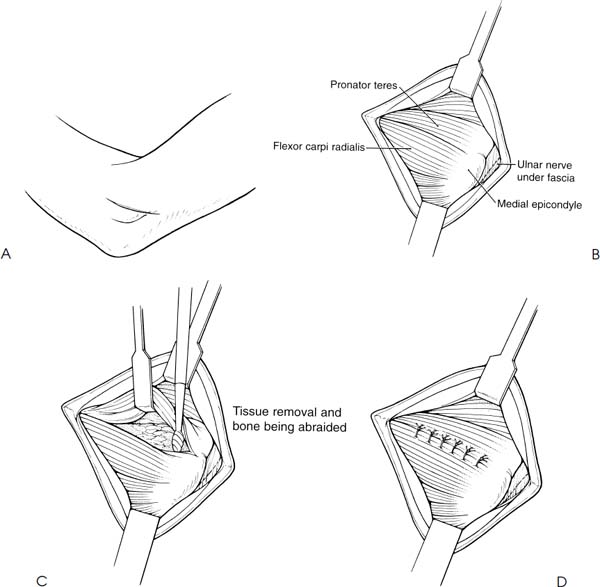
Case 44 A 40-year-old healthy, right-hand-dominant golfer presents with a 3-month history of activity-related medial elbow pain. He denies any hand numbness or weakness. There is no loss of elbow motion. This patient demonstrates a normal range of motion of the elbow, including normal supination and pronation. There is no instability to valgus, varus, or rotatory stress testing. He is neurovascularly intact and has a negative Tinel’s sign at the elbow. He does have tenderness limited to an area immediately distal to the medial epicondyle. He also complains of pain in this same general area with resisted forearm pronation. There is no atrophy along the medial elbow. No other abnormalities are identified. 1. Medial epicondylitis 2. Medial ulnar collateral ligament disruption 3. Ulnar neuritis 4. Ulnohumeral arthritis Anteroposterior (AP) and lateral radiographs of the elbow fail to reveal any obvious abnormalities. Medial Epicondylitis. Medial epicondylitis is diagnosed based primarily of the location of the pain just distal to the medial epicondyle. Patients usually complain of pain in the area of flexor-pronator tendinous origin. It is often exacerbated by participation in sports or overuse activities. Activities that cause repetitive wrist pronation are especially problematic. Achiness and stiffness in this same localized area are common symptoms as well. Just as in lateral epicondylitis, symptoms are often improved or even alleviated with rest, only to recur with resumption of these activities. Neither swelling nor edema is typical for this condition. Once the diagnosis of medial epicondylitis is made, a treatment regimen similar to that described for lateral epicondylitis is started. Flexibility and resistance exercises, emphasizing wrist flexion and forearm pronation, are carried out. Three to six sets of 10 repetitions, two to three times daily, are encouraged. Resistance to wrist flexion and pronation is provided by either the contralateral hand or by rubber tubing. These resistance exercises are then progressed as tolerated, but reduced in number and intensity if they reproduce medial elbow pain. Nonsteroidal antiinflamma-tory medications are sometimes effective in reducing symptoms. Also, while not used routinely, localized corticosteroid injections may occasionally be of therapeutic benefit. Persistent medial epicondylitis unresponsive to exercises and other measures is an indication for surgery. Restoration of the attachment of healthy tendon to the epicondyle is the goal of surgery. The authors prefer an oblique, 3-cm skin incision centered at the medial epicondyle. The incision is parallel and directly anterior to the ulnar nerve as it courses behind the epicondyle. Following dissection of the subcutaneous tissues, the medial epicondyle and flexor tendon origins are identified. A longitudinal incision aligned with the tendon fibers is made through the tendinous origins. It is centered at the point of maximal tenderness, as determined preoperatively. All pathologic tissue is then excised by extending the borders of the incision in an elliptical fashion; care should be taken not to remove or undermine remaining normal tissue. The exposed medial epicondyle is then abraded to bleeding bone to promote soft tissue healing. Occasionally, a suture anchor will be placed in this bony bed to facilitate this soft tissue reapproximation. The elliptical incision is then closed using absorbable sutures. The skin is closed in a standard fashion and a soft, compressive dressing applied (Fig. 44–1). Figure 44–1. The surgical technique for medial epicondylitis release. (A) An oblique skin incision is made. (B) A longitudinal fascial incision is made after exposing the flexor-pronator musculature. (C) The pathologic tissue is then excised, after which time the underlying bone is abraded. (D) The remaining healthy tendinous tissue is then reapproximated using absorbable sutures. • Excise all pathologic tissue in the area of the flexor-pronator tendon identified at surgery. • Identifying the area of maximum tenderness in the preoperative holding area helps to localize this site of pathologic tissue.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree