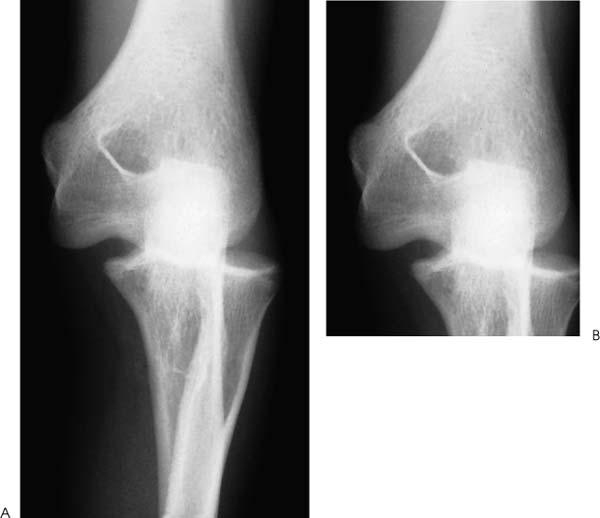
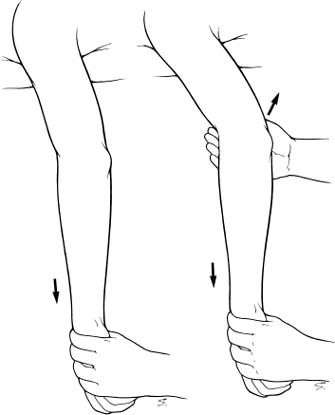
Case 38 A 19-year-old college basketball player presents to the emergency room 90 minutes after falling onto his extended arm. He complains of pain, swelling, and lack of motion of his elbow. He denies any numbness. The patient demonstrates an obvious deformity of the elbow. His olecranon process appears prominent, and his range of motion is from 70 to 85 degrees. He has limited pronation and supination. Neurovascular examinations demonstrate a 2+ radial pulse, a 2+ ulnar pulse, and normal median, ulnar, and radial nerve function. Figure 38–1. (A,B) Anteroposterior (AP) radiographs of the elbow. 1. Distal humerus fracture 2. Posterior elbow dislocation 3. Olecranon fracture Anteroposterior (AP) radiographs are obtained (Fig. 38–1). • A prereduction and postreduction assessment of neurovascular function is particularly important with elbow dislocations. Adjacent nerve injuries are common, and iatrogenic injury or entrapment of the nerves at the time of reduction is important to rule out and document. • Patients with significant valgus or posterolateral rotatory instability following reduction may benefit from a hinged elbow brace in the early postinjury period. This will allow for immediate flexion and extension exercises but will protect the collateral ligaments and prevent maximum pronation or supination, which can be detrimental during early ligament healing. Posterior Elbow Dislocation. Posterior elbow dislocation is suspected based on the clinical examination and the mechanism of injury. Radiographs confirm the diagnosis. No associated fracture of the radial head or coronoid process is appreciated. Also, the patient is neurovascularly intact. Treatment centers around an attempt at closed reduction of the posterior elbow dislocation. A thorough neurovascular examination should be performed prior to any attempt at reduction, not only to document abnormalities but also to assure that the reduction itself does not cause injury to the neurovascular structures. Many techniques of manipulation have been described for closed reduction of posterior elbow dislocations. Most employ a combination of longitudinal traction and mild distraction. Options include placing the patient prone on a stretcher, after which time 5 to 10 lb of weight is applied to the wrist. Another alternative is having the patient drape his arm over the back of a chair and apply weights in a similar fashion. Usually, 10 to 15 minutes of traction will either result in spontaneous reduction or easy reduction with gentle longitudinal traction and mild distraction (Fig. 38–2). This technique was applied in the present patient with a concentric reduction confirmed radiographically. Careful neurovascular examination should be performed after reduction to assure no deterioration in neurovascular function. Also, elbow range of motion should be assessed and stability assured through a range of motion. If marked valgus or postero-lateral rotatory instability is appreciated, postreduction restrictions may be required. Figure 38–2. Closed reduction can generally be accomplished by applying downward longitudinal force with the patient prone. A gentle distracting force at the ulnohumeral articulation is sometimes required. • The most common complication following an isolated elbow dislocation, is persistent elbow stiffness. For this reason, early or even immediate range of motion exercises are encouraged and promoted. Recurrent elbow instability is very unlikely following an isolated dislocation, but elbow stiffness is very common. • Fractures occur commonly in conjunction with an elbow dislocation, and careful scrutiny of the radiographs following reduction helps to rule out commonly associated fractures such as radial head fractures and coronoid process fractures. Also, articular cartilage injuries can occur and occasionally can be seen radio-graphically as a small sliver of bone. • If recurrent instability is to occur following an elbow dislocation, it is most likely to occur soon after the initial injury. For this reason, initial assessment of elbow stability immediately following reduction will help ensure that adequate stability is present through a full range of motion.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree