Protrusion in young adults without OA
Deformities
Treatment
(i) Global overcoverage
Rim trim ± labral refixation/reconstruction
(ii) High trochanter
Neck lengthening + trochanteric advancement
(iii) High fossa with negative roof angle
PAO
(iv) Medial shift of femoral heada
Intertrochanteric valgization osteotomy
Surgical Technique
The technique of surgical hip dislocation (SHD) is the workhorse to address acetabular overcoverage in protrusion and is covered in detail in the literature [15] and in Chap. 51, “Surgical Technique: Open Acetabular Rim Trimming, Labral Refixation, and Open Femoral Osteochondroplasty.” Based upon coexisting deformities, relative neck lengthening with trochanteric advancement [16, 17], periacetabular osteotomy (PAO) [18], and intertrochanteric valgus osteotomy are potential concomitant procedures that may become necessary. Since all of these procedures have been described in the literature, only critical aspects relevant to the treatment of protrusion will be covered.
Surgical Hip Dislocation
To address acetabular overcoverage (pincer impingement ), surgery usually starts with an SHD. The first important aspect to appreciate during SHD is that protrusion hips can reveal a relatively high-riding greater trochanter; oftentimes relative lengthening of the femoral neck and distal advancement of the greater trochanter is required to increase the clearance on the femoral side. In such instances, a classic trochanteric slide osteotomy as originally described [15] should be preferred over the more recently introduced step-cut osteotomy. The latter one provides better mechanical conditions after refixation [19, 20] but does not allow to distally advance the trochanter. Another consideration in hips revealing a high-riding trochanter is that the gluteus minimus muscle extends distally under the piriformis muscle, which might make the dissection off the capsule more difficult. The remaining dissection of the capsule and capsulotomy is not different from standard surgical dislocations.
Head Dislocation and Rim Trimming
The second critical step is the dislocation of the femoral head itself, which, similar to THR, is more difficult in protrusion and has to be performed carefully so as not to forcefully deliver the femoral head. When performed after relative neck lengthening, external rotation is increased and facilitates anterior dislocation. In the authors’ experience, rim resection prior to dislocation had never to be performed, but might be considered. Technically, however, rim resection with the dislocated head will allow for a more precise assessment and conduction of the rim resection. The third important consideration is the size of horseshoe or acetabular articular surface. The fact that there is global overcoverage does not mean that excess articular cartilage is present. In fact, often the opposite is true. The acetabular fossa in patients with protrusion is typically enlarged and runs very high (negative roof tilt), and the horseshoe may even be narrowed (Table 1). In such patients, especially with a negative roof tilt, conservative trimming of the acetabular rim is indicated, and a PAO needs to be considered to reorient and conserve the horseshoe. The head neck junction in protrusion frequently shows an indentation line (rather than a cam deformity) at the head neck junction which typically is more peripheral than the classic cam deformity. Additional femoral neck osteoplasty does not significantly improve the situation, but might be considered. Adaptive head neck changes on the posterior neck also have to be considered and if present should be addressed. These are sometimes ossifications at the head neck junction that can be found as a result of chronic neck abutment.
Labral Refixation/Reconstruction
Although sufficient coverage after rim trimming might not demand labral preservation, it is the authors’ recommendation to preserve the native labrum, if it is of sufficient quality [21]. However, chronic periosteal irritation followed by bone apposition and overgrowth of the labrum might have stretched the labrum with a resultant thinning impairing the sealing function especially when the acetabular rim had been surgically removed and the remnants of the labrum are fixed to the acetabular bone [22]. In these cases, circumferential labral reconstruction [23] might become necessary as described in another chapter (Chap. 97, “Surgical Technique: Open Hip HS Allograft”). Usually, multiple bone anchors between 10 and 15 mm apart are required for circumferential refixation (Fig. 1).
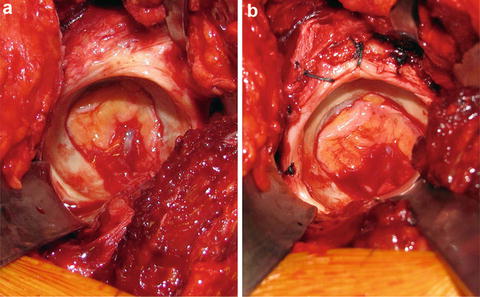
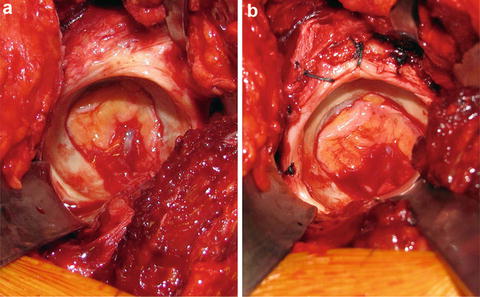
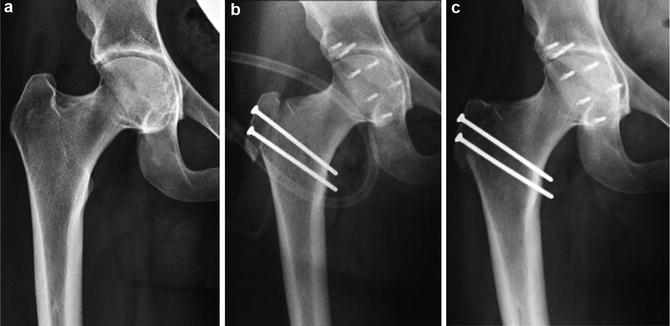
Fig. 1
(a) The acetabular fossa in patients with protrusion is typically enlarged and runs very high, and the horseshoe may even be narrowed. (b) In such patients, especially with a negative Tönnis angle, conservative trimming of the acetabular rim is indicated
Relative Neck Lengthening and Trochanteric Advancement
If not already performed to facilitate the dislocation, trimming of the stable trochanter for relative lengthening may be executed after addressing intraarticular impingement. The gain in range of motion might minimize the potential for pelvi-trochanteric impingement, specifically, in hips with a high trochanter. In these hips, relative neck lengthening with trochanteric advancement can improve muscular biomechanics and resolve the extra-articular impingement. The described technique is called “relative neck lengthening,” because only the superior circumference of the neck becomes longer by the trimming away of most of the trochanteric portion in its posterosuperior circumference, such that it becomes continuous with the smaller contour of the neck [16, 17]. Leg length remains the same, but muscle biomechanics and clearance for hip motion is improved [24]. At the end of the procedure, the distal advancement of the trochanteric fragment is facilitated by a release of the long head of the gluteus minimus muscle, which runs along the anterior border of the mobile trochanteric fragment. The definitive cephalad-caudad position of the trochanteric fragment, and therefore the amount of the trochanteric advancement, is aimed to distalize the tip of the trochanter to the level of the center of rotation of the femoral head avoiding overdistalization (Fig. 2).