20
Acute Nerve Laceration
Kevin D. Plancher
History and Clinical Presentation
A 20-year-old right hand dominant male laborer caught his left hand in a circular saw with the “guard” off. He has a laceration to his left index finger and can’t feel the tip of his finger, and has an open bleeding wound.
Physical Examination
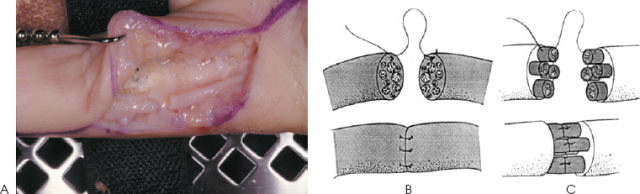
On physical examination, the patient has an acute open laceration involving the radial side of the right index finger. A careful motor examination was performed. The functioning level of specific muscles is determined to assist with identifying peripheral nerve injuries. A two-point sensory discrimination test (Fig. 20–1), as determined by the Weber two-point discrimination test, using a dull pointed eye caliper applied in the longitudinal axis of the digit without blanching the skin, and a two-point discrimination (2-PD) (both moving and static), Semmes-Weinstein monofilaments, and vibrometer tests were used to assess the status of the nerves. Denervated skin responds differently to stimuli; when the injured hand is placed in water, innervated skin wrinkles and denervated skin does not. This test can be helpful in determining the affected peripheral nerves in the hand in unconscious patients.
Diagnostic Studies
Radiographs were performed to rule out associated fractures.
PEARLS
- Microscopic repair is always more accurate.
- Occupational therapy post-operatively will successfully complete a desensitization program.
- The area of injury must be defined for successful functional nerve repair.
PITFALLS
- Clean ends of nerve must be sewn together to avoid a neuroma in continuity.
- Missed diagnosis with a devascularized finger may lead to amputation
- Range of motion must be controlled with splinting.
Differential Diagnosis
Vascular injury
Muscle laceration
Neurologic disorder
Nerve laceration
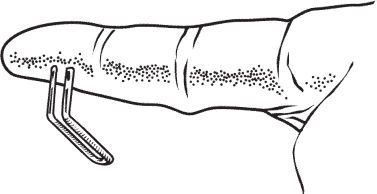
Figure 20–1. Weber static two-point sensory discrimination test.
Diagnosis
Acute Laceration, Radial Nerve, of the Index Finger
Neurapraxia is the mildest form of nerve injury. This usually involves demyelination without axon disruption and degeneration. This type of injury has a relatively short recovery time, and full function is expected without intervention.
Axonotmesis occurs when axons, myelin, and associated internal nerve structures are disrupted. These injuries often result from situations in which traction overcomes the inelastic internal structures but leaves the elastic epineurium intact. When axons are disrupted and the endoneurium and the rest of the nerve are intact, degeneration and regeneration occur. This is the first stage of injury that shows an advancing Tinel’s sign. Because the endoneurium is intact, regeneration should be full with complete sensory and motor function regained.
Another type of injury occurs when the axons and the endoneurium are damaged and the perineurium and epineurium are intact. This leaves the blood–nerve barrier intact but provides a disorganized bed through which the axons can travel. Nerve regeneration may be slowed due to infiltration of scar tissue or a smaller number of axons capable of survival and regeneration. An advancing Tinel’s sign, though some-what slowed, should be present.
The worst form of closed nerve damage is when all structures are damaged except the epineurial covering. This disables the intact axons and no conduction down the nerve is possible. Surgical intervention is required to restore function. A Tinel sign is present at the level of injury and does not move distally because the regenerating nerve is kept from advancing by large amounts of scar tissue or debris.
Neurotmesis is the most severe type of injury. This class of injury is easy to diagnose because it usually involves an open wound with nerve deficits. Surgical repair is a requirement for any return in function to occur. Results following the surgical repair of digital nerves are inconsistent. Among the factors that could impact on outcomes are the amount of direct trauma to the nerve, the length of nerve that has been traumatized, and the age of the patient. Increased tension on the repair has also been shown to effect the final results.
Nerve repair never results in the return of full sensibility. However, reasonable protective sensibility to light touch and pin pricks can be obtained. Two-point discrimination can approach normal in as many as one patient in three (33%).
Surgical Management
After usual draping and prepping of the patient, the skin is marked. The patient is supine and a regional anesthetic is administered. If multiple structures need to be repaired, then general anesthesia is used and the arm is exsanguinated using a tourniquet on the forearm or arm.
Incision use for this procedure is a midaxial incision because it offers the best extensile exposure to the palm and finger. Some surgeons use a Bruner zigzag to expose the nerve, but we feel excessive scarring results with this type of incision. Gross exploration is accomplished under loupe magnification using tenotomy or other scissors.
After initial exploration, using a microscope for high-power magnification, identify the nerve and trim any necrotic or bruised tissue until normal fascicles are found (Fig. 20–2A). Then transect the nerves perpendicular to the main axis and carefully examine them to ensure that they are healthy and uninjured fascicles are found (Figs. 20–2B,C). Several sequential transections may be indicated before finding appropriate endings for repair.