Acromioclavicular Joint Disorders
Richard B. Jones
Mark S. Schickendantz
INTRODUCTION
Acromioclavicular (AC) joint injury is among the most common problems occurring in sports today and throughout history. This joint is not only susceptible to traumatic injury, but degenerative processes as well from prior trauma or overuse. Injuries to the AC joint are commonly confused with other problems of the shoulder complex. Hippocrates (460-377 BC) found that AC joint dislocations were often misdiagnosed as a glenohumeral injury (1). This trend continues to hold true. AC joint dislocation is more common in males (5 to 10:1) and is more often incomplete than complete (2:1) (2).
A broad spectrum of injury can occur at the AC joint and much controversy still exists in the treatment of this injury. Whether or not to treat these injuries operatively or nonoperatively has been widely debated. Furthermore, numerous techniques have been described for the operative treatment of this injury. Treatment of AC disorders in the subgroup of overhead athletes is the most debated. Disorders of the AC joint are relatively uncommon in overhead athletes. The throwing motion seems to cause little stress to the AC joint. If problems do arise, they most frequently consist of degeneration or acute or chronic instability.
ANATOMY
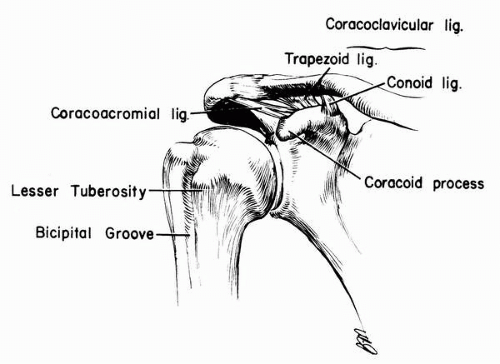
The AC joint is a diarthrodial joint composed of the lateral end of the clavicle and the medial margin of the acromion. Along with the sternoclavicular joint, it is the only articulation of the upper extremity with the axial skeleton. The articular surface initially consists of hyaline cartilage, which at age 17 years on the acromial side and 24 years on the clavicular side becomes fibrocartilage (3). The fibrocartilaginous intraarticular disk of the AC joint commonly undergoes degeneration throughout life; therefore, it is uncommon to find patients older than age 35 to 40 years without at least radiographic evidence of arthrosis of this joint (4,5). The AC ligaments reinforce the thin capsule. They consist of superior, inferior, anterior, and posterior capsular thickenings. The superior ligament is the strongest of the AC ligaments and blends with fibers of the deltoid and trapezius muscles, which are dynamic stabilizers of the AC joint (6). The coracoclavicular ligaments spanning from the inferior clavicle to the base of the coracoid process are the strongest static stabilizers of the AC joint. They consist of two parts, which may be separated by a bursa (Fig. 16-1). The conoid is 0.7 to 2.5 cm in length and 0.4 to 0.95 cm in width and cone shaped. Its apex attaches to the posteromedial side of the base of the coracoid process. The base of the conoid ligament attaches to the posterior inferior clavicular curve at the conoid tubercle. The trapezoid is 0.8 to 2.5 cm in length and 0.8 to 2.5 cm in width. It attaches anterolaterally to the conoid ligament on the coracoid process, extending superiorly to the undersurface of the clavicle (7,8).
BIOMECHANICS
The primary function of the AC joint is to transmit energy to the axial skeleton from the appendicular skeleton and support the upper extremity. The rotatory motion at the AC joint has been debated. Ranges have been reported from 5 to 20 degrees of motion (9,10). Rockwood placed pins into the acromion and clavicle of volunteers and found only 5 to 8 degrees of rotation with shoulder range of motion (2). This has important implications in considering surgical fixation options for AC injuries. Rigid coracoclavicular screw fixation must be removed after healing or screw failure will eventually occur because of this normal motion. Furthermore, cerclage techniques around the distal clavicle may eventually erode the clavicle from small amount of rotatory motion.
The AC ligaments are thought to primarily control horizontal (anterior and posterior) stability. Fukuda and colleagues demonstrated that the AC ligaments are the principal restraints to axial distraction and posterior translation (11). However, Lee and co-workers found the in situ force of the trapezoid (42.9 ± 15.4 N) was significantly greater during posterior displacement than other ligaments (6).
The coracoclavicular ligaments control vertical stability of the AC joint. They help couple glenohumeral abduction and flexion to scapular rotation on the chest wall. Both the conoid and trapezoid ligaments must be disrupted to cause a complete vertical AC joint dislocation. Debski and colleagues (12) showed that, after transection of the capsule, the conoid ligament served as the primary restraint to anterosuperior loading and the trapezoid ligament was the primary restraint to posterior loading. As a result of these findings, they recommended that surgical reconstruction address both ligaments in order to restore stability in both the horizontal and vertical planes. They also concluded that injuries to the AC capsule may render the intact coracoclavicular ligaments more likely to fail with subsequent anteroposterior loading. In another similar study, Debski and colleagues (13) showed differences in the load sharing properties of the conoid and trapezoid ligaments and again stressed the possible need to reconstruct both ligaments.
MECHANISM OF INJURY
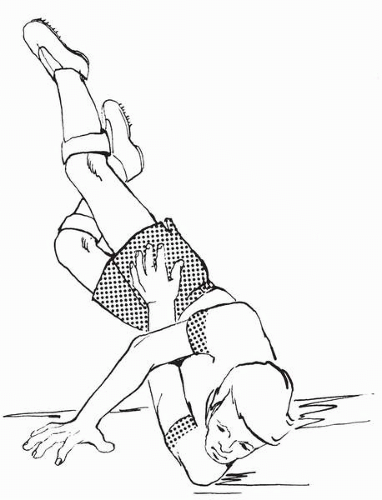
Injury of the AC joint most commonly occurs from the application of direct force. Direct force injury occurs when the athlete falls on the shoulder with arm adducted (Fig. 16-2). It can also occur with direct hits, such as those sustained in football, hockey, and karate. Most agree that the force first disrupts the AC ligaments. If the force is sufficient, this energy is transmitted to and disrupts the coracoclavicular ligaments, resulting in increased displacement of the clavicle relative to the acromion. The acromion is forced in a downward, medial, and anterior direction. During a fall, this is usually due to a combined direct impact and body roll toward the injured shoulder. Basamania (14) related that, as the body strikes the ground, the head and shoulder hit first causing rupture of the AC ligaments. With sufficient energy, the trapezoid ligament ruptures. As the force continues, the scapula and acromion are driven medially, causing the conoid to reside in a vertical position. As the force continues, the
conoid is ruptured, allowing further medial translation of the acromion relative to the clavicle.
conoid is ruptured, allowing further medial translation of the acromion relative to the clavicle.
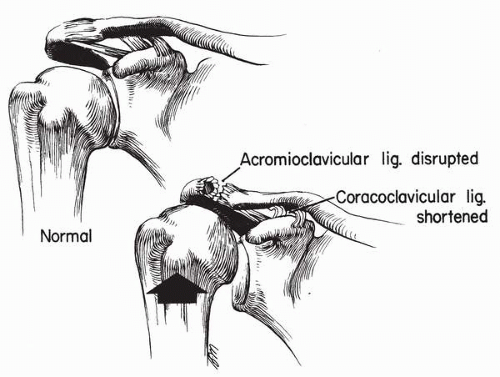
Indirect force injury is less common. It usually occurs when the athlete lands on an outstretched hand. The force is transmitted up the arm, through the humerus, into the humeral head, and into the acromion process. However, the energy is only directed to the AC ligaments. The coracoclavicular ligaments are not disrupted because there is a decrease in the coracoclavicular space (Fig. 16-3).
CLASSIFICATION
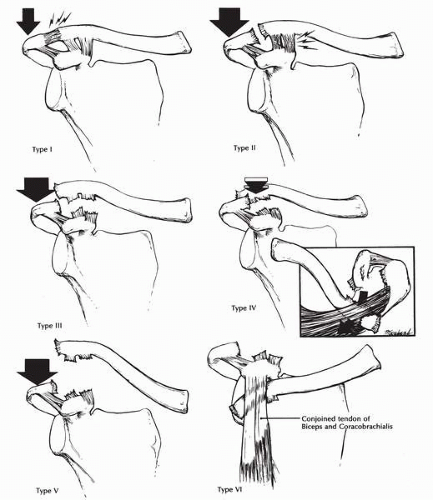
Like all classification systems, the classification of injuries to the AC joint should correlate to prognosis and assist with treatment. The two most popular classification systems for AC injuries are described by Allman (15) and Tossy and colleagues (16), and by Rockwood and colleagues (2). Allman (15) and Tossy (16) separated AC injuries into three distinct categories. Type I injuries involve a strain of the AC ligaments with intact coracoclavicular ligaments. Type II injuries involve ruptured AC ligaments with strained but intact coracoclavicular ligaments. Type III injuries were the worst in severity and involved ruptured AC and coracoclavicular ligaments. Rockwood, however, believed that there were varying degrees of type III injuries with different outcomes attributed to their severity. Based on his clinical findings, he proposed an expanded classification with further subdivision of Allman and Tossy’s type III category (Fig. 16-4). In Rockwood’s classification system, type I injuries are essentially the same as Allman and Tossy’s. Type II injuries involve disruption of the AC ligaments and strain of the coracoclavicular ligaments with up to 25% displacement of the coracoclavicular distance. A type III injury includes disruption of the AC ligaments and the coracoclavicular ligaments with a 25% to 100% displacement of the coracoclavicular interspace. The deltotrapezial fascia is usually disrupted as well. Type IV injuries are similar to type III except that the clavicle is displaced posteriorly into the trapezius. This occurs with a more anteroposterior force than the typical superoinferior force. Type V injuries are a more severe form of type III, with greater than 100% displacement at the coracoclavicular interspace. Type VI injuries are rare and associated with severe trauma. These involve inferior displacement of the clavicle beneath the coracoid. This is thought to be due to a severe hyperadduction and external rotation of the extremity (17).
PRESENTATION AND PHYSICAL EXAMINATION
The athlete should be examined in the standing or sitting position to allow downward force from the weight of the arm to intensify the deformity of the AC joint. Often a severe deformity reduces with the patient in the supine position. It is not uncommon for injuries that appear less severe initially to look worse upon later examination. Acute soft tissue swelling often hides the actual degree of deformity. As this subsides, the deformity becomes more obvious. Additionally, patients tend to initially splint their injury because of pain, and once pain subsides the weight of the arm accentuates the deformity. Grasping and gently manipulating the mid shaft of the clavicle can be done to assess the stability of the AC joint. Gross motion, particularly in the vertical plane, often indicates the presence of a high-grade injury. With an injury to the AC joint, athletes experience pain at the joint with full forward flexion of the shoulder as well as with cross-body adduction. Another examination technique involves having the athlete place the hand of the affected arm on the contralateral shoulder while the examiner applies gentle downward pressure on the affected elbow. If the athlete experiences pain at the AC joint, injury should be suspected.
With type I injuries there is usually no gross deformity. There may be mild swelling over the AC joint. There is tenderness to palpation over the AC joint but usually not in the region of the coracoclavicular ligaments. Range of motion is usually full. Overhead athletes may have pain at the extremes of motion such as the late cocking phase or follow-through phase of throwing.
Patients with type II injuries have moderate to severe tenderness at the AC joint. They usually have some mild deformity in the region as a result of swelling or slight displacement of the AC joint. These patients may have some slight motion with manipulation of the clavicle and may have palpable popping or grinding in the joint. Range of motion is usually limited by pain.
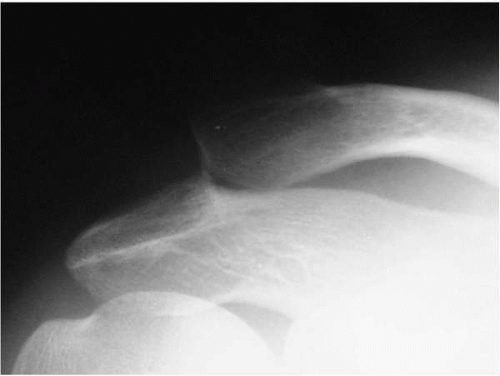
Type III injuries usually display obvious deformity (Fig. 16-5). Patients have severe pain, limited range of motion, and tenderness over the AC joint as well as the coracoclavicular region. Instability is present at the AC joint with manual manipulation. Patients usually hold the arm at their side in attempts to splint the injury, and, as mentioned earlier, this may decrease the deformity. Adducting the arm across the body usually causes severe prominence of the clavicle as a result of medial displacement of the acromion (Fig. 16-6).
Type IV injuries display posterior displacement of the clavicle into the trapezius. This may be due to the anteromedial rotation of the scapula relative to the clavicle and often reduces when the patient is in the supine position. However, the clavicle can button-hole through the trapezius fascia and be difficult to reduce. However, this is a rare injury. Patients with type V injuries have a similar presentation as type III, but usually have a more severe deformity at the AC joint. Type VI injuries are rare and are usually associated with severe trauma. Gross deformity is present often with other associated injuries. Severe neurovascular compromise may be present as well.
Patients with chronic injuries have varying degrees of deformity depending on the severity of the initial injury. They may have continued instability of the AC joint. Chronic pain at the AC joint and weakness with lack of endurance at the shoulder joint may be seen as well.
RADIOGRAPHIC AND DIAGNOSTIC EVALUATION
Radiographs are used to evaluate the extent of injury as well as exclude fractures of the acromion, clavicle, and coracoid. However, standard radiographic technique for shoulder radiographs overpenetrate and wash out the AC joint. Radiographs evaluating the AC joint should be obtained at about 50% of the intensity of those obtained for the glenohumeral joint. This helps avoid missed injuries to the area resulting from poor radiographs. It is also important to obtain a standard shoulder radiographic series in any patient with a traumatic shoulder injury to thoroughly assess the joint.
The patient should be standing or in the seated position to accentuate any deformity at the AC joint. If possible, both AC joints should be imaged on the same cassette to ensure the same technique is used in comparison. Zanca (18) showed that the optimal technique to visualize the AC joint is to angle the x-ray beam 15 degrees in the cephalad direction on an anteroposterior radiograph. This eliminates superimposition of the spine of the scapula on the AC joint.
Patients may splint the injury by supporting the injured extremity with the opposite arm or by muscular contraction, thus decreasing deformity on radiographs. Stress radiographs can be used in this situation. These are performed by suspending approximately 10 to 15 pounds from the patient’s wrists while obtaining standard anteroposterior radiographs of both shoulders. Bossart and colleagues (19) believed that weighted radiographs are ineffective and offered low yield in obvious AC joint injuries, and thus should not be routinely ordered. Similarly, we have not found weighted radiographs of the AC joint to be helpful and do not recommend their routine use.
Other stress views have been described. Alexander (20) described a view in which the shoulders are pushed forward to displace the acromion inferiorly and anteriorly. A scapular lateral view is obtained in this position and compared to the opposite side. Basamania (14) described a cross-body adduction view in which the patient adducts the arm across the body and grasps it with the unaffected arm. A standard anteroposterior radiograph is then obtained. With significant injury to the AC joint, the acromion is seen displaced inferior and medial to the clavicle.
 FIGURE 16-6. Accentuation of the deformity seen with a grade III acromioclavicular injury that occurs with adduction of the involved limb. |
Consistent radiographic findings are present on standardized radiographs of the AC joint depending on the severity of injury. Comparison with the uninvolved side is important in all cases. With type I injuries, there is usually no joint widening or deformity. There may be mild soft tissue swelling over the AC joint. Type II injuries display a slight increase in the coracoclavicular interval, usually less than 25% greater than the opposite side (Fig. 16-7). The
AC joint may appear widened as a result of the slight posterior displacement by the trapezius muscle. With type III injuries, the acromion is displaced inferior to the clavicle 25% to 100% the width of the clavicle. The coracoclavicular interval is also increased 25% to 100% relative to the opposite shoulder. If the coracoclavicular distance is not increased, a fracture of the base of the coracoid should be suspected. A Stryker notch view is indicated in this case to rule out coracoid fracture.
AC joint may appear widened as a result of the slight posterior displacement by the trapezius muscle. With type III injuries, the acromion is displaced inferior to the clavicle 25% to 100% the width of the clavicle. The coracoclavicular interval is also increased 25% to 100% relative to the opposite shoulder. If the coracoclavicular distance is not increased, a fracture of the base of the coracoid should be suspected. A Stryker notch view is indicated in this case to rule out coracoid fracture.
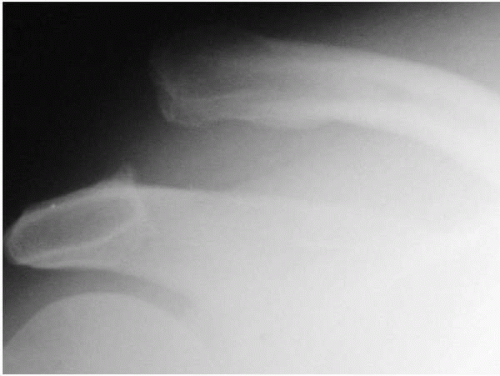
Type IV injuries show posterior displacement of the clavicle relative to the acromion. This is best seen on an axillary view or CT scan. There are varying degrees of displacement at the AC joint and increases in the coracoclavicular interval. Type V injuries have increases in the coracoclavicular interval of greater than 100% (Fig. 16-8). There is severe displacement at the AC joint as well, reaching two to three times the width of the clavicle. Type VI injuries are rare and severe injuries that may have associated fractures or dislocations. The clavicle is displaced inferior to the coracoid process.
TREATMENT
Treatment of AC joint injuries, particularly type III, remains controversial. There have been more than 35 nonoperative treatment modalities described in the orthopedic literature and far more operative procedures described for this particular injury (2). It is well accepted that patients with AC joint injuries of type I or II should initially be treated nonoperatively. However, not all patients who experience type I or II injuries recover fully. Bergfeld and colleagues (21) looked at the long-term clinical results of type I and II AC joint injuries in Naval cadets. Symptoms were present in 39% of cadets who sustained type I injuries and in 65% of those with type II injuries.
It is also well accepted that type IV, V, and VI injuries should generally be treated operatively. However, when treating an athlete with a type III AC injury, the decision to treat the injury operatively or nonoperatively is often difficult. Historically, proponents of early operative treatment of type III injuries have cited persistent deformity, AC arthritis, and residual weakness as reasons for surgery (22, 23, 24). However, current literature suggests that most patients with type III AC injuries have comparable strength and range of motion of the shoulder with either operative or nonoperative treatment (25,26). Wojtys and Nelson (27) supported this claim, but did find increased discomfort with high activity levels in patients treated nonoperatively. Schlegel and co-workers (25) prospectively evaluated a small group of patients with type III injuries treated nonoperatively. Twenty percent believed their outcome was suboptimal. However, none experienced symptoms severe enough to warrant surgery. Objectively, no patient had significant deficits in strength or range of motion. Rockwood (2) recommends operative treatment of type III injuries in laborers and overhead, high-performance athletes. He does point out that contact athletes may be better treated nonoperatively because of the high risk of failure of surgery in this patient population.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree