Anterior Cruciate Ligament Reconstruction in Children and Adolescents
Craig Finlayson
Adam Nasreddine
Mininder S. Kocher
The knee is the most common site of injury in the skeletally immature athlete (1). The incidence of anterior cruciate ligament (ACL) tears appears to be on the rise. The treatment of these injuries is controversial. Nonoperative management can lead to functional instability and difficulty with cutting and pivoting sports. Additionally, the pathologic shear forces are associated with meniscal and chondral damage over time. ACL reconstruction in children and adolescents risks iatrogenic injury to the physis. This chapter reviews the historical perspective of ACL injuries in the young patient, clinical and diagnostic findings in children, treatment options, and results of treatment.
HISTORICAL PROSPECTIVE
The ACL is the principal intra-articular stabilizer of the knee. As in adults, an ACL injury in a child or an adolescent is usually a noncontact valgus injury. Prior to the 1980s, these injuries were thought to be rare in the pediatric athlete. Advances in diagnostic imaging and improved clinical acumen have allowed physicians to identify midsubstance ACL tears in patients with open physis (2, 3, 4, 5). A Finnish population-based cohort of 46,472 adolescents was followed for 9 years, and the incidence of ACL tears was reported to be 60.9 per 100,000 person years. Gender and activity level were identified as risk factors for ACL injuries. The relative risk of ACL injury for a young athlete participating in sports four times per week was 4 for males and 8.5 for females (6).
The results of nonoperative management in children are consistently associated with poor outcomes (7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17). Aichroth et al. reported on 23 children who were treated nonoperatively between 1980 and 1990. At final follow-up, meniscal tears were present in 15 knees, three osteochondral fractures occurred, and osteoarthritic changes developed in ten knees (11). From 1980 to 1985, McCarroll followed 16 patients under the age of 14 with open physes and midsubstance tears of the ACL treated without reconstruction. Six patients underwent arthroscopy for meniscal tears. Only seven patients returned to sports, all experiencing recurrent episodes of giving way, effusions, and pain (14).
Early attempts at primary repair of the ligament in children were unsuccessful (9,18, 19, 20). Engebretsen et al. presented eight adolescents who were followed 3 to 8 years after primary suture of a mid substance rupture of the ACL. Only three patients had good function, and five were functionally unstable. DeLee et al. examined three children <14 years old treated by primary surgical repair at 21 months postoperatively. All three patients had clinical evidence of ACL laxity. Two of the three had recurrent giving way. Failure of primary repair has led to the development of a variety of procedures to stabilize the knee. Surgical options include transphyseal, partial transphyseal, and physeal-sparing reconstructions.
TIBIAL SPINE FRACTURES AND PARTIAL ANTERIOR CRUCIATE LIGAMENT TEARS
It is important to understand the different types of injuries that can occur in the skeletally immature patient. Partial ACL tears and avulsion fractures of the tibial spine are more common in the pediatric population (21). Excellent functional results have been reported following arthroscopic reduction and internal fixation of tibial spine fractures, although long-term follow-up does demonstrate some residual laxity, indicative of associated intrasubstance injury to the ACL (2,22,23). Many partial tears can be treated nonoperatively (24). Based on a prospective study of arthroscopically confirmed partial ACL tears, failure of nonreconstructive treatment has been associated with tears >50%, tears of the posterolateral bundle, older skeletal age, and presence of a pivot shift.
HISTORY AND PHYSICAL EXAM FINDINGS
Important history questions include
How did the injury occur?
Was there contact with another athlete?
Was there a fixed position of the foot and rotation or twisting movement?
Were you able to continue to compete?
Was there significant swelling directly after the injury?
Have there been previous injuries to the knee?
Our understanding of ACL tears in the setting of younger athletes has changed considerably. The tibial spine fracture was once thought to be the pediatric equivalent of an ACL tear. Midsubstance ACL ruptures are now diagnosed more frequently in pediatric athletes participating in cutting and contact sports. The typical presentation is a young athlete who has a decelerating, twisting injury. Approximately two thirds of ACL injuries occur by noncontact mechanisms (25). The patient will often report a “pop” and the inability to return to the field. A large amount of swelling due to hemarthrosis is expected. The presentation is less dramatic in athletes who have had a prior partial tear of the ACL.
The findings on physical exam are dependent on the timing in relation to the injury. Directly after the injury, the stability of the knee can be tested on the sideline. The Lachman and pivot shift are positive before swelling and guarding occurs. When the patient presents for evaluation in the emergency department or clinic, the knee is typically swollen, compromising the ability to perform an accurate physical exam. Rates of ACL injury are reported between 10% and 65% in pediatric patients presenting with traumatic hemarthrosis of the knee; therefore, young athletes presenting with a hemarthrosis of the knee should raise suspicion for an ACL tear (26, 27, 28, 29, 30). The differential diagnosis of hemarthrosis of the knee includes patellar dislocation, meniscal tear, osteochondral fracture, tibial spine fracture, and epiphyseal fracture of the femur or tibia.
A thorough examination of the knee must be performed to rule out concomitant injuries. Associated injuries include meniscal tears, posterior cruciate, and/or collateral ligament tears, osteochondral fractures, and physeal fractures of the distal femur or proximal tibia. Given the higher prevalence of generalized ligamentous laxity in skeletally immature patients, a direct comparison to the contralateral knee should also be made.
IMAGING
Evaluation of the knee by magnetic resonance imaging (MRI) is an important part of the assessment, particularly in children. The MRI is useful to distinguish between partial tears, avulsions, and midsubstance tears of the ACL. Secondary findings in an acute injury include hemarthrosis and the presence of a bone contusion at the posterior lateral tibial plateau and anterior lateral femoral condyle. The MRI is useful for confirming the diagnosis of ACL tear, ruling out associated injuries, and assisting in preoperative planning (Fig. 31.1).
INDICATIONS AND TIMING OF SURGERY
Indications for ACL reconstruction in a skeletally immature patient include complete ACL tear with functional instability, partial ACL tear that has failed nonoperative treatment, and ACL injury with associated repairable meniscal or chondral injury. Due to higher rates of postoperative stiffness, acute ACL reconstruction is not recommended for isolated ACL tears (31). Surgery is typically delayed 3 weeks from the time of injury or until adequate range of motion has been achieved. Patients must be mature enough to participate in the extensive rehabilitation process following ACL reconstruction.
TREATMENT OPTIONS
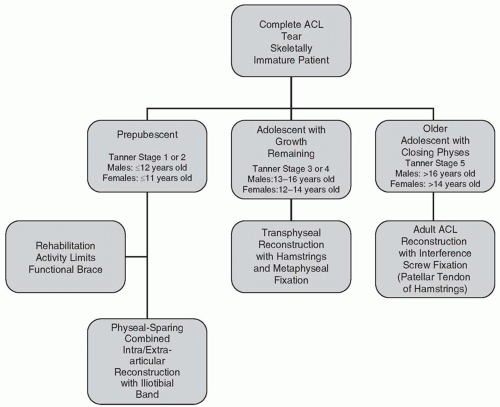
The choice of surgical technique is dependent on the physiologic age of the patient and the amount of growth remaining. For prepubescent children, violation of the tibial and femoral physis presents a risk of significant growth disturbance that would require limb lengthening or osteotomy. Animal studies have demonstrated a risk of physeal arrest with transphyseal ACL reconstruction (32, 33, 34). A number of clinical reports have documented growth disturbances following ACL reconstruction in this age group (35, 36, 37). Radiographs and developmental findings are used to determine the physiologic age. Referencing radiographs of the left wrist to the atlas of Greulich and Pyle (38) provides an efficient means to determine skeletal age. Roche et al. (39) referenced radiographic patterns of maturation of the knee to develop a formula for knee-specific estimates of skeletal age, but this system is less widely used. The physiologic age is based on the Tanner staging system (40) (Fig. 31.2; Table 31.1).
TABLE 31.1 Tanner Staging Classification of Secondary Sexual Characteristics | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|