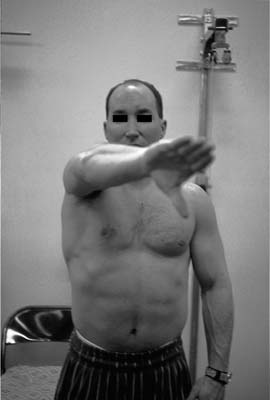
Case 26 A 56-year-old laborer presents with a several-year history of recurrent shoulder pain associated with overhead-motion activities. He denies any weakness in the shoulder or numbness in the upper extremity but has failed to respond to two subacromial steroid injections and several months of organized physical therapy directed at treatment of rotator cuff tendinitis. He reports pain not only within the shoulder but also on top of the shoulder to palpation. Active range of motion is normal and strength is normal. No atrophy, asymmetry, or scapular winging is present, and no tenderness is identified except directly over the acromioclavicular (AC) joint. The patient demonstrates a positive impingement sign and complains of pain in the area of the AC joint when a downward force on the arm is resisted by the patient when positioned in 90 degrees of forward flexion and 20 degrees of adduction. Strength and stability of the shoulder are likewise normal. Figure 26–1. An anteroposterior (AP) radiograph of the shoulder. 1. Full-thickness rotator cuff tear 2. Rotator cuff tendinitis along with a symptomatic AC joint 3. Rotator cuff tendinitis 4 Adhesive capsulitis 5. Osteoarthritis of the glenohumeral joint An anteroposterior (AP) radiograph of the shoulder is obtained (Fig. 26–1). Rotator Cuff Tendinitis and a Symptomatic Acromioclavicular Joint. This patient complains not only of chronic rotator cuff tendinitis, but also of a symptomatic AC joint. His complaints of pain on top of the shoulder along with his physical examination demonstrating tenderness in the area of the AC joint suggest AC joint arthritis. Radiographs confirm the diagnosis. Sophisticated imaging modalities are rarely indicated in the diagnosis of AC joint degeneration as clinical findings and plain radiographs will thoroughly assess the joint. The AC joint is a common site of shoulder symptoms, and resection of the distal clavicle is a reliable treatment for refractory cases. Pain originating from the AC joint can be due to a number of causes. Osteolysis of the distal clavicle can cause pain, swelling, and limited function. Likewise, degeneration of the AC joint can cause similar symptoms. Finally, injury to the AC joint that results in subluxation or intraarticular injury can cause persistent pain and disability. The proper technique and operative approach for treatment of a symptomatic AC joint depends on the etiology of the symptoms and on any other shoulder pathology that is to be treated concurrently. Patients with a symptomatic AC joint generally complain of pain over the top of the shoulder and difficulty sleeping on the affected side. The pain often radiates to the trapezius muscle and a painful AC joint can occasionally lead to trapezial spasm. Direct palpation of the AC joint will elicit tenderness and is the most reliable physical finding on clinical examination. Palpation may also demonstrate asymmetry or irregularities within the joint as well. Provocative maneuvers that load the AC joint, such as horizontal adduction of the arm (Fig. 26–2) and internal rotation of the shoulder, compress the AC joint and elicit pain. These provocative maneuvers, however, are not very specific for the joint and may overlap with other painful shoulder conditions, such as rotator cuff injury or capsular tightness. Radiographic findings associated with degenerative changes within the AC joint include marginal osteophyte formation, subchondral sclerosis, and cartilage space narrowing. Radiographic findings indicative of osteolysis are subchondral bone loss, cystic resorption of the distal clavicle, and generalized osteopenia of the distal clavicle. Radiographic findings associated with AC joint separations center on incongruency of the joint, although type I AC separations do not generally demonstrate any significant subluxation as compared with the contralateral AC joint. Although patients with symptomatic AC joints usually demonstrate the classic findings of tenderness to palpation and pain with AC joint loading, these symptoms can sometimes be obscured by other shoulder pathology. A valuable diagnostic tool to identify a symptomatic AC joint in such a clinical situation involves the injection of lidocaine into the joint. It is also valuable in helping to determine whether distal clavicle excision is indicated when other surgical procedures such as acromioplasty and/or rotator cuff repair are to be carried out. Figure 26–2. Horizontal adduction of the arm across the body compresses the acromioclavicular (AC) joint. The majority of patients with symptomatic AC joints respond to nonoperative measures. Nonsteroidal antiinflammatory medications, the judicious use of corticosteroid injections, and time will usually lead to the reduction or elimination of symptoms. Patients unresponsive to these nonoperative measures are considered for arthroscopic distal clavicle excision, and when carried out, it provides complete relief of symptoms with a high degree of success. Patients with symptomatic AC joints due to osteolysis, degenerative arthritis, or type I AC joint separations can be effectively treated with distal clavicle excision. The choice of arthroscopic approach to the distal clavicle depends on whether or not additional pathology must be treated. When an acromioplasty is required, the authors prefer the bursal approach for distal clavicle excision. In those cases where isolated distal clavicle excision is required, as for osteolysis of the distal clavicle or in some cases of type I AC joint separations, the direct superior arthroscopic approach is employed. Open resection of the distal clavicle has proven a very successful operation for AC joint pathology since first being reported by Gurd (1941) and Mumford (1941). Open resection, however, necessitates violation of the deltoid and trapezial fascial insertions onto the distal clavicle. In addition, the superior aspect of the AC capsuloligamentous complex is also incised and stripped for visualization and access to the distal clavicle. Open resection compromises the integrity of this structure, potentially destabilizing the AC joint and resulting in persistent symptoms postoperatively. In contrast, arthroscopic approaches for distal clavicle excision minimize interference with the clavicular insertions at the deltoid and trapezius muscles and thus maximize their stabilizing effect. Disruption of the superior AC ligaments is also avoided with the arthroscopic technique further enhancing postoperative stability. PEARLS • The amount of resected distal clavicle can be accurately determined by using a portal cannula of known diameter to compare with the amount of resected distal clavicle. • When the bursal approach distal clavicle excision is employed, difficulty is sometimes encountered in visualizing the superior portion of the distal clavicle during resection. Visualization can be aided by arthroscopic resection of a limited portion of the inferior and medial acromion. • Following resection of the distal clavicle arthroscopically using the bursal approach, visualization through the anterior portal will confirm that no residual superior clavicular bone has been inadvertently overlooked.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree