CHAPTER 72 Adult Isthmic Spondylolisthesis
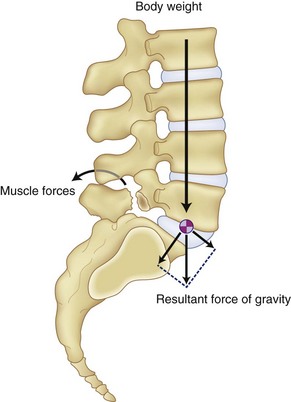
Spondylolisthesis by definition is an anterior or posterior translational displacement of one vertebra on another. In the adult, this occurs in the lumbar spine as a result of defects in the bony architecture, trauma, or degeneration.1–3 Due to the body’s center of gravity being anterior to the lumbosacral joint, slippage occurs as the lumbar spine rotates around the sacral dome. The age of the patient when these defects occur and the individual’s sagittal alignment of the spine determine to what degree the deformity progresses.
Classification/Natural History
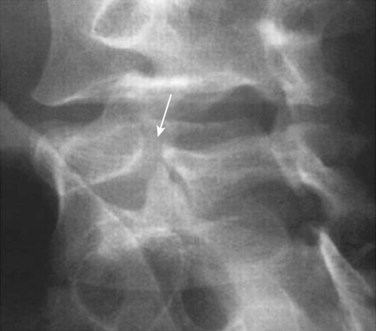
Adult spondylolisthesis presents in predominately two patterns: the isthmic variety, which involves abnormalities of the pars intra-articularis (Fig. 72–1), and the degenerative variety, which occurs as a result of lumbar spondylosis with its disc degeneration and instability causing a physiologic unwinding of the facets in the sagittal plane.4–6 (Fig. 72–2) This section concentrates on the isthmic variety.
Fredrickson and colleagues7 prospectively followed 500 elementary students and found a 4.4% incidence of spondylolysis and a 2.6% of spondylolisthesis at age 6. After reaching adulthood, the incidence of spondylolysis was 5.4% and spondylolisthesis was 4%. Healing of the pars did not routinely occur and slippage occurred throughout both decades covered, with the greatest change occurring during the adolescent years.
Pathophysiology
Incidence
The incidence of defects in the pars interarticularis or isthmic variety of spondylolisthesis is 4% to 6% in the general population.8–10 It is more common in males and more common at the L5-S1 level. Fifty percent present with only spondylolysis with no slippage. Even though the rate of occurrence is lower in females, when it occurs, there is a tendency for a higher rate of progression of the slippage. The pars defect usually occurs between 5 and 7 years of age and is not seen until erect posture is achieved. The incidence varies according to race with 6.4% in white American males, 2.8% in black males, 2.3% in white females, and 1.1% in black females. Eskimos have been shown to have a rate as high as 50%.11 A genetic tendency has also been shown to exist in patients with spondylolysis with a higher incidence than normal being reported in other family members.12 Slippage occurring as a result of degenerative etiology is more common in females older than the age of 40.
Mechanism of Injury
Spondylolisthesis as a result of defects in the pars intra-articularis has been subdivided into three categories by Wiltse2,13 (isthmic spondylolisthesis). Subtype A occurs as a result of fatigue failure of the pars and is evident by a complete defect or separation of the bone. Subtype B or an elongated pars occurs as a result of repeated microtrauma with subsequent healing of the bone as the slippage gradually occurs. Subtype C is an acute pars fracture.
Anatomy and Biomechanics
The cross-sectional anatomy of the pars at each level in the lumbar spine contributes to the increased incidence as to which level the breaks occur.14 The pars is fairly large in diameter in the upper lumbar vertebra and relatively thin at the L5 level. A congenitally dysplastic pars combined with upright posture increases the forces concentrated across the pars with extension and can lead to stress fractures. Sports activities that place loaded extension across the lumbosacral junction increase the forces across the pars and increase the chance of a stress fracture occurring in the pars with the smallest cross-sectional area. Facet joints oriented more coronally cephalad to the lumbosacral junction have been shown to be present in patients with isthmic spondylolisthesis.15 Attempts to heal the pars defect lead to increased cartilage and fibrous tissue further compromising the lateral recess and compressing the exiting nerve root. Slips occurring as a result of acute trauma cause destruction of the bony arch or facet, as well as the soft tissue components of the disc, annulus, and ligaments.
Diagnosis
History
Most people with isthmic spondylolisthesis are asymptomatic.16 Those who do become symptomatic usually present with back pain, leg pain, or a combination. Complaints of back pain with activity and relieved with recumbency are often described. The leg pain numbness or paresthesia described by symptomatic patients is predominately dermatomal in distribution if the nerve is being compressed in the lateral recess at the level of the pars defect. It is described as scleradermal if referred into the broad region of the buttock or posterior thigh, which occurs usually as a result of the disc degeneration that often accompanies the pars defect.
Imaging
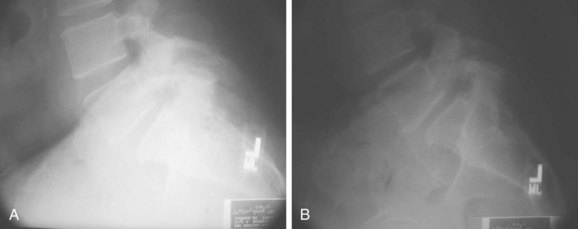
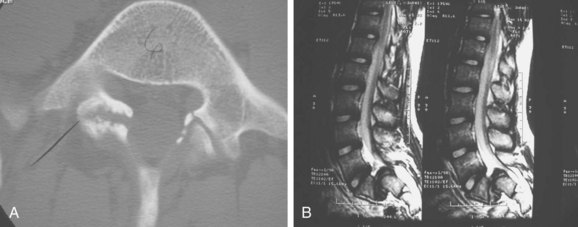
Radiographic evaluation should consist of anteroposterior and lateral flexion-extension radiographs. Having both a supine and standing lateral radiograph is important.9 This combination will allow the determination of translational instability (Fig. 72–3). If necessary, oblique radiographs can be obtained. This will better delineate the integrity of the pars intra-articularis. Computed tomography (CT) scans will provide excellent bony details of the pathology, and the magnetic resonance scan will give much better delineation of the soft tissue abnormalities associated with the problem (Fig. 72–4).
SPECT scans can be used for delineation of the problem if suspected clinically and radiographs are inconclusive. This study can also be helpful in determining whether or not the defect is acute or chronic. Spina bifida occulta has been reported to be as high as 70% in patients with an isthmic defect.17 Scoliosis is noted in 5% to 7% of patients with spondylolisthesis and usually presents as a long C-shaped curve rather than those of a rotated variety.18
Treatment Options
Conservative Treatment
Initial treatment in the acute phase should consist of nonsteroidal anti-inflammatory drugs (NSAIDs), pain management, and physiotherapy. Exercises should be directed to strengthen the abdominal and paraspinal musculature, as well as a stretching program to improve flexibility. Weight loss and aerobic conditioning programs should be added if necessary. Bracing can be used as an adjunct to the physiotherapy.19 The use of steroid injections into the facet joint and epidural space are helpful in the acute phase but are not advocated for long-term use due to potential complications of this medication with long-term use. The use of narcotic medications other than in the acute phase should be avoided because they adversely affect recovery and can lead to prolonged disability. The majority of patients will completely recover within 3 months of onset and can be allowed to return to full activity. Incorporation of a daily exercise routine for maintenance of muscular strength and flexibility should be encouraged. If this fails, surgical options should be considered.
Surgical Goals
The goals of surgical treatment in spondylolisthesis consist of stabilization of the affected levels along with decompression of the neural elements. Stabilization prevents further slippage of the vertebra. Decompression of the neural elements prevents further progression of the neural deficit and allows the present deficit the best chance to recover. Wiltse and colleagues20 reported that stabilization of segmental movement through the defect by fusion can result in improvement and resolution of the neural deficit by preventing the continued motion segment from irritating the neural tissues.
In the high-grade slips, the cosmetic problem that results from the posture and gait abnormalities can be an indication for the surgery. The significant risk of neurologic problems in this group of patients, should reduction be planned, must be carefully considered and presented when discussing this procedure with the patient.21–26
Contraindications for Surgical Repair
Relative contraindications for surgery because of expected poor outcome include patients who continue to smoke and have either disability or compensation claims.27,28 Those with previous multiple procedures for fusion or pseudarthrosis repair also have reported poor outcomes following surgery.
Surgical Options
Treatment options in isthmic spondylolisthesis consist of (1) a direct repair of the pars intra-articularis30–33; (2) decompression of the neural elements alone34–37; (3) decompression of the neural elements in conjunction with an in situ posterior lateral fusion32,38,39,40; (4) decompression of posterior lateral fusion with associated pedicular instrumentation28,39,41; and (5) decompression and reduction of the spondylolisthesis with instrumentation and interbody fusion.42–44
The progression of the slippage is a fairly complex biomechanical problem, which results from shear forces being placed across the segment as a result of the kyphotic deformity from the spondylolisthesis.45–47 The body weight acts as a vertical load creating a shearing moment, which is enhanced as result of the local kyphosis and results in anterior translation in the sagittal alignment, as the vertebra rolls over the sacral dome. The paraspinal muscles increase their tone in response to minimize the shear going across this segment, which can result in spasm with hyperlordosis often seen clinically (Fig. 72–5). Pelvic incidence seems to play a factor in the progression of the spondylolisthesis.48 Hansen and colleagues recently showed in their study a statistically significant increase in the chance of slippage as the pelvic incident angle increases.49 (Fig. 72–6) When compared with his control group without any spondylolisthesis, which had a 57-degree pelvic incidence angle, those patients with a low-grade spondylolisthesis had a pelvic incidence of 68.5 degrees, whereas those with high-grade slippage had a pelvic incidence angle of 79 degrees. This, in conjunction with the gravity across the locally kyphotic segment, tends to increase the shear forces across the affected segment and result in increased slippage.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree