15
Anterior Cruciate Ligament Reconstruction: Quadriceps Tendon Autograft
More than 100,000 anterior cruciate ligament (ACL) reconstructions are performed annually in the United States with good to excellent results. Debate exists regarding the ideal graft source because of the potential for graft harvest morbidity. Patellar tendon, hamstring tendon, and allografts are the most commonly used grafts. Ipsilateral quadriceps tendon, although less commonly used, is an excellent graft choice.1–6
Surgical Indications and Therapeutic Options
Patients who have symptomatic knee instability due to an ACL tear are candidates for reconstruction. Physical therapy to reduce swelling and regain motion and muscle tone is completed prior to surgery. Patients without functional instability or older patients who elect a less active lifestyle may be treated conservatively with bracing and exercise.
Surgical Techniques
A careful examination under anesthesia of both injured and uninjured knees is performed. Particular attention is given to accessing the lateral and posterior lateral stabilizers of the injured knee.
Diagnostic Arthroscopy
A thorough diagnostic arthroscopy is performed. Careful attention is given to the menisci and articular surfaces, and any needed repairs are completed prior to ligament reconstruction. The tear of the ACL is defined.
Graft Harvest
A 3 cm transverse incision is made at the superior pole of the patella, and a plane is developed between the subcutaneous tissue and the quadriceps tendon. The dorsal aspect of the patella is exposed in preparation for the patellar bone plug harvest. Starting immediately adjacent to the vastus medialis oblique (VMO) and 7 to 8 cm above the patella, the quadriceps tendon is excised straight down onto the patella, cutting through about 70 to 80% of the thickness of the tendon but trying to stay out of the suprapatellar pouch. A parallel longitudinal incision 10 mm lateral to the first incision is made and carried onto the patella. A small oscillating handsaw is used to harvest a patella bone plug 7 mm wide by 25 mm long. Angling the bone about 20 degrees produces a trapezoidal graft. Prior to removing the bone plug, it is drilled to accept two No. 2 Ethibond sutures (Ethicon, Somerville, NJ). The bone plug is gently lifted from the patella with a small osteotome.
Keeping tension on the graft, the tendon is dissected off the superior pole of the patella until a layer of fat is encountered. This fat marks the level between the vastus intermedius tendon and the synovium. Dissection is then carried proximally using transverse strokes with a No. 10 blade just anterior the undersurface of the quadriceps tendon for 2 to 3 cm. The tendon harvested should be 7 to 8 mm thick at this level (Fig. 15-1). The bone plug is sized to a 9 mm size, and two No. 2 sutures are passed through the hole in the bone plug. Scissors are then used proximally and longitudinally along the previous longitudinal quad tendon incision lines to free the graft to a length of 90 to 100 mm. The scissors are then turned 90 degrees, and the graft is amputated. The defect in the quadriceps tendon is then closed with a running No. 1 absorbable. The suture is saved for later closure of the bursal tissue over the bone-grafted patellar defect.

Figure 15-1 Quadriceps tendon harvest through a 3 cm transverse incision.
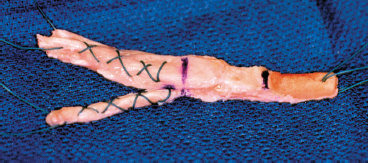
Figure 15-2 Split quadriceps tendon graft prepared with a nonlocking whipstitch No. 2 suture.
Graft Preparation
With tension on the graft’s two ends, the plane between the rectus femoris and vastus intermedius tendons is then developed with a pair of Metzenbaum scissors, leaving about 3 cm of the tendon unsplit. Each of these two limbs are then secured separately using five throws of a nonlocking whipstitch of No. 2 suture (Fig. 15-2). The entire graft is sized. Typically the tendinous portion of the graft passes through a 10 or 11 mm sizer and the bone plug through a 9 mm sizer. An interference screw guide pin is then placed between the split tendinous limbs, through the center of the quad tendon graft until it impacts the bone plug. The junction between the bone plug and the tendon is then marked.
Notchplasty
A standard notchplasty is completed, taking only enough bone and soft tissue to ensure good visualization and no impingement of the graft.
Tunnel Location
The tibial tunnel is then placed using a guide set between 45 and 55 degrees. The guide pin should enter the joint in the posterior foot print of the tibial footprint of the ACL and adjacent to the posterior aspect of the anterior horn of the lateral meniscus halfway between the posterior cruciate ligament (PCL) and the lateral femoral condyle (Fig. 15-3). Once this location is confirmed, a 1.5 cm incision is made on the proximal-medial tibia to allow for passage of the guide pin. The appropriate-size tibial tunnel is then reamed and the distance from the articular surface to the skin measured using a ruled depth gauge to allow for later aperture fixation of the tibial interference screw. A trocar-tipped guide pin is then placed through the tibial tunnel and impacted 3 mm anterior to the overthe-top position at the superolateral corner of the notch. This creates a divot to mark placement of the femoral guide pin. The knee is then flexed to 95 degrees and the femoral guide pin drilled bicortically through the tibial tunnel (Fig. 15-4). A 30 mm femoral tunnel is made with an acorn reamer.
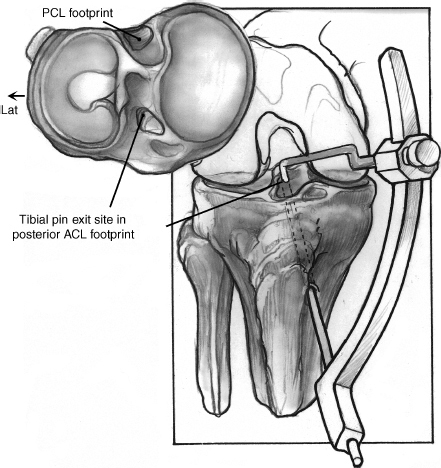
Figure 15-3 Placement of the tunnel location using a guide pin.
Femoral and Tibial Fixation
A ball-tipped manual burr inserted through the tibial tunnel is used to remove any sharp edges from the femoral tunnel and to check for impingement of the graft. A curette is used to create a notch at the superior aspect of the femoral tunnel to allow for passage of the bioabsorbable interference screw guide pin. A long Beath-type pin with an eyelet is passed through the tibial tunnel up and through the femoral tunnel with the knee hyper-flexed. This pin passes out the anterior lateral thigh, and the pullout suture through the bone plug is pulled through the knee using this pin. The graft is pulled into place and the bone plug seated in the femoral tunnel to its marked depth (Fig. 15-5). A low straight stab wound is made through the patella tendon with a No. 15 knife blade, and a guide pin is placed beside the bone plug into the superior notch of the femoral tunnel. A dilator and tap are used to prepare for a 7 × 23 mm bioabsorbable screw, which is inserted along the guide pin through the patella tendon stab wound. Hyperflexion of the knee aids in placing the screw parallel to the bone plug. Fixation of the plug is checked by pulling tension on the sutures on the tendinous ends of the graft. A 9 × 28 mm bioabsorbable screw is used to fix the tibial side of the graft and is placed in over the guide pin that was placed initially in the tendinous portion of the graft. (Screw diameter can be increased if needed to obtain a tight fit in the tibial tunnel). The screwdriver is inserted to a depth equal to the aperture measurement of the tibial tunnel (Fig. 15-6).
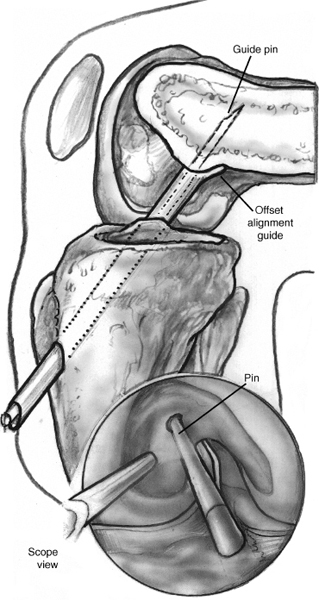
Figure 15-4 Femoral guide pin drilling bicortically through the tibial tunnel.
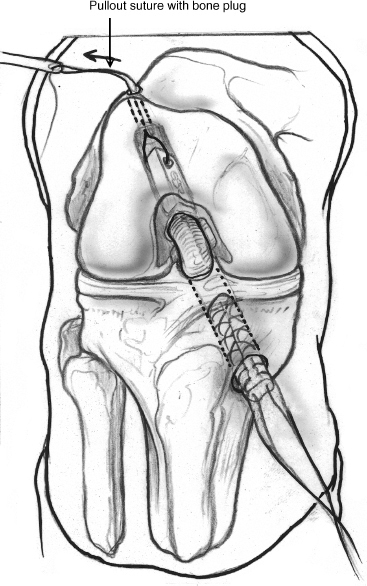
Figure 15-5 Pullout suture with bone plug.
Closure and Dressings
Bone graft from the trimmed bone plug and tibial reamings are impacted into the patellar defect, and the bursal tissue is closed over it using the remaining No. 1 suture from the extensor mechanism closure. The transverse graft harvest incision and the tibial tunnel incision are closed with buried interrupted 2–0 absorbable suture and Steri-Strips. A sterile cotton gauze dressing is applied, and the patient is placed in a knee immobilizer.
Weight Bearing and Rehabilitation
Aggressive closed chain exercises are begun on postoperative day 1. Patients are allowed to do touch-down weight bearing with two crutches for the first 3 weeks. They are advanced to one crutch at 3 weeks postoperatively and then can discontinue the crutches after 6 weeks.
Tips and Tricks and Avoiding Pitfalls
The quadriceps tendon is 8 to 9 mm in thickness. The belly of a No. 10 blade is about 7 mm. This is a useful guide to prevent inadvertent entry into the suprapatellar pouch during harvesting.
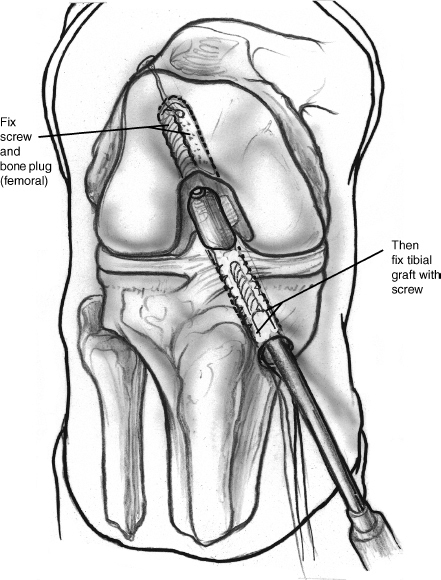
Figure 15-6 A fix of the femoral plug and tibial graft.
A thin fat layer exists between the vastus intermedius tendon and the synovium. Dissection should be taken just anterior to this plane to remain extraarticular and to preserve 1 to 2 mm of tendon posteriorly for later closure. If an inadvertent puncture wound is made in the suprapatella pouch, careful closure of it is performed when the defect in the tendon is closed.
Reamings from the tibial tunnel can be saved for bone graft.
The length of the tibial tunnel should be measured to allow for aperture fixation.
A low stab incision through the patellar tendon and hyperflexion of the knee facilitate coaxial placement of the femoral interference screw.
Conclusion
The quadriceps tendon graft is 7 to 8 mm thick, compared with a 4 mm-thick patella tendon. Quadriceps tendon graft harvest produces fewer anterior knee symptoms postoperatively. The infrapatella branch of the saphenous nerve is spared.
References
1 Blauth W. Die zweizugelige Ersatzplastik des vorderen Kreuz-bandes aus der Quadricepssehne. Unfallheilkunde 1984;87:45–51
2 Fulkerson JP, Langeland R. An alternative cruciate reconstruction graft: the central quadriceps tendon. Arthroscopy 1995;11:252–254
3 Harris NL, Smith DAB, Lamoreaux L, Purnell M. Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: Morphometric and biomechanical evaluation. Am J Sports Med 1997;25:23–28
4 Howe JG, Johnson RJ, Kaplan MJ, et al. Anterior cruciate ligament reconstruction using quadriceps patellar tendon graft. Part I: Long-term followup. Am J Sports Med 1991;19:447–457
5 Marshall JL, Warren RF, Wickiewicz T, Reider B. The ACL: a technique of repair and reconstruction. Clin Orthop Relat Res 1979;143:97–106
6 Staubli HU. The Knee and the Cruciate Ligaments. New York: Springer-Verlag; 1992:447
< div class='tao-gold-member'>









