthrodesis may be an important consideration in a select patient population with end-stage arthrosis of the hip. A properly positioned, fused hip joint can offer long-term pain relief and good function.3–6 However, as the results of total hip arthroplasty improve with further development of implants, bearing surfaces, and techniques, hip fusion may become even more limited. Discussions between patient and physician with the patient’s best interest in mind, combined with quality data, will continue to direct decision making.
Historical Perspective
In the United States in 1908, F. H. Ablee first discussed arthrodesis of the hip for advanced arthrosis in five patients.7 Indications for most early reports included tuberculous hips in younger patients and unilateral osteoarthritis in older patients. Arthrodesis was first used for old congenital dislocation by Heusner, by Lampugnani, and by Albert as early as 1885, according to Nové-Josserand.8 In the early 1900s, many methods of extra-articular arthrodesis were described.9–11 Ghormley, in 1931, and Henderson, in 1933, described their techniques of arthrodesis, used chiefly in tuberculous hips.12,13 Ghormley advocated a combined intra-articular and extra-articular arthrodesis and pointed out that the risk of spreading tuberculosis by opening the superior surface of the capsule was minimal. Henderson recommended clean removal of tuberculous tissue and combined intra-articular and extra-articular fusion for tuberculosis of the hip.
Trumble, in 1932,14 and Brittain, in 1941,15,16 described techniques for ischiofemoral arthrodesis. Brittain’s method of arthrodesis involved making a subtrochanteric osteotomy with special chisels and placing a tibial autograph strut from the subtrochanteric osteotomy into the ischium. Patients were kept in plaster cast immobilization for 4 months postoperatively.
In 1938, Watson-Jones advocated internal fixation of the femoral head to the pelvis by a long Smith-Petersen nail.17 This was later refined and described in combination with iliac grafting. Watson-Jones reported in 1956 an incidence of 94% sound bone fusion in 120 patients who had arthrodesis of the hip for osteoarthritis who had been observed for a minimum of 5 years.18,19 Immobilization in a double hip spica for at least 4 months was considered essential by these authors. Lange reported the largest series (500 patients) of the technique with 85% perfect results.20
Thompson and Cholmeley, both in 1956, advocated routine subtrochanteric osteotomy for all patients having arthrodesis of the hip.21,22 Both Thompson and Cholmeley concluded that success occurred more frequently when the grafting operation was combined with or followed by osteotomy. Thompson noted a 90% rate of union in those patients having combined hip fusion and osteotomy against a prior 26% rate of union in patients in whom fusion was attempted without osteotomy for osteoarthritis.22
Charnley, in 1953, advocated central dislocation of the femoral head in surgical arthrodesis of the hip and subsequently reported excellent or good results in 88% of 105 patients treated by this method. Even though many of his patients did not obtain fusion, they were included in the 88% good results.23 Medialization of the hip center lowered joint reaction forces across the hip by shortening the lever arm from the center of gravity. Schneider applied the concepts of Charnley’s arthrodesis and added the Cobra-headed plate arthrodesis.24
These reports and others had relatively short follow-up and focused on fusion rates with different intra-articular and extra-articular techniques with and without internal fixation. Many reports required prolonged immobilization in plaster cast for 6 weeks to 4 months to achieve fusion.
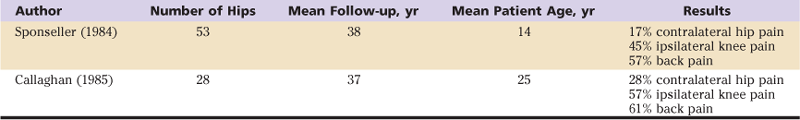
Callaghan and Sponseller were some of the first to report the long-term outcomes of patients with arthrodesis of the hip. Sponseller cited that 78% of patients were satisfied with the arthrodesis, and all were able to work; 57% had some low back pain, and 45% had knee discomfort. Only 13% had undergone total hip arthroplasty on the arthrodesed hip.6 Callaghan retrospectively reviewed 28 patients with an average follow-up of 38 years after arthrodesis through various techniques. About 60% of patients had pain in the ipsilateral knee, with onset on average 23 years after arthrodesis. Back pain was similar, with an average onset of 25 years after arthrodesis. Seventy percent of patients could walk farther than 1 mile. Based on their results, investigators believed that the optimal position for fusion was in approximately 5 degrees of adduction and 35 to 40 degrees of flexion. The authors concluded that a patient with an arthrodesis of the hip could function at a high level for many years and would be able to work at most occupations. Pain in the back and knee was a common sequela, especially at long-term follow-up. However, symptoms usually are not incapacitating and generally had their onset many years after the arthrodesis.4
Indications/Contraindications
Indications
• Monoarticular hip osteoarthritis, especially in a young, high-demand patient
• Hip arthrosis after fracture
• Unilateral end-stage avascular necrosis of the femoral head
• History of unilateral septic arthritis of the hip with end-stage arthritis
• Salvage of prior surgery (e.g., osteotomy)
• Unilateral hip dysplasia with end-stage arthritis
• Patients with contraindications to total hip arthroplasty (THA) with end-stage disease
• Muscular or neurologic deficiencies about the hip in the setting of end-stage arthrosis
Contraindications
Only after appropriate exhaustion of nonsurgical modalities, such as activity modification, anti-inflammatories, and the use of assistive devices, can an operative salvage procedure such as fusion be entertained. A strong indication for arthrodesis of the hip is a young patient (generally defined as 1 less than 40 years of age) who is healthy with high demands (such as a heavy laborer) and end-stage monoarticular osteoarthritis of the hip. Patients with neurologic or muscular abnormalities that would compromise the function of the abductor musculature after total hip arthroplasty may also be better suited for arthrodesis. Other relative indications include hip arthrosis after fracture, end-stage unilateral avascular necrosis of the femoral head, a history of unilateral septic arthritis of the hip with end-stage arthritis, salvage of prior surgery (e.g., osteotomy), unilateral hip dysplasia with end-stage arthritis, and other patients with contraindications to THA with end-stage hip disease.
Strong contraindications for arthrodesis of the hip include active infection, inflammatory arthritis such as rheumatoid arthritis or systemic lupus erythematosus, older patients with osteoarthritis that can be managed with total hip arthroplasty, and those with bilateral hip disease. Radiographs of the patient’s lumbar spine, contralateral hip, and bilateral knees should be obtained. Although early changes in back and knee arthritis are not an absolute contraindication, various authors have reported poorer results with spondylosis, gonarthrosis, and knee instability.4,25
Other relative contraindications include patients who are not able to comply with postoperative rehabilitation and limited weight bearing, especially the obese. The patient’s lifestyle must be taken into consideration. Those with a job or a desire for activity such as climbing, sitting for long periods of time, and repetitive stooping or squatting may not be best served by arthrodesis. The patient’s overall psychological condition should be assessed for tolerance of the procedure and rehabilitation.
Preoperative Planning
An important component of the preoperative plan is a precise and careful discussion of the options and expected functional outcome of the arthrodesis. The physician-patient relationship is very important in this situation for a positive outcome. Patients should be counseled that although the motion of the hip joint will be obliterated, they will be allowed to resume all activities. The reality of the salvage situation must be conveyed to enable the patient to have realistic and appropriate expectations after the procedure.
To help define the bony anatomy and any bony deformities that may be encountered at arthrodesis, enhanced radiographic evaluation is indicated. Routine standing anteroposterior (AP) pelvis, Judet, and AP and cross-table lateral views of the femur should be obtained. These films will allow the surgeon to assess leg length discrepancy, offset, rotation, and angular deformity. Additionally, the acetabular bone stock and points of fixation can be more readily assessed with Judet films. If the pelvic anatomy or bone deficiency is more complex, preoperative three-dimensional computed tomography (CT) reconstructions of the pelvis and proximal femur may assist the surgeon in proper positioning and fixation of the arthrodesis.
Routine preoperative laboratory tests should be obtained. However, in addition, erythrocyte sedimentation rate, C-reactive protein, and complete blood count with differential are advised in patients with a history of infection. If any of these tests are abnormal, preoperative hip joint aspiration with cell count and culture will help rule out chronic infection. Patients with remote histories of inflammatory disease may have to be evaluated by a rheumatologist and may need to be reconsidered for fusion if active inflammatory disease is present. Preoperative blood donation or intraoperative blood salvage may be indicated because blood loss may necessitate transfusion.
Description of Technique(s)
Positioning of the Hip Arthrodesis
Positioning of the arthrodesis has been developed as a position of the limb that best accommodates normal activities of daily living. Patients with unilateral hip fusion walk with a gait that is somewhat slow, asymmetrical, and arrhythmic. Compensation for absent hip motion is accomplished by increased transverse and sagittal rotation of the pelvis, increased motion in the sound hip, and increased flexion of the knee throughout the stance phase on the fused side.26–28 Positioning can have a large effect on the durability of the fusion and the joints adjacent to it.4 The optimal position of hip fusion is 5 to 7 degrees of adduction, 20 to 30 degrees of hip flexion, and 5 to 10 degrees of external rotation. Limb shortening is kept to a minimum. Gore and associates stated, “Relationships between the fusion position, certain physical traits, and walking performance suggest that the best gait can be expected in young patients who have free motion of the lumbar spine, the sound hip, and the knee on the side of fusion, and who have equal limb lengths and a hip fused in a position that includes excessive adduction.”27 It is important to note that Fulkerson found that in children with long-term follow-up, the fused hip can drift into excessive adduction over time. In these patients, it is advisable to fuse in neutral adduction.29,30 Activities that require hip flexion are most difficult for patients, who find that sitting in tight spaces such as airplanes is difficult. Additionally, simple activities of daily living such as donning and doffing socks and bending are troublesome. Some women may have difficulty with sexual activity. The patient and the surgeon must accept the limitations of the procedure and must position the fusion in the most functional and durable position.
Techniques
Anterior Plating Technique.
The modern anterior approach to arthrodesis described by Beaule and associates is done through an extended Smith-Petersen approach with the patient supine on a radiolucent table. Depending on the type of table used, the leg may be prepped free and supported intraoperatively for optimal positioning, or the leg may be held by the table in the proper position if a traction table is used. An incision is made from just superior-lateral to the anterior superior iliac spine to below the greater trochanter, lateral to the course of the lateral cutaneous femoral nerve. The fascia over the tensor fascia lata is incised and elevated off of the muscle medially. Tensor, sartorius, and rectus muscles are released from their insertions, and a complete anterior capsulectomy is performed. After the extended Smith-Petersen approach, the internal aspects of the ilium, hip, and proximal femur are well seen. The traction table can facilitate distraction and/or dislocation of the hip for preparation of the bony surfaces. The acetabulum is curetted and reamed, and a bleeding cancellous surface is obtained, if possible. The surface of the femoral head is likewise denuded and is shaped with female reamers, if available. A conforming fit of the femoral head and acetabulum is important for successful fusion. At this point, proper positioning of the hip joint is obtained, or it is re-evaluated for fusion. Flexion is checked and measured relative to the angle of the femoral shaft and the floor. The foot and the patella are used to judge rotation. Fluoroscopy is helpful to identify the horizontal axis, defined as a line between the anterior superior iliac spines. The mechanical axis of the femur can also be identified by fluoroscopy by a line subtended between the center of the femoral head and the center of the knee or the center of the weight-bearing dome of the talus. When the position is correct, a long 6.5 mm cancellous lag screw is placed from the lateral aspect of the greater trochanter to the femoral head into the ilium to obtain medialization and compression of the femoral head. A 12 or 14 hole 4.5 mm low-contact dynamic compression (LCDC) plate is then modeled to the anterior contour of the femur, pelvic brim, and proximal femur. The released vastus lateralis, rectus femoris, and sartorius muscles are reattached. The abductors are spared and pelvic deformity is minimized, making later conversion to THA less technically challenging. Bone graft may be added from the ilium or from allograft sources and placed around the site of fusion. Deep drains are placed, and the wound is closed in standard fashion.31
Screw Technique.
The procedure may also be carried out in a lateral position through an anterolateral approach. The patient is positioned in the lateral position on the traction table. An incision is made over the lateral aspect of the greater trochanter. The fascia over the greater trochanter is incised in line with its fibers. The anterior one third of the gluteus medius is elevated from the greater trochanter. The anterior capsule is excised. The leg is externally rotated, and the hip is dislocated anteriorly. The rectus is released, and the capsule is released to assist with retracting the femur for acetabular exposure. The acetabulum is curetted and reamed. The femoral head is prepared likewise. The hip is then relocated and is placed in proper position for arthrodesis. A guide pin for a fixed angle hip screw is inserted from the greater trochanter through the femoral head into the supra-acetabular bone. The path is drilled, and a hip screw of appropriate length is placed. The lateral side plate is placed in standard fashion, and the surfaces are compressed. Then three 6.5 mm cancellous screws are placed along the axis of the hip screw for added compression. Cancellous bone chips can be added around the rim of the femur and acetabulum for added osteoconductive potential. The abductors are reattached in standard fashion, and the wound is closed in layers. A double hip spica cast is placed and kept for 3 months. The fusion is re-evaluated at that time and is converted to a single leg spica for an additional 4 to 6 weeks.
Postoperative Care
Standard postoperative antibiotics are maintained for 24 hours. Drains are removed when output has declined to less than 50 mL over 8 hours. Deep venous thrombosis prophylaxis should be maintained with a comprehensive protocol as with total hip arthroplasty, including but not limited to mechanical and dynamic compression garments and chemical thromboprophylaxis. Whether casting has been chosen or not (based on the rigidity of internal fixation and surgeon preference), weight bearing should be limited to no more than 30 lb for the first 6 to 8 weeks. If not treated with a cast, the patient should not sit at any angle greater than 60 degrees so as not to stress the fixation of the fusion. AP and lateral radiographs of the pelvis are obtained at 3 months to assess the fusion, and every 6 weeks thereafter until fusion is obtained. Activity and weight bearing are progressed when bony fusion has been achieved and pain has subsided.
Results
In Callaghan’s review of 28 Iowa patients who had been fused from 1923 to 1966 with a variety of techniques, and with an average follow-up of 35 years, 22 of the 28 remained fused; in 6, the arthrodesed hip had been converted to total hip replacement. Average age at fusion was 25 years. Low back pain was present in 61%, and knee pain was present in 57%. Arthrodesis reliably relieved patients’ pain but limited lifestyle to some degree. Patients fused in abduction had more back pain than those fused in neutral or adduction (78% vs. 50% to 60%). Additionally, those fused in adduction had a lower rate of knee pain and radiographic changes in the knee than those fused in abduction (43% vs. 78%). Patients fused in a more flexed position (average 33 degrees) tended not to have back pain compared with those fused in a less flexed position, who had back pain (average 29 degrees). Most patients were unsure whether in hindsight they would have preferred a total hip arthroplasty or an arthrodesis (Table 59-1).
Table 59-1
Long-Term Results of Hip Arthrodesis
With more modern fusion techniques and with a group of primary fusion and re-fusion patients, Brien reviewed 16 patients who had undergone hip arthrodesis utilizing an anteriorly placed compression plate an average of 4.5 years after surgery. The rationale for the anteriorly based plate is that future conversion to total hip arthroplasty should be considered at the time of planning for hip fusion. Rates of conversion to THA range from 13% to 21%.4,6 In this study, 63% of patients failed to unite, and 100% of those were re-fusions. Half of those with pseudarthroses were accepted by patients, and few significant restrictions in functional activities were reported.25 However, in a retrospective review by Matta, at an average follow-up of 25 months, 83% achieved solid fusion by clinical and radiographic criteria. Seventy-five percent of patients in that study had no or minor restrictions when participating in their former sports activities, and half regained the ability to work at their former jobs or in new occupations.32
Complications
Today, the major complication of arthrodesis may be patient dissatisfaction. Most patients know or have seen someone with a total hip arthroplasty and desire that level of function and hip motion. An open conversation about the procedure is very important. Proper patient education, combined with excellent surgical technique, may decrease this concern. Fusion position adjustment, based on the patient’s daily activity and interests, may enhance acceptance of an arthrodesis. Some authors have suggested a trial of spica casting before arthrodesis to “test out” the position and make modifications to the position preoperatively.
Malunion is the major complication of hip arthrodesis. Modern reports cite a high rate (≈80% to 90%) of union with modern techniques.31,32 However, Brien found that patients with previous failed fusion or bone loss have a high risk of nonunion.25 A single plate may not be adequate to neutralize forces across the hip joint, particularly in cases such as multiply operated hips, re-fusion, or avascular necrosis, when the contact surface area between the femoral head and the acetabulum is reduced. In these cases, supplemental fixation with lateral plates and additional bone graft may be indicated.25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








