Discoid Lateral Meniscus
Examination/Imaging
 Examination may show joint line tenderness, effusion, decreased range of motion, quadriceps atrophy, bulge at the anterolateral joint line in full flexion, click and shift of the meniscus on extension, and a positive McMurray’s sign.
Examination may show joint line tenderness, effusion, decreased range of motion, quadriceps atrophy, bulge at the anterolateral joint line in full flexion, click and shift of the meniscus on extension, and a positive McMurray’s sign.
 Radiographs may show widening of the lateral joint space, cupping of the lateral tibial plateau, flattening of the lateral femoral condyle, tibial spine hypoplasia, and elevation of the fibular head.
Radiographs may show widening of the lateral joint space, cupping of the lateral tibial plateau, flattening of the lateral femoral condyle, tibial spine hypoplasia, and elevation of the fibular head.
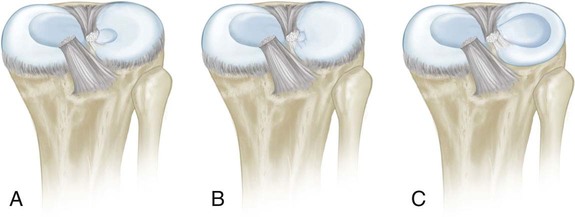
 MRI should show continuity of the meniscus between the anterior and posterior horns on ≥ 3 consecutive sagittal sections that are 5 mm thick (Fig. 1).
MRI should show continuity of the meniscus between the anterior and posterior horns on ≥ 3 consecutive sagittal sections that are 5 mm thick (Fig. 1).

 MRI should also show increased width of the meniscus at the midpoint of the anterior and posterior horns on a coronal view.
MRI should also show increased width of the meniscus at the midpoint of the anterior and posterior horns on a coronal view.
 MRI will help visualize tears and intrasubstance degeneration.
MRI will help visualize tears and intrasubstance degeneration.
Positioning
 The patient is placed in the supine position.
The patient is placed in the supine position.
 The hip is flexed and abducted, with external rotation when applying varus stress in the figure-of-4 position.
The hip is flexed and abducted, with external rotation when applying varus stress in the figure-of-4 position.
 A bolster is placed behind the knee to allow for 70–90° of flexion at rest.
A bolster is placed behind the knee to allow for 70–90° of flexion at rest.
 A tourniquet is applied and inflated after Esmarch bandaging.
A tourniquet is applied and inflated after Esmarch bandaging.
Portals/Exposures
 Standard anterior medial and lateral portals are used (Fig. 3).
Standard anterior medial and lateral portals are used (Fig. 3).

 Midpatellar medial and lateral portals are added as required (see Fig. 3).
Midpatellar medial and lateral portals are added as required (see Fig. 3).
 A posterolateral incision is made as necessary for inside-out meniscal repairs.
A posterolateral incision is made as necessary for inside-out meniscal repairs.
 An anterolateral incision is made as necessary for outside-in meniscal repairs.
An anterolateral incision is made as necessary for outside-in meniscal repairs.
Procedure
Step 1: Arthroscopic Assessment
 The surgeon must visualize the discoid meniscus and determine its extent. Figure 4 shows an incomplete discoid meniscus.
The surgeon must visualize the discoid meniscus and determine its extent. Figure 4 shows an incomplete discoid meniscus.

 An assessment is made for tears and instability of the discoid meniscus.
An assessment is made for tears and instability of the discoid meniscus.
 The surgeon should assess for chondral damage, osteochondritis dissecans lesions, and loose bodies.
The surgeon should assess for chondral damage, osteochondritis dissecans lesions, and loose bodies.
31: Discoid Lateral Meniscus