25 ABDOMINAL INJURIES
Trauma is the fourth leading cause of death for all age groups in the United States.1 It is the leading cause of death for individuals between the ages of 1 and 44 years.1 Abdominal injuries rank third among the causes of traumatic death, preceded only by head and chest injuries.2 Death and disability from traumatic injury have become a significant health and social problem. Intra-abdominal trauma is seldom a single organ injury or single system injury; therefore, a concomitant rise in morbidity and mortality rates is evident.
Abdominal trauma challenges even the most experienced nurse. The manifestations of abdominal injury are often subtle, requiring continual assessment and care modification as the patient progresses from the initial assessment to the critical care phase. Frequent assessments and continual monitoring are essential components of the nursing process for detection of changes in the patient’s condition. Unrecognized abdominal trauma is a frequent cause of preventable death.3 An organized, methodical approach to assessment, diagnosis, and intervention is necessary for the management of suspected abdominal injury. Knowledge of the mechanism of injury, patient complaints, serial physical assessments, and timely diagnostic test results are the nurse’s resources for identifying potentially life-threatening abdominal injuries.
THE ABDOMEN: ANATOMY AND PHYSIOLOGY
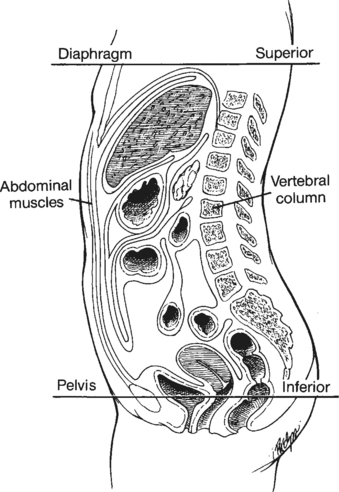
The abdomen is formally thought of as containing structures bordered superiorly by the diaphragm, inferiorly by the pelvis, posteriorly by the vertebral column, and anteriorly by the abdominal and iliac muscles (Figure 25-1). For this discussion of abdominal trauma, the esophagus, which passes through the diaphragm and connects with the stomach, has been added to this chapter.
For purposes of examination, the abdomen is divided into four quadrants: right upper quadrant (RUQ), left upper quadrant (LUQ), right lower quadrant (RLQ), and left lower quadrant (LLQ). The major organs found in each quadrant are highlighted in Figure 25-2.
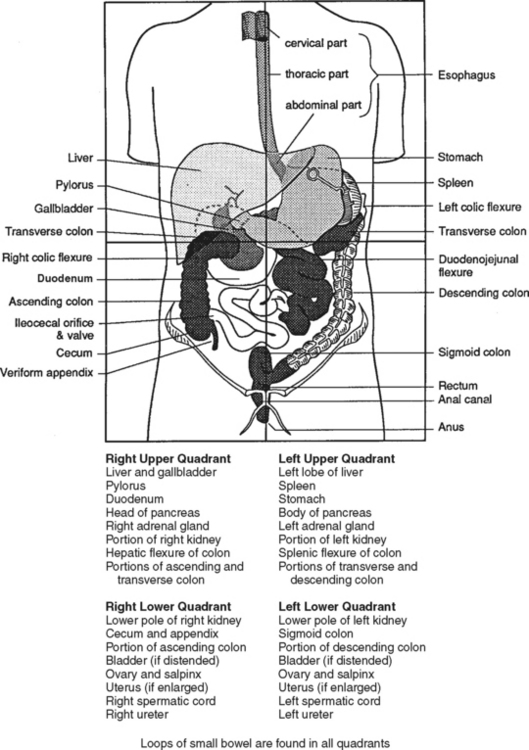
FIGURE 25-2 Contents of the four abdominal quadrants.
(Modified from GI series—physical examination of the abdomen, Richmond, Va, 1975, AH Robins, p 6.)
ESOPHAGUS
The esophagus, the first segment of the digestive process, carries food from the pharynx to the stomach. The presence of food within the esophagus stimulates peristaltic action and causes food to move into the stomach. Mucosal glands of the esophagus secrete mucus to lubricate and facilitate passage of the food bolus.4
DIAPHRAGM
The diaphragm assists with inspiration and expiration by changing the thoracic volume during respiration. Flattening and contraction of the diaphragm lengthen the thoracic cavity, increasing thoracic volume during inspiration.5 During expiration the diaphragm relaxes, returning to its original dome shape and reducing thoracic volume.5 This process is aided by the accessory intercostal muscles. The diaphragm also separates the thoracic and abdominal cavities, preventing herniation of organs.
STOMACH
The stomach has multiple digestive functions, including (1) serving as a reservoir to store food, (2) secreting gastric juice containing acids and enzymes to aid in the digestion of food, (3) secreting intrinsic factor, (4) carrying on a limited amount of absorption of certain drugs, alcohol, some water, and some short-chain fatty acids, and (5) producing the hormone gastrin, which helps regulate digestive functions.5
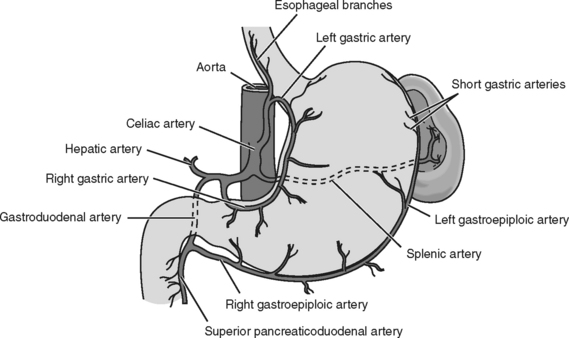
The stomach joins the esophagus approximately 3 cm below the diaphragm. It is located in the LUQ and is suspended superiorly by the gastrohepatic ligament, inferiorly by the gastrocolic ligament, and laterally by the gastrosplenic ligament. The stomach resides within the peritoneal cavity. It is divided into the fundus, body, and pylorus (Figure 25-3). The stomach wall contains glands that secrete mucus, hydrochloric acid (HCl), intrinsic factor, and pepsinogen (type I); serotonin is secreted in the fundus and body; and mucus and pepsinogen II are secreted in the pylorus. Perforating gastric injury causes the release of these digestive contents into the peritoneal cavity. These same gastric secretions cause stress ulcerations in the stomach.
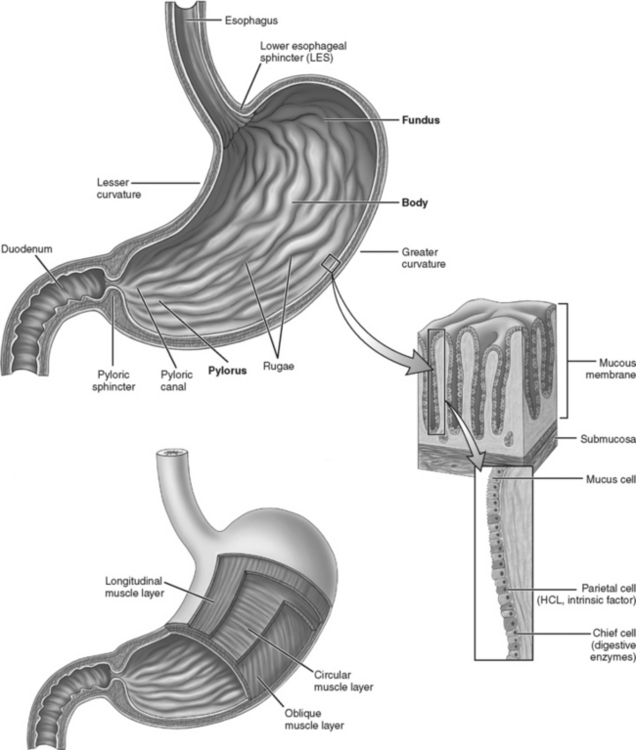
FIGURE 25-3 Stomach: regions of the stomach: fundus, body, and pylorus. HCL, Hydrochloric acid.
(From Herlihy B, Maebius NK: The human body in health and illness, Philadelphia, 2000, W. B. Saunders, p 394.)
The stomach has a rich blood supply. The arterial supply is provided by the splenic artery, gastric arteries, gastroepiploic arteries, and short gastric arteries (Figure 25-4). Venous drainage occurs through the hepatic portal system, which branches out to include the gastric and the gastroepiploic veins, which drain into the splenic vein. Gastric emptying is facilitated by peristaltic movement from the pylorus and is stimulated by stretch receptors. An inhibiting function is controlled in the duodenum.
LIVER
The liver, the largest gland in the body, performs many vital, life-sustaining functions, including those listed below4:
• Detoxification of various substances, such as drugs and alcohol
• Synthesis of plasma proteins, important in maintaining blood volume and controlling blood coagulation
• Storage of iron and vitamins A, D, E, K, and B12 in liver cells
• Metabolism of carbohydrates, which has a role in regulating blood glucose levels
• Metabolism of protein, which can synthesize amino acids and converts nitrogen to urea for excretion by the kidneys
• Metabolism of fats, which breaks down fatty acids, synthesizes cholesterol and phospholipids, and converts excess dietary protein and carbohydrates to fat
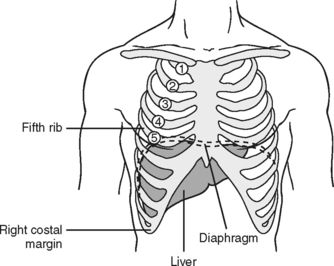
The liver is the largest intra-abdominal organ, weighing approximately 3 to 4 pounds. It is an extremely vascular organ and lies in the RUQ, extending transversely across the midline. The right margin lies at the sixth to tenth ribs and the left margin at the seventh and eighth ribs (Figure 25-5). The liver is divided into two lobes, right and left, which are separated by fissures on the inferior surface. Between these two lobes is the porta hepatis, where veins, arteries, nerves, lymphatic vessels, and bile ducts enter or leave the liver.
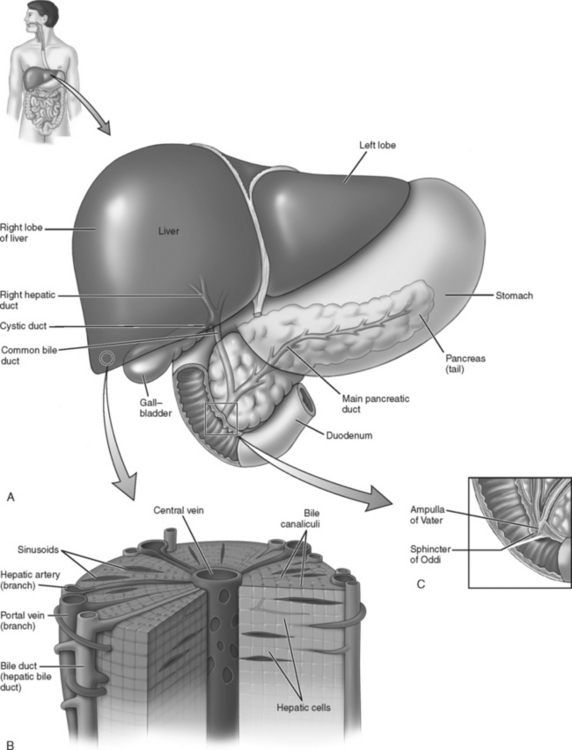
Approximately three fourths of the blood to the liver is delivered by the portal vein, which carries a rich supply of nutrients after draining the gastrointestinal tract. The rest of the arterial blood supply is rich in oxygen and enters through the hepatic artery. Each lobule (Figure 25-6) has a central vein, which collects the mixture of blood from the portal vein and hepatic artery and channels blood to the lobular veins, which empty into the hepatic vein and then into the inferior vena cava. Surgical repair can be complicated after trauma to the liver because of the rich vascular supply. Uncontrolled hemorrhage is the primary cause of early death after liver trauma.
Hepatocytes produce bile, which is essential to the digestion of fats. Bile flows from the hepatic cells into bile canaliculi between the cells toward the periphery of the lobule and empties into the interlobular bile ducts of the hepatic triad. The ducts join, forming the common hepatic duct, which allows bile to flow into the gallbladder. The gallbladder lies on the inferior surface of the liver. Its duct, the cystic duct, meets with the hepatic duct to form the common bile duct, which drains through the head of the pancreas into the duodenum (see Figure 25-6).
SPLEEN
The spleen is a lymphoid organ with various functions including defense, hematopoiesis, and red blood cell (RBC) and platelet destruction; it also serves as a reservoir for blood. Macrophages line the spleen and break apart hemoglobin molecules from the destroyed RBCs, salvaging the iron and globin content and returning them to the bloodstream for storage in the bone marrow and liver.5
The total circulation of the spleen is estimated at 250 ml/min, with a normal volume of approximately 350 ml.5 This is an impressive blood volume considering that the average weight of the spleen is 150 g. The spleen’s volume can be reduced to 200 ml very quickly after sympathetic stimulation, which causes constriction of the smooth muscle capsule. This response to stress can be a result of hemorrhage.5
The spleen is an elongated ovoid body located in the LUQ of the abdomen. It lies beneath the diaphragm, to the left of the stomach, and in immediate proximity to the tail of the pancreas, the colon, and the left kidney. It is in close proximity to ribs 7 through 10, which makes it vulnerable to injury when ribs are fractured.
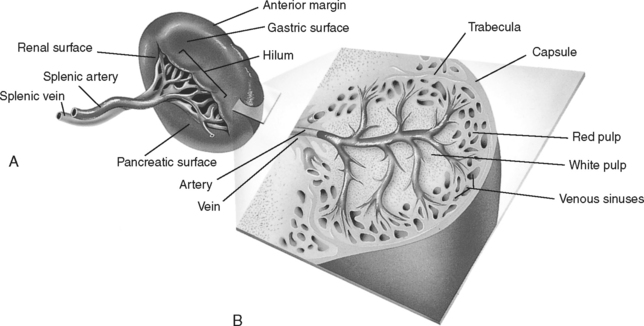
The spleen’s blood supply is from the splenic artery, which enters at the hilum and divides into five or six branches before entering splenic pulp (Figure 25-7). The splenic vein originates outside the hilum and courses along the dorsal pancreatic surface to join the superior mesenteric vein, forming the portal vein. The vascular nature of the spleen makes it a ready source for profuse bleeding into the peritoneal cavity after injury.
The splenic capsule, 1 to 2 mm thick, encloses the splenic pulp. Lymphoid tissue lies throughout the pulp and is responsible for filtration. The blood supply to the pulp is from arterioles off a central artery. The blood collects in a venous sinus and then moves to trabecular veins coursing to the main splenic veins and finally to the portal circulation (Figure 25-7, B). Arterial blood travels to venous sinuses through splenic cords (connective tissue between sinuses) and “sieves” RBCs, destroying many in the process. The spleen’s sieving process promotes it as a primary defense organ to remove microorganisms from the blood and destroy them by phagocytosis.
PANCREAS
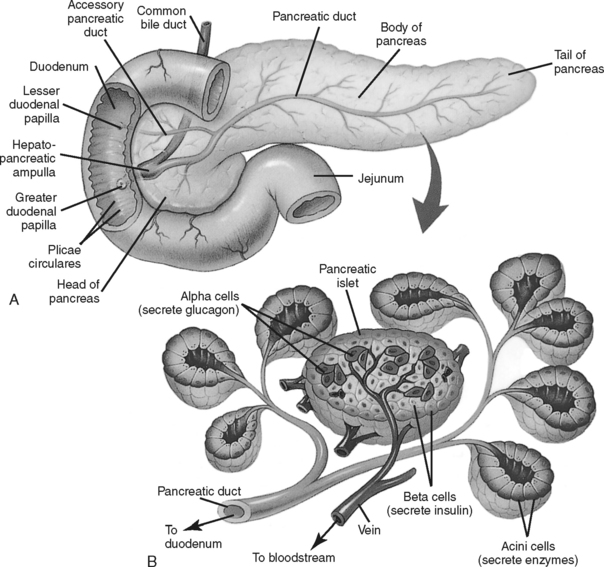
The pancreas is composed of both exocrine and endocrine glandular tissue. The exocrine pancreas secretes enzymes that digest protein, carbohydrates, and fats. These enzymes include trypsin, chymotrypsin, carboxypeptidase, α-amylase, and lipase. The endocrine pancreas produces two hormones: glucagon from the α cells and insulin from the β cells (Figure 25-8). These hormones facilitate the formation and cellular uptake of glucose.
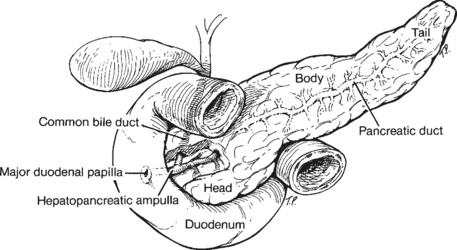
The pancreas lies at the level of the first lumbar vertebra against the posterior abdominal wall. It extends from the C-loop of the duodenum to the hilum of the spleen. A blunt trauma episode can force the pancreas against the vertebral column and may rupture it. The pancreas is divided into lobules that empty into the main pancreatic duct, which passes through the tail, body, neck, and head of the pancreas, emptying into the duodenum at the ampulla of Vater in conjunction with the common bile duct (see Figure 25-8, A). An accessory duct empties into the duodenum from the head of the pancreas. Rupture of the pancreas frequently tears its ductal system, allowing pancreatic juice (rich in digestive enzymes) to invade pancreatic tissue and the peritoneum.
Blood is supplied by the splenic artery and vein and the superior mesenteric artery and vein. Venous drainage from the body and tail of the pancreas occurs through the splenic vein to the portal vein; the head empties directly into the portal vein.
SMALL INTESTINE
The 21 to 23 feet of small intestine are divided into duodenum, jejunum, and ileum (Figure 25-9). The major functions are digestion of food and absorption of nutrients and water for the body. The blood supply is from the superior mesenteric artery. Venous drainage is to the portal vein through the superior mesenteric vein.
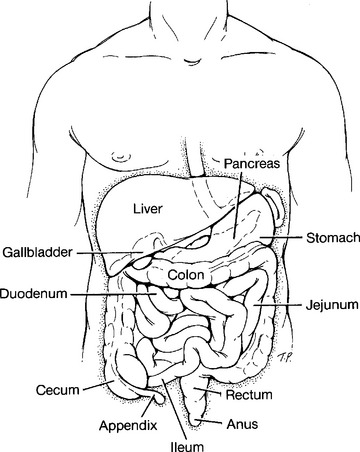
FIGURE 25-9 The small intestine: duodenum, jejunum, and ilium in relationship to other abdominal structures.
Duodenum
Most digestion and absorption occur within the duodenum. The duodenum, the first part of the small intestine, is a C-shaped loop approximately 25 cm long molded around the head of the pancreas (Figure 25-10). Beginning at the pyloric valve junction, the duodenum receives the highly acidic chyme from the stomach and fluids, enzymes, and electrolytes from the biliary and pancreatic ducts.
LARGE INTESTINE
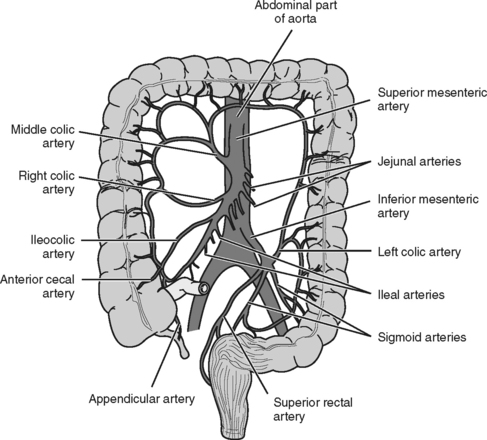
The cecum, colon, and rectum constitute the large intestine. The colon is divided into ascending, transverse, descending, and sigmoid segments (Figure 25-11). The ileum joins the large intestine at the junction of the cecum and ascending colon. The ileocecal valve permits slow movement of intestinal contents through the cecum and colon. The cecum and ascending colon are continuous from the ileum and rise to the undersurface of the right lobe of the liver, bending to the left at the hepatic flexure and becoming the transverse segment. This segment continues across to the splenic flexure (anterior to the left kidney) and then turns downward to become the descending colon. The sigmoid colon, the S-shaped segment, courses from the left iliac fossa to the pelvic cavity, becoming the rectum and terminating at the anal canal. The rectum forms the last 17 to 20 cm of the intestinal structures. The final inch is called the anal canal, and its opening is the anus. The anus is controlled by two sphincter muscles, which are closed except during defecation.
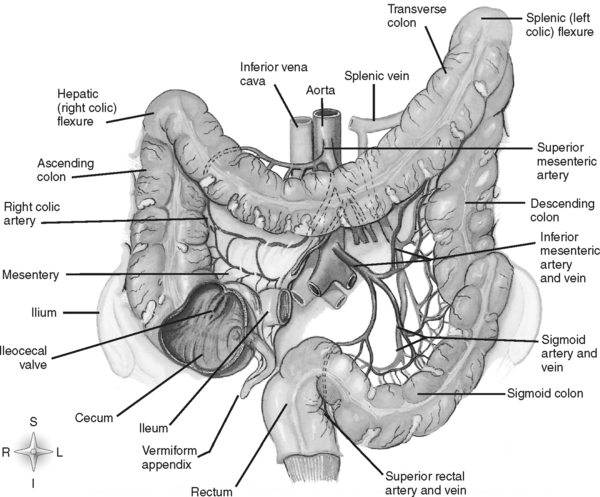
FIGURE 25-11 Divisions of the large intestine.
(From Thibodeau GA, Patton KT: Anatomy and physiology, 4th ed, St. Louis, 1999, Mosby, p 747.)
The blood supply to the colon and rectum is predominantly from the superior and inferior mesenteric arteries arising from the abdominal aorta (Figure 25-12). Blood from the large intestine drains through the portal vein to sinusoids in the liver.
ABDOMINAL VASCULAR SYSTEM
Arterial Supply
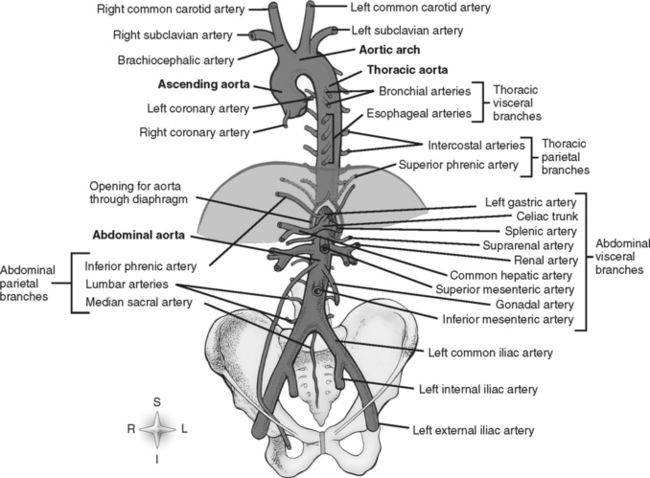
The descending aorta passes through the diaphragm at the T12-L1 level to become the abdominal aorta. At the L4 level the aorta bifurcates into the two common iliac arteries. It further divides into external and internal iliac arteries. Finally, the external iliac becomes the common femoral artery (Figure 25-13).
Venous Drainage
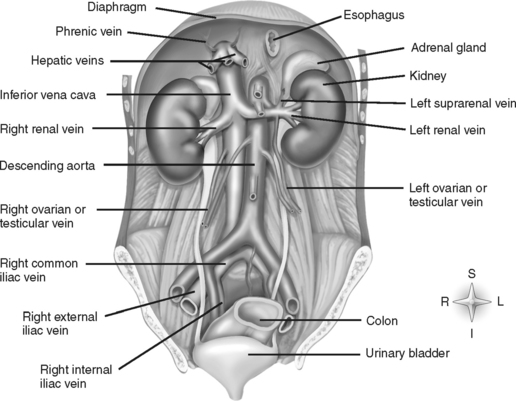
Other abdominal venous flow (Figure 25-14) originates in the external iliac veins in the inguinal ligament, which are joined by internal iliac veins to form the common iliac veins, which become the inferior vena cava at the sacral promontory. The renal veins join the inferior vena cava at the L2 level. Other smaller veins join the inferior vena cava as it passes to the superior margin of the liver. Much of the inferior vena cava lies in close proximity to the aorta, making injury to one vessel likely to affect the other.
MECHANISM OF INJURY
The mechanism of injury and forces involved direct attention toward certain organ involvement and should heighten a clinician’s suspicion regarding certain injuries. Blunt injury from a motor vehicle crash results from a compression or crushing mechanism and involves three collisions. In the first collision the motor vehicle hits a stationary object. For example, a frontal impact may crush the driver’s compartment, causing direct injury to the driver or passengers. The second collision occurs when the victim hits internal parts of the vehicle, including the windshield, steering wheel, or dashboard. The third collision involves the supporting structures of the body (e.g., skull, ribs, spine, pelvis) and movable organs (e.g., brain, heart, liver, intestines). As energy is loaded onto the body, internal forces (e.g., stress and strain) are exerted within the body as the dimensions of body tissues change. These forces can be further classified as tensile (stretch), shearing (opposing forces across an object), or compressive (crush). The types of injuries that result from these forces include spleen or liver rupture, comminuted bone fractures, and tearing of the aorta.
Penetrating trauma may occur from a stabbing, impalement, or missile event. The size, shape, and length of the stabbing instrument help to estimate intra-abdominal damage. Management is frequently dictated by the degree of penetration into the peritoneal cavity. Impalement injuries are a dirty form of stab wound that result in high mortality rates as a result of bacterial contamination and multiple organ involvement (Figure 25-15).

FIGURE 25-15 Impalement event. Young man impaled by wooden fence rail, which entered the abdomen through the peritoneum.
Missile injuries are more difficult to evaluate. Mortality rates depend on major vessel disruption and multiple organ involvement. The terminal velocity, or the amount of energy imparted to the tissue by the missile, often determines the extent of injury. The incidence of significant abdominal injury related to firearms ranges from 68% to 94%.6 The wide variation in percentage may be due to differences in how the wounds were categorized. The magnitude of entrance and exit wounds may bear little relationship to the degree of damage or the course of destruction caused by a bullet. Bullets may ricochet off organs or bones, roll or move throughout the body, or embolize through the vessels. Organs in proximity to the GSW may be injured by a blast effect. Quick evaluation of the situation is necessary because hemorrhage and hollow viscus perforation resulting in chemical and bacterial peritonitis are major problems in this type of abdominal trauma. The extent of tissue destruction varies depending on velocity, type of weapon or bullet, and individual tissue characteristics; therefore, abdominal wounds and their complications have a wide range of presentations.
ABDOMINAL ASSESSMENT
A brief systematic secondary survey is the next step in the resuscitation phase. A head-to-toe assessment is completed to identify all injuries. During this process the nurse and various other team members are simultaneously assessing, providing interventions, and reassessing the patient. The secondary survey includes obtaining a complete set of vital signs, ordering laboratory studies, placing a gastric tube and urinary catheter, performing a complete neurologic examination, and obtaining more information about the patient. Diagnostic testing can occur simultaneously during the primary and secondary survey, including bedside ultrasonography (US), computed tomography (CT), diagnostic peritoneal lavage (DPL), and chest radiograph.
AUSCULTATION
Auscultation is often the most difficult part of the abdominal examination during resuscitative or critical care efforts simply because of the noise created by team members performing lifesaving procedures. The presence or absence of bowel sounds on initial examination is nonspecific information in patients with suspected abdominal injury.7 While auscultating in all four quadrants, the nurse should be alert for the presence of bowel sounds in unlikely locations, such as the chest cavity, which may indicate a diaphragmatic tear. In serial auscultation, diminished or absent bowel sounds may indicate an ileus or peritonitis. The nurse should listen for bruits, especially over the renal arteries, abdominal aorta, and iliac arteries, which may indicate partially obstructed arterial blood flow.
PERCUSSION
Dullness throughout the four quadrants indicates free fluid in the abdomen. Fixed areas of dullness (Ballance’s sign) in the LUQ may suggest a subcapsular or extracapsular hematoma of the spleen or flank. Dullness that does not change with position suggests the presence of retroperitoneal hematoma. Tympanic percussion may represent air in the abdominal cavity, indicative of perforated viscus. A diaphragmatic tear or hemothorax may be suspected if a dull sound is elicited over the otherwise tympanic thoracic space.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree