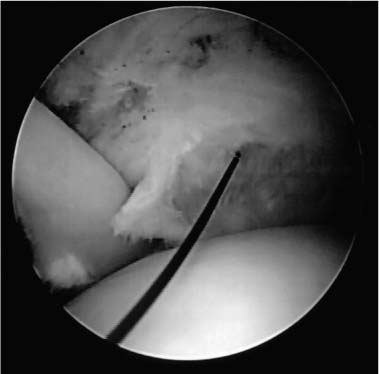
Case 21 A 62-year-old carpenter presents with a 1-year history of dominant-sided shoulder pain increased with overhead activities. He denies any specific precipitating injury. He also denies any numbness or neck symptoms. At presentation, he reports a several-month course of organized rotator cuff exercises. He has had two subacromial injections, which gave him significant but temporary relief. He also states he has decreased stamina with overhead work and must sometimes avoid strenuous activities. This patient demonstrates a normal active range of motion except for a three-vertebral-level loss of internal rotation. His passive range of motion and rotator cuff strength is normal except for 4/5 supraspinatus strength. Stability testing demonstrates no abnormalities, but the patient has a markedly positive impingement sign. Also, passive range of motion of the shoulder demonstrates palpable crepitus. 1. Full-thickness rotator cuff tear 2. Partial-thickness rotator cuff 3. Bicipital tendinitis 4. Impingement syndrome 5. Glenohumeral joint arthritis An anteroposterior (AP), axillary, and scapular Y view fail to demonstrate any abnormalities. Partial-Thickness Rotator Cuff Tear. This patient had a history and physical exam compatible with chronic, resistant impingement syndrome. His crepitus and mild weakness to supraspinatus testing suggest the possibility of a partial-thickness or a small full-thickness rotator cuff tear. However, weakness and crepitus can be due to chronic impingement syndrome without tearing of the rotator cuff tendon. This patient had failed an extensive exercise program prior to presentation. He also responded very favorably to two subacromial steroid injections. His activity level and failure to improve with these extensive nonoperative measures would suggest that surgery may be indicated. The positive impingement sign and positive impingement test in this patient make the diagnosis relatively straightforward. The one question that remains is the status of the rotator cuff. Partial-thickness rotator cuff tears are very common in patients such as the one presented here. These partial-thickness tears can either be articular surface or bursal surface tears. The majority of partial-thickness rotator cuff tears occur on the articular surface. Not uncommonly, localization of the site of an articular-sided tear at the time of arthroscopy by placement of a marking suture will also demonstrate corresponding bursal-sided degeneration. The arthroscope is an excellent tool in the evaluation of the rotator cuff, particularly as it relates to articular-sided, partial-thickness rotator cuff tears. It also allows for a thorough evaluation of the glenohumeral joint for labral pathology, biceps tendon tears, subscapularis tendon tears, and other pathologic entities. The authors always perform glenohumeral joint shoulder arthroscopy prior to acromioplasty. Shoulder arthroscopy can be performed with the patient in either the beach chair or lateral decubitus position. Following the induction of adequate regional (interscalene) anesthesia or general endotracheal anesthesia, the shoulder is sterilely prepped and draped. Standard posterior and anterosuperior portals are established and a thorough glenohumeral joint evaluation accomplished. The articular surface of the glenoid and humeral head is evaluated, as is the labrum circumferentially. Care is taken to visualize and palpate the biceps tendon to rule out superior labrum anterior and posterior (SLAP) lesions or partial-thickness biceps tendon ruptures. The biceps tendon can be pulled into the glenohumeral joint using a probe to help rule out degeneration and partial rupture of the tendon in the area of the bicipital groove. The rotator cuff tendon is then visualized. When a partial-thickness, articular-sided rotator cuff tear is identified, debridement of the frayed, tendinous tissue is accomplished. Following debridement, an assessment of the relative thickness of the cuff tear is made. This can sometimes be difficult, but probing will often help identify near-complete tears and distinguish them from relatively superficial, partial-thickness tears. Whenever a significant partial-thickness, articular surface rotator cuff tear is identified, the authors mark the site by placing a 2-0 polydioxynone suture (PDS) through the tear using a spinal needle inserted near the anterolateral acromial border. Following placement of the spinal needle through the rotator cuff defect, the PDS is passed through the needle and retrieved out the anterior portal using an arthroscopic grasper (Fig. 21–1). All cannulas are then removed and both ends of the suture are tagged together using a hemostat. Figure 21–1. A 2-0 PDS marker is seen passing through the rotator cuff defect in question. This suture marker is retrieved out the anterior cannula. (See Color Plate 21–1.) Attention is then directed to the subacromial space by visualizing through the posterior portal. An inflow cannula is placed through the anterior portal site and a lateral portal is established. A complete bursectomy is carried out, taking care not to transect the previously placed suture. Following the completion of an arthroscopic bursectomy, visualization of the bursal surface of the rotator cuff allows for identification of the suture marker and localization of the articular surface tear. Palpation in the area of the suture marker will allow for a more accurate assessment of the tear’s thickness, often identifying a small, full-thickness tear. Probing this area of the tendon can also allow for an evaluation of the quality of the tendinous tissue itself. Often the bursal surface of the rotator cuff tendon adjacent to an articular surface, partial-thickness tear will not be healthy in appearance. Such tissue quality raises concerns about the propensity of this partial-thickness tear to progress to a full-thickness tear and may lead the surgeon to choose repair over simple debridement. After the rotator cuff tendon has been evaluated and the depth of the partial-thickness tear determined, a standard arthroscopic acromioplasty is carried out. Release of the coracoacromial ligament from the anterior acromion is accomplished through the lateral portal while visualizing from the posterior portal. Portals are then switched, and while visualizing laterally, the acromial osteophytes are resected through the posterior portal. Resection of the acromion through the posterior portal is preferred by the authors because the reproducible resection allowed using the “cutting block” technique. The flat posterior acromion provides a plane to guide acromial resection, reducing the chance of excessive bone removal. However, placement of the arthroscope through the lateral portal during acromial resection limits visualization of the lateral acromial edge. For this reason, following completion of the resection, the arthroscope is again placed into the posterior portal to confirm adequate removal of lateral acromial bone. Deciding whether or not a partial-thickness rotator cuff tear requires repair depends on a number of factors. The depth of the partial-thickness tear is the most important factor to consider. In general, partial-thickness tears estimated to be greater than 50% of the cross-sectional diameter of the tendon should be repaired. This is particularly true in high demand, overhead-motion athletes or laborers, or when the remaining rotator cuff tissue is of poor quality. When repair of the partial-thickness tear is to be carried out, the technique employed depends on the nature of the tear. For example, when a significant articular-sided, partial-thickness tear is present but there is a relatively strong residual attachment to the greater tuberosity, an arthroscopic repair is preferred by the authors. This repair is accomplished by using an arthroscopic knife to incise the rotator cuff tendon in line with its fibers in the area of the tear. An arthroscopic shaver is then passed through the defect created by the incision and the greater tuberosity abraded. Next, an arthroscopic suture passing device is used to overlap the anterior and posterior edges of the tendon in the area of the longitudinal incision (Fig. 21–2). Permanent no. 2 ethibond sutures are passed to repair the incision using an arthroscopic knot-tying device. Alternatively, a mini-open approach to the rotator cuff can be easily carried out. This is accomplished by either extending the lateral portal proximally for 1 to 2 cm, or performing a separate 2-cm incision oriented in Langer’s lines centered over the rotator cuff tendon to be repaired (Fig. 21–3). Regardless of which incision is used, the deltoid is bluntly separated and a self-retaining retractor placed deep to the deltoid. The rotator cuff tear is identified by following the suture marker down to the tendon. A longitudinal incision can then be made in the tendon in a fashion identical to that accomplished arthroscopically. After a light abrasion is carried out, a suture anchor is placed in the area of the greater tuberosity. The suture limbs are then passed through their respective sides of the rotator cuff incision and tied down. This effectively “thickens” the rotator cuff tendon, as well as provides a secure approximation of the tendon to the abraded greater tuberosity. PEARLS • Most partial-thickness rotator cuff tears respond to simple debridement followed by arthroscopic acromioplasty with or without distal clavicle resection. • The value of a marking suture in the area of question on the articular side of the rotator cuff tendon cannot be overemphasized. It is a technically easy suture to place with a spinal needle, and it allows for accurate localization of the area in question on the bursal side of the rotator cuff tendon within the subacromial space. This marking suture not only allows for the recognition of adjacent bursal-sided rotator cuff tearing, but also for recognition of small otherwise difficult to localize full-thickness rotator cuff tears. However, its greatest value is in localization of the adjacent bursal surface of the cuff when no such changes are seen on the bursal surface. Localization of the articular-sided rotator cuff tear in the absence of the suture is often very difficult because of the degradation of tactile sensation with use of the arthroscopic instruments.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree