CHAPTER 7 Anatomy, Evaluation, and Operative Setup for Posterior Ankle Arthroscopy
Arthroscopy of the posterior ankle was originally described as a diagnostic tool. As surgeons became more proficient with the technique, therapeutic procedures were incorporated.1–5 The posterior portion of the ankle is often poorly visualized from traditional arthroscopic portals, and certain lesions are more easily dealt with by performing a dedicated posterior arthroscopy. Although the prone position and the proximity of the tibial neurovascular bundle have led some away from the technique, recent articles demonstrate that the procedure can be undertaken safely.6
ANATOMY
The sural nerve lies lateral to the Achilles tendon at a distance of approximately 1 cm form the lateral edge of the Achilles tendon at the level of the posterolateral portal. It courses obliquely away from the Achilles as it heads toward the lateral portion of the foot. Medially, the flexor hallucis longus (FHL) tendon is encountered first when moving from the margin of the Achilles tendon. Immediately adjacent to that is the tibial nerve. Further medially and anteriorly lie the posterior tibial artery and vein (Fig. 7-1).
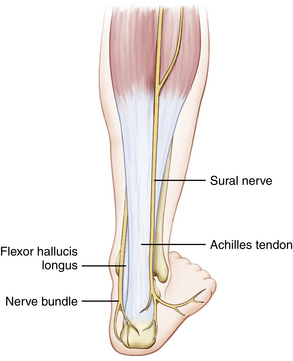
FIGURE 7-1 In the drawing of the surface and subcutaneous anatomy, notice the course of the sural nerve.
Retrocalcaneal bursitis is primarily treated nonoperatively, but refractory symptoms can be treated with bursa excision through the arthroscope. The normal bursa is encountered routinely in posterior arthroscopy, because it is often the first potential space developed.
CLINICAL EVALUATION
Retrocalcaneal Bursitis
Retrocalcaneal bursitis is a disease of the tissue adjacent to the insertion of the Achilles tendon on the calcaneus. Some authorities think that it part of a spectrum of disease that includes calcific insertional Achilles tendinitis and that it is not as much an inflammatory phenomenon as it is a fibroproliferative disease of the Achilles insertion, akin to lateral epicondylitits.5 A prominent posterosuperior part of the calcaneus (i.e., Haglund’s deformity) contributes to the symptoms is some patients.2,3,7,8
Watson and colleagues8 described a series of patients with retrocalcaneal bursitis with or without calcific insertional tendinitis. They found that patients without obvious insertional disease fared better than those with a spur. There was a 93% satisfaction rating, with an average time to maximal improvement of 5 months.8
Os Trigonum Syndrome
Nonoperative treatment consists primarily of immobilization and nonsteroidal anti-inflammatory medications. Casting for a period of 4 to 6 weeks with regimented anti-inflammatory medications can relieve symptoms in most patients. For those with recurrent or recalcitrant symptoms, excision of the os trigonum can alleviate pain. Open excision has long been used successfully, but there have been complications related to infection and hematoma.9
Great success with arthroscopic excision has been reported.2–4 Scholten and colleagues thought they were better able to address soft tissue impingement syndromes with posterior arthroscopy. They followed 55 patients for a minimum of 2 years, with none lost to follow-up. They found a significant increase in the American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot score (75 to 90) and no degenerative changes on repeat radiographs.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








