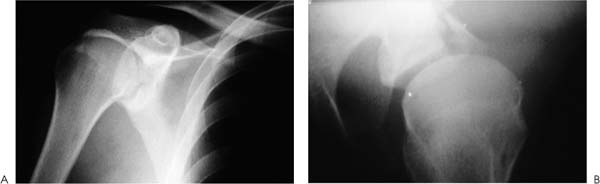
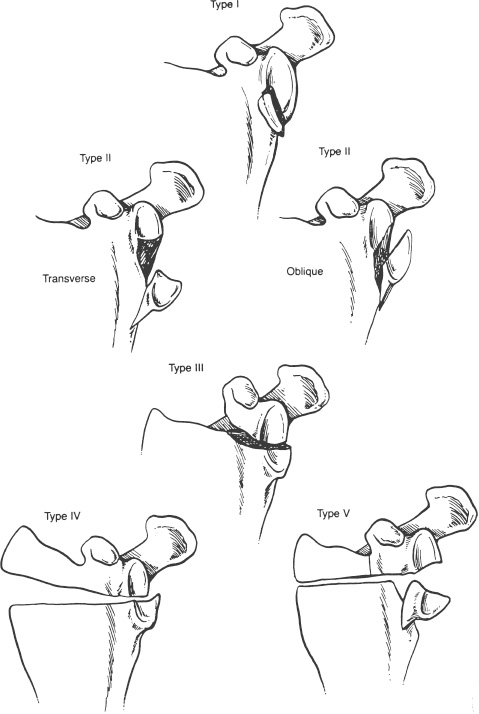
Case 6 An 18-year-old high school athlete presents several hours after sustaining an anterior shoulder dislocation, which was reduced by his trainer on the field. He denies any previous injury to or dislocation of the shoulder. He is neurovascularly intact and complains only of pain in the shoulder. Range of motion is limited because of pain and generalized weakness about the shoulder. Translation testing demonstrates marked anterior shoulder instability, and the patient spontaneously dislocates while attempting to sit up from the examining table. Figure 6–1. Anteroposterior (AP) (A) and axillary (B) radiographs of the shoulder in this patient. 1. Anterior shoulder dislocation 2. Fracture-dislocation of the proximal humerus 3. Anterior glenoid rim fracture with dislocation An anteroposterior (AP) and axillary view of the shoulder were obtained (Fig. 6–1). Anterior Glenoid Rim Fracture. An anterior shoulder dislocation is diagnosed based on both the history and physical examination. The spontaneous dislocation that occurred in the examining room suggests a high degree of instability. Radiographs show a concentrically reduced glenohumeral joint, but also demonstrate an anterior glenoid rim fracture. This rim fracture is presumably contributing to the instability that is present. Large glenoid rim fractures are generally evident on routine radiographs. However, an accurate assessment of the size of the fragment relative to the articulating surface of the glenoid is difficult to determine with routine radiographs. Computed tomography (CT) scanning can help to assess the size and displacement of the rim fracture. Figure 6–2. Ideberg’s classification of intraarticular fractures of the glenoid. (From Rockwood C Jr., et al. Fractures in Adults. Philadelphia: Lippincott-Raven Publishers, 1996, p. 1176, Fig. 18–21. With permission of Lippincott-Raven Publishers.) The treatment of glenoid rim fractures depends on a number of factors, including the articular step-off and the instability that is present following this injury. Articular step-off of 5 mm or more, particularly when associated with recurrent instability, is an indication for surgical treatment. Intraarticular fractures of the glenoid are classified into five types (Fig. 6–2). Glenoid rim fractures are classified as type 1 intraarticular glenoid fractures. Fracture fixation, when required, can generally be performed through an anterior or posterior approach, depending on the respective rim fracture that is present. Surgery is indicated if a glenoid rim fracture results in persistent subluxation of the humeral head or if the reduction is unstable. Instability can be anticipated if the fracture is displaced by 10 mm or more and if at least 25% of the anterior aspect of the glenoid cavity or one third of the posterior aspect of the cavity is involved. The goal of operative intervention is to reestablish osseous stability, thereby preventing chronic glenohumeral instability. • CT scanning should be performed on any glenoid rim fracture where displacement and size cannot be accurately determined on regular radiographs. This will provide valuable insights into the fracture orientation and can be critical in deciding the best course of treatment. • AO small fragment cannulated screws provide for strong, effective reapproximation of the glenoid rim fracture. They minimize the number of holes required to achieve fixation of this small bony fragment prone to comminution.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree