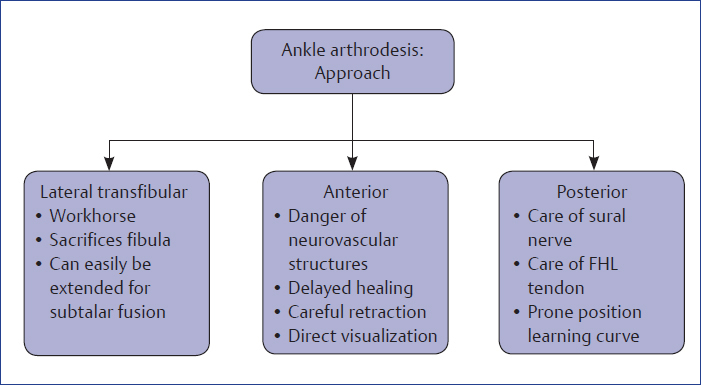
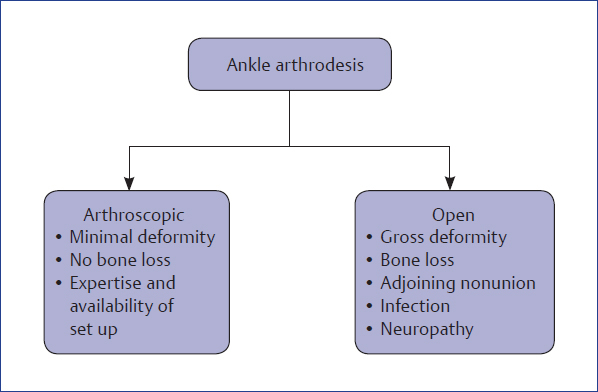
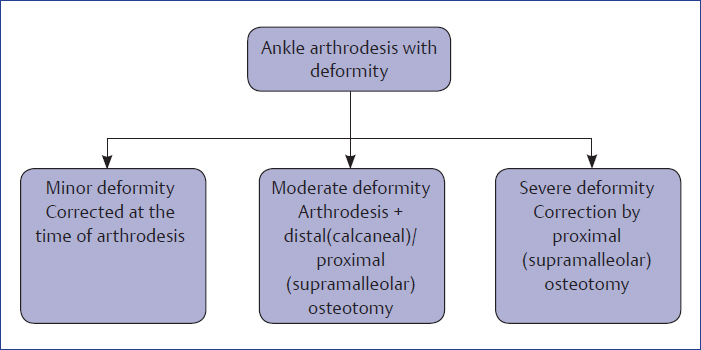
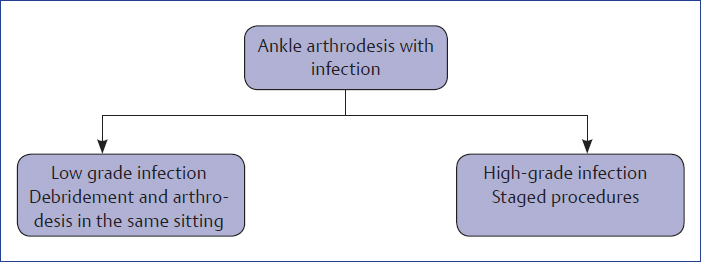
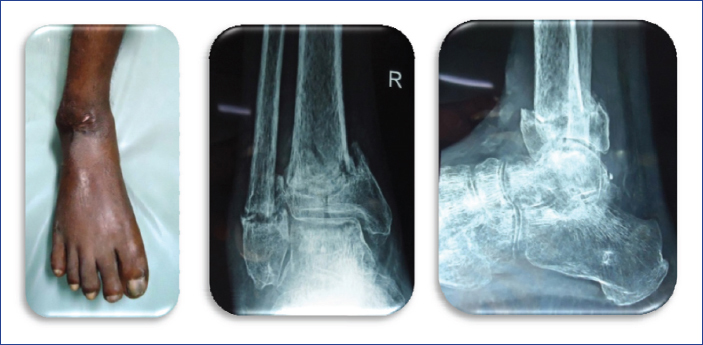
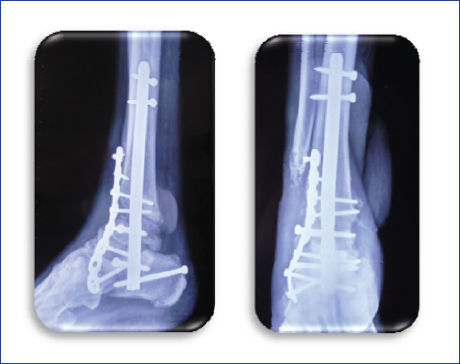
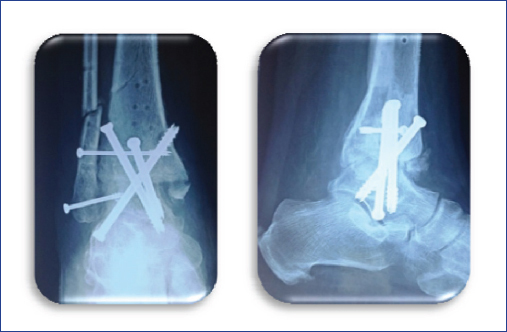
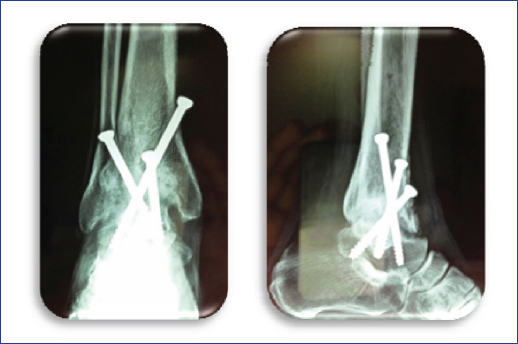
Chapter Arthrodesis is an art, let us live it! The aims of arthrodesis are as follows: ♦ Creation of broad, cancellous, bleeding surfaces ♦ To restore a plantigrade foot ♦ Rigid fixation and compression across the arthrodesis site ♦ Filling of defects with bone grafts or bone substitutes ♦ Augmentation of healing if needed using orthobiologics ♦ Generous release of soft tissues and soft tissue balancing ♦ Correction proceeds from proximal to distal ♦ Arthrodesis is always done in a corrected position ♦ Removal of bone to correct deformity must precede removal of articular cartilage ♦ Release of tendo Achilles or contracted muscles must accompany arthrodesis, if needed ♦ Tissue force balancing by suitable tendon transfer may be required as an adjunct procedure ♦ Spare as many joints as you can ♦ Drilling of articular surface is done to increase vascularity ♦ Feathering of arthrodesis surfaces is done to increase the vascularity ♦ Arthrodesis in grossly infected cases shall follow generous debridement ♦ Arthrodesis in low-grade infection cases can be done as a single-stage procedure where debridement precedes arthrodesis ♦ Use of plate and screws is justified in cases with good bone stock and good soft tissue envelope ♦ Use of external or ring fixator is justified in cases with poor bone stock, poor soft tissue envelope, and comorbid conditions ♦ For a case with nonunion, fusion mass must extend to stabilize nonunion site ♦ Proximal or distal corrective osteotomy will be needed as an adjunct procedure in cases with severe deformity ♦ In neuropathic fusions, longer and stronger combination fixations are used. These fixations must cross multiple joints to augment stability ♦ Neuropathic arthrodesis needs extended period of immobilization and no weight bearing. Postunion protection with brace is done for a long duration ♦ Use of lamina spreaders of various sizes and Hintermann retractor of various sizes is a must for midfoot and forefoot arthrodesis Position: Position of fusion is neutral dorsi/plantar flexion, 5° to 10° of external rotation of foot with hindfoot in neutral; 5°of valgus with talus slightly posterior. The specific indications for arthroscopic ankle arthrodesis and open-ankle arthrodesis are mentioned in Flowchart 14.1. Flowchart 14.1 Indications for arthroscopic and open ankle arthrodesis. Ankle for arthrodesis could be approached anteriorly, posteriorly, or laterally (Flowchart 14.2). Depending on the severity of the deformity, arthrodesis procedure changes with the addition of other adjuvant procedures (Flowchart 14.3). Flowchart 14.3 Ankle arthrodesis with deformity. In case of associated infection, treatment of infection is done prior to arthrodesis (Flowchart 14.4). Flowchart 14.4 Ankle arthrodesis with infection. ♦ Always assess preoperative movements of transverse tarsal and subtalar joint ♦ Assess vascular status of the limb ♦ Assess the neurological status of the limb ♦ Vascularity of the talus must be confirmed preoperatively for successful fusion (Fig. 14.1) Fig. 14.1 X-ray showing ankle arthritis with avascular talus. ♦ Presence of deformity must be noted and corrected during ankle fusion (Fig. 14.2) Fig. 14.2 X-ray and clinical picture of a case showing gross varus deformity with ankle arthritis. ♦ Tendo Achilles tightness must be assessed and, if needed, release of tendo Achilles should be done ♦ Previous scars and badly healed incisions would mandate change of approach (Fig. 14.3) Fig. 14.3 Clinical and radiological pictures of a case with poor skin condition on the lateral aspect of ankle mandating anterior approach for fusion. ♦ Poor host conditions such as diabetes, medical comorbidities, and osteoporosis shall be dealt with augmentation, additional fixations, external fixation, prolonged protection over and above medical management (Fig. 14.4) Fig. 14.4 Diabetic ankle fusion done with hindfoot nail with addition of plate. ♦ Care of subcutaneous nerves must be taken while doing surgery to prevent future neurological complications ♦ Take full-thickness flaps and avoid vigorous retraction of soft tissues ♦ Excision of anterior osteophytes of tibia is a must (Fig. 14.5) Fig. 14.5 X-ray showing ankle arthritis with anterior osteophyte. ♦ Transfibular approach is preferred as far as possible ♦ Fibular osteotomy is done 2.5 cm above lateral malleolus and fibula is cut in a proximal lateral to distal medial direction ♦ Fibula should be used as a biological plate and is fixed with two 4 mm screws, one in tibia and the other in talus (Fig. 14.6) Fig. 14.6 AP and lateral projections of a case operated by transfibular ankle fusion in a case of infected ankle arthritis. Fibula is used in this case as a biological plate. ♦ Compression at arthrodesis site must be generated before placement of plate ♦ All screw threads should cross the arthrodesis site ♦ Crossing of compression screws should not be at the level of arthrodesis site ♦ For cases with minimal deformity and no bone loss, arthroscopic ankle fusion is the best alternative ♦ Try to save the fibula in younger patients for feasibility of future total ankle replacement (Fig. 14.7) Fig. 14.7 Case where fibula was preserved for possibility of future ankle replacement.
14
Art of Arthrodesis in Foot and Ankle
Principles of Arthrodesis
Tips and Tricks
Ankle Arthrodesis
Tips and Tricks



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree