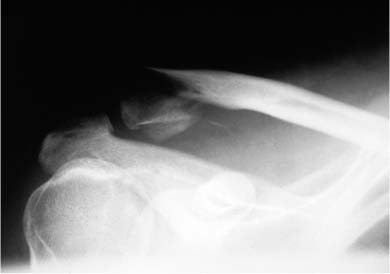
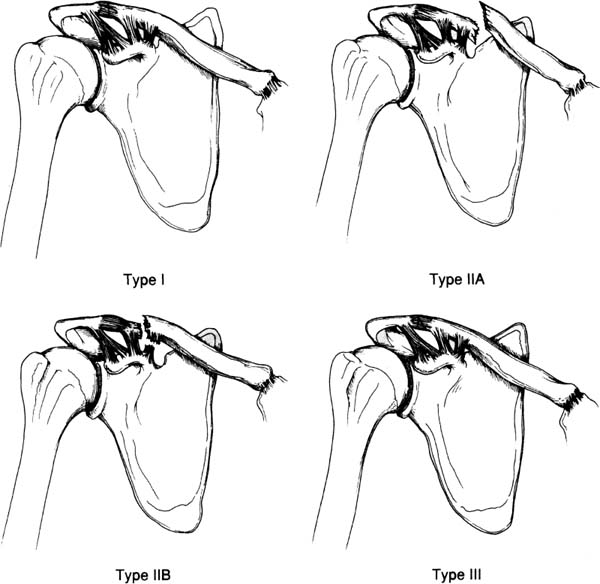
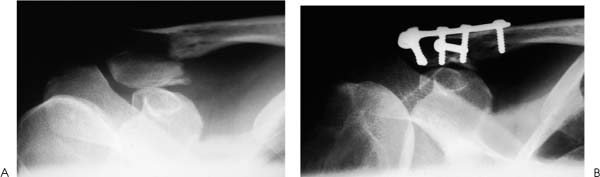
Case 9 A 27-year-old woman presents 2 days after being involved in a motor vehicle accident. She complains primarily of right shoulder pain and deformity. She denies any other injuries, although she states that the motor vehicle accident was a high-speed crash. Passive forward flexion of 90 degrees is possible, after which time severe pain in the shoulder occurs. Passive external rotation is normal. Rotator cuff strength is 4/5. Tenderness and moderate swelling are present along the superior aspect of the shoulder and a superficial abrasion is present there as well. A prominence in the area of the distal clavicle is seen, but no full-thickness skin defects or lacerations are present. She is neurovascularly intact. Figure 9–1. An anteroposterior (AP) X-ray of the affected extremity. 1. Clavicle fracture 2. Glenohumeral joint 3. Shoulder contusion 4. Proximal humerus fracture 5. Acromioclavicular joint dislocation An anteroposterior (AP) radiograph is shown (Fig. 9–1). Distal Clavicular Fracture. Distal clavicle fracture was suspected based on the cosmetic deformity present. Another possibility is an acromioclavicular joint separation, but clinically deformity is present over the lateral portion of the clavicular shaft instead of at the acromioclavicular joint. A shoulder dislocation can demonstrate significant shoulder asymmetry based on the relative prominence of the acromion, but no such acromial irregularity was appreciated. Radiographs confirm the distal nature of the clavicular shaft fracture and the displacement that is present. Lateral third clavicle fractures often result from higher levels of energy transfer and trauma than do middle third fractures of the clavicle. When a lateral third clavicle fracture is identified, particular attention to surrounding soft tissue and bony structures may demonstrate additional fractures and/or soft tissue injury. For example, rib fractures and scapular fractures are sometimes seen. Also, the possibility of neurovascular injury is greater, making careful neurovascular examination important. Clavicle fractures are grouped according to their position on the clavicle. Middle third clavicle fractures are considered group I fractures. Group II fractures constitute fractures of the distal third, and these fractures can be further subtyped according to their position in the distal third of the shaft. Group III fractures constitute fractures of the proximal one third of the clavicle. Group I fractures, or fracture of the middle third, are the most common fractures seen in adults and children. They generally occur at a point in which the clavicle changes to a flattened cross section. This area of the clavicle is otherwise unsecured, as opposed to the more proximal and distal segments, which are mechanically supported by the ligamentous structures and muscular attachments at each end. Middle third (group I) fractures account for approximately 80% of all clavicle fractures. Group III (medial third) fractures constitute approximately 5% of clavicle fractures. Group II fractures account for 15% of all clavicle fractures and are subtyped according to their location relative to the coracoclavicular ligaments and the articular surface of the distal clavicle. Neer emphasized the importance of subdividing this fracture according to its location and articular extension. Type I distal third fractures occur lateral to the coracoclavicular ligaments but do no extend into the acromioclavicular joint articulation. Because the ligaments remain intact, there is little displacement of the fracture (Fig. 9–2). Type II distal third fractures are interligamentous and cause the coracoclavicular ligaments to detach from the medial fragment. Type III fractures extend into the articular surface of the distal clavicle. The treatment of distal third clavicular fractures depends on a number of factors. The degree of displacement and the location of the fracture site relative to the coracoclavicular ligaments are important in deciding on treatment. Minimally displaced distal third fractures can be safely treated nonoperatively with the expectation of bony union and excellent functional recovery. However, when significant displacement is seen, particularly in type II-A and type II-B fractures (Fig. 9–2), with loss of the suspensory effect that the coracoclavicular ligaments provide, surgical treatment is a consideration. Also, with displaced intraarticular distal third fractures (type III), surgical intervention may be required. In type II distal clavicle fractures, the coracoclavicular ligaments are detached from the medial segment. Both the conoid and trapezoid ligaments may be attached to the distal fragment (II-A) (Fig. 9–2), or the conoid ligament may be ruptured while the trapezoid ligament remains attached to the distal fragment (II-B) (Fig. 9–2). Four forces act on this distal third clavicular fracture that contribute to displacement at the fracture site: (1) the weight of the shoulder girdle and arm cause downward displacement of the lateral clavicular fracture fragment when the patient is in the upright position; (2) the pectoralis major and minor muscles, along with the latissimus dorsi, draw the distal segment downward and medially, causing overriding and displacement; (3) the scapula may rotate the distal segment as the arm is moved; and (4) the trapezius muscle tends to draw the medial clavicular fracture fragment superiorly and posteriorly, displacing the fracture site as well. Figure 9–2. Types of distal clavicle fractures. A type I distal clavicle fracture occurs lateral to the coracoclavicular ligaments, and little displacement of the fracture fragments is seen. A type II-A fracture occurs medial to the coracoclavicular ligaments, leading to significant displacement at the fracture site. Type II-B fractures occur within the coracoclavicular ligaments. Type III distal third clavicle fractures result in intraarticular extension, but frequently occur without significant ligament disruption. Type II fractures of the distal third of the clavicle occur medial to (type II-A) or within (type II-B) the coracoclavicular ligaments. Displacement of the fragments is accentuated by the downward displacement of the arm and shoulder girdle as a result of the loss of the suspensory effect that the coracoclavicular ligaments provide when attached to the medial fracture fragment. As a result, nonunion of type II distal third fractures occurs with increased frequency. Type III distal third fractures present with intraarticular extension. However, significant displacement is not usually seen, nor is significant ligamentous disruption. Because there is often little or no displacement, these fractures are frequently misdiagnosed as acromioclavicular joint injuries. Type III fractures involve the medial third of the clavicle. These fractures constitute about 5% of all clavicle fractures and are not usually very displaced. (© 1997 American Academy of Orthopaedic Surgeons. Reprinted from the Journal of the American Academy of Orthopaedic Surgeons, Volume 5(1), p. 17, with permission.) The patient is placed in the beach chair position for surgical stabilization of the clavicle. The upper extremity and anterior chest are sterilely prepped and draped with the arm draped free. An incision parallel to the clavicle is made and dissection of the subcutaneous tissues accomplished. Care is taken to minimize soft tissue stripping. The fracture site is identified and an AO reconstruction plate, or occasionally a T plate, is used (Fig. 9–3). A T plate is preferred by the authors because of its low profile superiorly and because it maximizes the ability to place screws into the lateral fracture fragment. A lag screw is routinely drilled across the fracture site through the plate to maximize stability of the internal fixation. When inadequate bone exists laterally to support a plate and screw construct, an intramedullary device is used. With the patient in the beach chair position, a small vertical incision can be made at the fracture site. The deltotrapezial interval is split in line with the clavicle and the fracture site is exposed. A Steinmann pin or Knowles pin can be drilled from the posterolateral aspect of the acromion to emerge from the medullary canal of the lateral fracture fragment. The fracture can then be reduced and the Knowles pin advanced into the medullary canal of the medial clavicular fracture fragment. The straight pin passed through the curved clavicle serves to enhance stability because of the three-point fixation achieved. If the Knowles pin penetrates the anterior cortex of the clavicle, it can be cut off so as not to be prominent under the skin (Fig. 9–4). Alternatively, a Steinmann pin can be drilled in a retrograde fashion out the lateral fracture fragment, and then advanced antegrade into the medullary canal of the medial fragment. The advantage of the Knowles pin is that it can be removed more easily because of the more prominent head. Figure 9–3. Preoperative (A) and postoperative (B) radiographs of the displaced distal third clavicle fracture in the patient presented here. PEARLS • Use of a low-profile AO T plate designed for wrist fractures will maximize the ability to secure the lateral fragment with screws. • When a Knowles pin is used to secure intramedullary fixation, a technical tip to aid in placement involves the retrograde drilling of a Steinmann pin or Kirschner wire out the lateral fracture fragment and then advancing a Knowles pin ante-grade while removing the Steinmann pin.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree