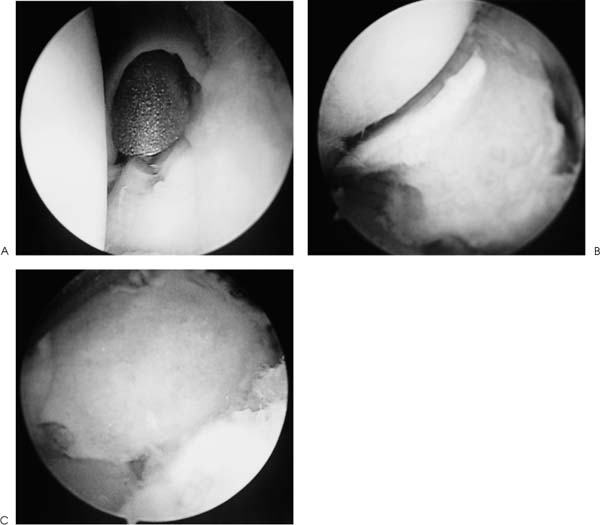
Case 49 A 61-year-old healthy woman presents 6 months following an injury to her elbow during which she reports falling onto her outstretched hand. She says that she was treated with immediate limited-motion exercises that were progressed to activities as tolerated over a 1-month period of time. She reports continued pain and crepitation in the elbow and persistent loss of motion. She denies any catching or locking of the elbow. No numbness or weakness of the upper extremity was reported. Range of motion demonstrates a 25-degree extension lag and elbow flexion of 120 degrees. She has supination of 40 degrees and pronation of 20 degrees. Her stability is normal on examination, but she has crepitation to passive supination and pronation in the area of the radiocapitellar joint. She also has a positive compression rotation test for pain. This test is accomplished by applying a longitudinal compression force on the forearm while passively supinating and pronating the forearm. The patient demonstrates no tenderness over the lateral epicondyle or just distal to it, although palpation in the area of the radiocapitellar joint and in the posterolateral gutter causes mild pain. Figure 49–1. Anteroposterior (AP) (A) and lateral (B) radiographs of the elbow. 1. Posterolateral rotatory instability of the elbow 2. Radiocapitellar arthritis 3. Ulnohumeral joint arthritis 4. Posterior interosseous nerve compression 5. Lateral epicondylitis Anteroposterior (AP) and lateral radiographs are obtained (Fig. 49–1). Radiocapitellar Arthritis. Symptomatic radiocapitellar arthritis was identified based on the patient’s history, positive physical finding, and the radiographic evidence of radiocapitellar arthritis. The previous radial head fracture and subsequent mild malunion probably accounted for the progressive articular degeneration and the persistence of symptoms following the injury. The patient had no tenderness over the lateral epicondyle or immediately distal to it, as would be expected in lateral epicondylitis. Also, the patient did not exhibit posterolateral rotatory instability of the elbow. There was no evidence to suggest posterior subluxation of the radial head on the capitellum, either clinically or radiographically. Radiocapitellar arthritis may occur in isolation following a radial head fracture. However, it is more often seen in conjunction with global elbow degenerative changes or systemic illness. Loose bodies can cause progressive degeneration of the elbow as well. Systemic illness, such as rheumatoid arthritis, can lead to progressive radiocapitellar degeneration with increasing symptoms. No evidence of systemic illness was seen in this patient. Tenderness in the posterolateral gutter could simply be secondary to a local reactive and inflammatory process, or it could be the result of an as yet radiographically unrecognizable arthritis. A symptomatic posterolateral elbow plica could also be the cause of posterolateral elbow joint pain. Chronic inflammatory changes can cause thickening and fibrosis of this plica, leading to painful popping, tenderness, and swelling. Management of patients with radiocapitellar arthritis depends on the degree of symptoms, the limitation of motion, and any systemic illnesses contributing to the problem. Radiocapitellar arthritis resulting from a traumatic injury such as a radial head fracture may respond to a trial of nonsteroidal antiinflammatory medications along with an organized exercise program. Also, while an intraarticular injection of corticosteroid may reduce inflammation and synovitis, it rarely leads to permanent improvement in elbow motion and symptoms. Patients with radio-capitellar degeneration due to an underlying systemic illness, such as rheumatoid arthritis, present a different clinical problem. Elbow synovectomy and debridement with or without radial head excision has proven to be an effective method of managing rheumatoid arthritis. Several classification schemes for rheumatoid arthritis have been suggested. The Hospital for Special Surgery classification of rheumatoid arthritis defines the degree of joint involvement by clinical and radiographic criteria. Grade I disease indicates only a mild to moderate degree of synovitis without radiographic changes. Grade I changes are managed with aspirin or nonsteroidal antiinflammatory medications. Grade II disease indicates a recalcitrant synovitis that cannot generally be managed with aspirin. Intermittent arthrocentesis and corticosteroid intraarticular injections are required. The radiographs show minimal architectural changes. Grade IIIA disease indicates an unremitting, active synovitis with variable signs of joint articular damage. Grade IIIB disease exists when extensive articular damage, as well as loss of subchondral bone and ligamentous stability, occurs. Grade IV disease is characterized by gross destruction and loss of normal architectural landmarks. Gross instability is generally seen with grade IV disease. Rheumatoid arthritis patients with grade II disease can be effectively treated with synovectomy. The arthroscope is an excellent tool that allows for complete elbow synovectomy. Likewise, in cases where the synovitic reaction is accompanied by symptomatic radiocapitellar joint degeneration, the arthroscope can be used to perform a minimally invasive radial head excision. Elbow synovectomy and debridement have proven to be an effective method of managing patients with grade II involvement. In these patients, there is an uncontrolled, painful synovitis of the elbow joint, leading to pain and limitation of function. These patients also often demonstrate symptoms attributable to radiocapitellar joint degeneration. There is generally no extensive joint or ligamentous destruction. Synovectomy is preferred in the treatment of grade II disease and should be performed early, before there is gross joint destruction. Although a limited, subtotal synovectomy with removal of the radial head can be performed through a lateral approach to the elbow joint, arthroscopic synovectomy, accompanied by arthroscopic radial head excision, is preferred by the authors. Neither the open nor arthroscopic technique can remove all of the synovium, but this subtotal synovectomy has proven extremely useful. The indications for arthroscopic radial head excision include the following: (1) primary degenerative changes; (2) posttraumatic radiocapitellar joint changes without significant deformity of the radial head and/or radiocapitellar joint; (3) in conjunction with arthroscopic synovectomy when symptomatic radiocapitellar joint symptoms exist, such as in rheumatoid arthritis, and (4) as a treatment alternative in patients with chronic symptomatology associated with osteochondritis dissecans of the capitellum after bone growth maturity. Relative contraindications to arthroscopic radial head excision include (1) patients with moderate to severe radial head deformity following fracture malunion, particularly when accompanied by soft tissue elbow contractures, because of the extreme proximity of the radial nerve to this malunited radial head fracture; and (2) anatomic landmarks that are not adequately visualized or insufficient technical expertise to use the arthroscopic technique. Patients are placed in the prone or lateral decubitus position, as these positions allow excellent access to the posterior elbow joint. Good access to the posterolateral gutter is imperative to completing an arthroscopic radial head excision. Arthroscopic radial head excision should be carried out only after a thorough arthroscopic evaluation of the entire anterior and posterior elbow joint. Patients with radiocapitellar joint changes sufficient to require radial head excision generally have accompanying intraarticular pathology. Such pathology can include degenerative changes in the ulnohumeral joint with coronoid process and olecranon process osteophytes, along with posterolateral and posteromedial gutter osteophytes. Loose bodies are commonly seen in this clinical situation and should be extensively searched for, both in the anterior and posterior compartments. Also, patients with symptomatic radiocapitellar joint degenerative changes sometimes develop a symptomatic posterolateral plica. This normal thickening of the posterolateral capsule sometimes becomes thickened and fibrosed in the presence of long-standing inflammatory changes in and around the radiocapitellar joint. This thickened and fibrotic plica can create symptoms of its own by impingement on the posterolateral bony structures through a range of motion. This can result in pain, swelling, and tenderness in the area of the posterolateral elbow joint, along with popping, clicking, and catching complaints. Recurrent irritation of the plica by impingement on the bony structures only serves to create a vicious cycle of injury, inflammation, and fibrosis. If the patient demonstrates findings compatible with a symptomatic posterolateral plica, arthroscopic excision and release of the plica can be accomplished at the same operative intervention. Following placement of the patient in the prone or lateral decubitus position, a sterile prep and drape is carried out. A tourniquet is placed on the arm prior to prepping and draping, but it is not routinely inflated unless untoward bleeding is encountered. The arthroscopic procedure always starts with insufflation of the joint through the direct lateral portal. Approximately 25 cc is generally instilled, but care is taken not to overdistend the joint, as capsular rupture can occur quite easily. A proximal anterolateral portal, described by Field and colleagues (1994), is initially positioned 2 cm proximal and 1 cm anterior to the lateral epicondyle. All portals are established by pulling the skin under a knife and using a hemostat to dissect down to the level of the capsule. The arthroscope is inserted, and the coronoid, trochlea, and coronoid fossa are evaluated. Instrumentation is performed via a proximal anteromedial portal, which can be placed through either an inside-out or outside-in technique. Coronoid spurs are excised and the coronoid fossa is deepened, as necessary, using a motorized burr. The anterolateral portal allows for assessment of valgus instability through use of the arthroscopic valgus instability test. In patients with valgus instability on clinical examination, or the possibility of it, the arthroscopic valgus instability test provides an accurate measure of medial ulnar collateral ligament competency. This test, performed by placing a valgus stress on the elbow while it is flexed approximately 70 degrees, allows for direct visualization of ulnohumeral joint opening if medial ulnar collateral ligament disruption or insufficiency is present. An opening of 1 mm or more confirms complete disruption of the medial ulnar collateral ligament. Anterior compartment evaluation is completed by switching the arthroscope to the anteromedial portal. The radial head and capitellum are carefully examined. Flexing and extending the elbow allows for a complete capitellar evaluation. Pronation and supination allow for adequate evaluation of the radial head. Instrumentation is passed through the anterolateral portal and radial head and capitellar spurs are excised. If arthroscopic radial head excision is to be performed, then pronation and supination are simply continued until all of the exposed radial head has been excised via the proximal anterolateral portal. Generally, some residual radial head persists, and radial head excision is completed by placing the arthroscopic shaver through the soft spot portal while continuing to visualize through the anteromedial portal. The remaining radial head can then be excised from posterior to anterior using a “cutting block” technique with medial to lateral sweeps of the arthroscopic shaver. The forearm is pronated and supinated to ensure complete resection of the radial head (Fig. 49–2). The resection is continued until full pronation and supination can be achieved and no radiocapitellar impingement occurs through a normal flexion and extension arc of motion (Fig. 49–3). Figure 49–2. Excision of an arthritic radial head. (A) View from anteriomedial portal prior to excision. (B) Radial head excision partially completed through anterolateral working portal. (C) Radial head excision completed arthroscopically after the shaver has been advanced from the posterolateral soft spot portal. (See Color Plates 49–2A,B,C.) Upon completion of anterior compartment debridement and radial head excision, an evaluation of the posterior compartment is performed. An inflow cannula is maintained in the anteromedial or anterolateral portal. The arthroscope is then inserted through a proximal posterolateral portal. Evaluation of the posterolateral gutter and confirmation of adequate radial head excision can be seen through this portal site. Excision of the posterolateral plica, if present, can be accomplished by working through the soft spot portal. Also, posterolateral gutter osteophytes can be removed under direct visualization. Next, a posterocentral portal is established and debridement of the olecranon fossa, with removal of any olecranon osteophytes, can be performed. Visualization of the posterolateral and posteromedial gutters also allows for the identification and removal of any loose bodies. Full range of motion confirms the adequacy of the olecranon osteophyte excision and olecranon fossa debridement. If persistent impingement is seen in the olecranon fossa near full elbow extension, an arthroscopic ulnohumeral arthroplasty can be carried out. • Use of the minifluoroscopic unit or radiographs intraoperatively allows for confirmation of the appropriate amount of radial head excision. • In cases of radial head excision with moderate distortion of the radial head, an inside-out technique for anterolateral portal placement using a spinal needle may be beneficial in maximizing access to the radial head. This can be accomplished by first visualizing the anterolateral joint through the proximal anteromedial portal.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree